Neoadjuvant treatment in patients with pancreatic cancer has increased the efficiency of surgery and improved patients’ response to radiotherapy. It has also been shown to expose previously occult metastatic disease and reduce the incidence of microscopically positive margins and leaks from the pancreatic-enteric anastomoses. This article focuses on the effects of the trials and studies conducted on neoadjuvant therapy and also on the hindrances and limitations that must be overcome for this therapy to gain widespread traction.
Neoadjuvant therapy for patients with localized pancreatic adenocarcinomas was first reported in 1980, in a series of patients treated with radiation therapy alone. Of the 17 tumors treated, 15 were declared to be either unresectable or of borderline resectability by the surgeon who performed the initial exploratory celiotomy. The intent of the radiation therapy was to increase the resectability rate and to decrease the incidence of local and systemic recurrence. Six of the 17 patients underwent resection, and 2 of those lived for more than 5 years. Conclusions from the results of radiotherapy were that (1) preoperative radiation therapy is feasible and safe, (2) a thorough look for metastatic disease should be undertaken after completion of radiation therapy (because one-third of the patients demonstrated metastases after radiation treatment), and (3) response to radiation therapy should be an important parameter for selecting candidates for resectional surgery. It was also suggested that chemotherapy be tried as a radiation sensitizer.
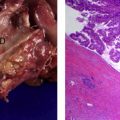
The first report of neoadjuvant radiation therapy combined with chemotherapy was published 10 years later. Fourteen patients were treated; 10 underwent resection, many with excellent histologic responses to treatment. The emphasis here was on increased resectability of locally advanced cancers and increased histopathologic response to the chemoradiation.
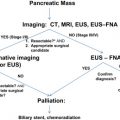
Two years later, Evans and colleagues reported their experience at the MD Anderson Cancer Center (MDACC) with patients who had potentially resectable disease. Contained within that publication was a grading scale for measuring the histologic response of pancreatic cancer to neoadjuvant treatment, which is still used today. Of the 28 patients treated, 5 developed metastatic disease during the period of neoadjuvant therapy. In every subsequent report of neoadjuvant therapy, at least 15% of the patients treated have demonstrated metastatic disease after restaging. The identification of patients with previously occult metastatic disease is one of the fundamental advantages of neoadjuvant treatment sequencing, as those patients who would not benefit from surgical resection are spared the risk of operative morbidity and mortality.
The second fundamental advantage of neoadjuvant sequencing was pointed out by 2 retrospective, single-institution studies of preoperative versus postoperative adjuvant therapy sequencing. These studies showed that of those who underwent upfront surgery, 24% and 22% were unable to complete postoperative adjuvant therapy. In contrast, nearly 100% of those who received neoadjuvant therapies completed therapy. Other advantages of neoadjuvant therapy are that it can reduce the incidence of microscopically positive margins and the leak from the pancreatic-enteric anastomosis. It is also widely theorized that there is superior tumor downstaging and better response to radiation therapy when treatment is given preoperatively because tissue oxygen delivery has not been disrupted by surgery.
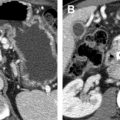
There have been numerous phase 2 experiences with neoadjuvant therapy published over the past 15 years. Median survival in these series has ranged from 12 to 45 months. This variability in outcome is much more likely a function of patient selection than treatment regimen. A relatively new development in the field has been the recognition and definition of the category now termed “borderline resectable cancers.” These are cancers that, although are technically resectable, have a higher-than-average risk of microscopic margin positivity and therefore are likely intermediate prognosis between clearly resectable and clearly unresectable cancers. Definitions for these cancers have been published by the National Comprehensive Cancer network (NCCN) and the MDACC pancreas cancer treatment group ( Table 1 ). Resectability for this group (averaging 40%) is considerably less than that for those with clearly resectable cancers (60%–80%). However, for those who tolerate and respond to the neoadjuvant therapy and whose cancers do not metastasize, resection with excellent survival rates is possible, perhaps as good as those with clearly resectable cancers. The MDACC group defined 2 other cohorts as borderline resectable. They defined “Group B” to include those patients with a high suspicion of occult distant metastatic disease. Examples include cases in which (1) a patient has had a previous abdominal exploration and was felt by the surgeon to have an unresectable cancer, (2) there have been biopsies of positive regional nodes, or (3) there are equivocal imaging findings of liver metastases. It may be useful to include patients with a high carbohydrate antigen 19–9 (CA 19–9) level in this category, although it is unclear what the cutoff value should be. The MDACC borderline category C consists of patients who are deemed too weak to undergo surgical resection but felt to be able to recover to such a point that they would be able to eventually undergo surgical resection.
| Blood Vessel Status | NCCN | MDACC |
|---|---|---|
| Superior mesenteric vein/pulmonary vein | Severely narrowed or occluded with possibility of reconstruction | Occluded with possibility of reconstruction |
| Superior mesenteric artery, hepatic artery, celiac axis | Abutment <180 ° | Abutment <180 ° |
It is clear from the many published phase 2 studies of neoadjuvant chemotherapy that most have accrued patients with either borderline resectable cancers or locally advanced unresectable cancers. Many of these studies were designed to convert unresectable tumors to resectable ones. Clearly, in patients with truly locally advanced tumors demonstrating encasement of the superior mesenteric artery, hepatic artery, or celiac axis, resectability is rarely, if ever, achieved after neoadjuvant regimens. The median survival reported in these trials therefore is likely a function of the composition of the study population (percentage of resectable vs borderline vs locally advanced) than of the specific treatment regimen. Only clear definition of the patient resectability status at study registration will help to differentiate successes from the various treatment programs.
Recent neoadjuvant experiences
A study by Evans and colleagues on preoperative gemcitabine and radiation therapy was restricted to only those patients with clearly resectable lesions as defined by the objective imaging criteria. Patients were treated with 7 weekly intravenous infusions of low-dose gemcitabine (400 mg/m 2 over 30 minutes) and 30 Gy of radiation therapy in 10 fractions over 2 weeks (weeks 2 and 3). They then had 4 weeks of rest and were restaged in week 12. A total of 86 patients were enrolled, and all were observed until death or for at least 6 years after treatment in case of the survivors. Unfortunately, CA19–9 levels were not reported. Distant metastases developed in 8 of 12 patients who did not undergo surgery (6 in liver, 2 in peritoneal cavity), whereas 1 did not return for treatment and 3 became too debilitated for resection. They each had recurrent distant disease development and died within 13 months of the initiation of treatment. No previously resectable tumor progressed locally such that a resection was denied. One patient did not return for surgery (cause not stated), therefore a total of 73 patients underwent surgery. Of those, 9 had laparoscopically determined (1) or open-abdomen determined liver metastases (6) or peritoneal metastases (3). In total, 64 patients underwent resection of a pancreatic head cancer. Of these, 13 (20%) required some form of superior mesenteric vein resection and 4 were tangential excisions with patch grafts. Only 4 patients (6%) had a microscopically positive superior mesenteric artery margin. One patient died of multisystem organ failure after an abscess following a pancreatic leak. Median survival was 34 months for these 64 patients, and their 5-year actual survival was 36%. This was an extraordinarily well-conducted trial with long follow-up of a large, homogeneous group of patients. Future phase 2 experiences for patients with resectable cancers can be compared with this cohort. If the same stringency of preoperative imaging and excellent surgical outcomes can be duplicated, then one could hold some degree of confidence that any survival differences would be a function of the adjuvant regimen or sequence.
The subsequent trial conducted at the MDACC studied patients with the same eligibility criteria and a longer and more aggressive systemic regimen of 4 treatments of neoadjuvant gemcitabine combined with cisplatin, followed by gemcitabine and 30 Gy of radiation therapy. However, the results showed no improvement in survival as compared with the former trial. An analysis of 4 consecutive phase 2 trials conducted at MDACC is provided in an article by Varadhachary and colleagues. There was a significantly greater number (60% vs 38%) of patients with node positive disease and also a significantly greater number of patients (36% vs 20%) who required a vascular resection in the last trial. Therefore, even in this extremely well-controlled series of neoadjuvant trials, it is not clear whether the addition of cisplatin to the chemotherapy-alone part of the neoadjuvant regimen is of benefit. Because of the strict adherence to protocol eligibility in their 4 trials, the investigators are quite confident that the superior median survivals seen for both the gemcitabine-containing regimens as compared with their previous 5-fluorouracil/radiotherapy and paclitaxel/radiotherapy regimens are only because of the differences in the drug regimens.
The concept of using full-dose neoadjuvant chemotherapy before or after radiation therapy was introduced within the last several years. Because the dominant pattern of recurrence after neoadjuvant therapy plus surgery in the previous MDACC series was distant (local recurrence 11%, isolated local recurrence 3%), the rationale for using the full-dose chemotherapy before radiation therapy was to reduce and possibly ablate the occult systemic disease at the earliest possible time. The rationale for full-dose chemotherapy after chemoradiotherapy in a Fox Chase Cancer Center study of patients with borderline resectable cancers was that (1) many tumors were still seen to abut or occlude major pancreatic vessels after completion of the chemoradiotherapy, and therefore more intensive chemotherapy might further increase the percentage of those achieving clear surgical margins, (2) the extensive surgical procedures envisioned might seriously delay the use of full-dose chemotherapy, and (3) this would be an improved method of selecting those patients who could truly benefit from resectional surgery. It is still too early to know whether the third rationale is justified, but in this study, 11 of 13 patients were able to undergo margin-negative resections, which was an improvement compared with historical patients with similar lesions treated with neoadjuvant chemoradiotherapy alone.
Problems in neoadjuvant trial design
Although comparisons of neoadjuvant regimens for resectable disease are difficult even when well conducted, such comparisons are simply impossible when studies include patients with borderline resectable cancers and locally advanced unresectable lesions. In fact, most of the neoadjuvant trials for pancreatic cancer consist of many, if not all, such patients. Clearly, only an objective definition of resectability combined with high-quality imaging that results in an anatomic description of the tumor-vessel relationships can allow for reproducible classification of tumors as potentially operable or not. This designation then serves as a surrogate for the chances that a surgeon may or may not be able to achieve an R0 resection. The fact that margin positivity confers a poorer survival provides the rationale for this use. However, it is important to remember that resectability as defined by initial imaging still represents an extrapolation because the anatomy of a primary tumor does not uniformly reflect tumor biology. The introduction in recent studies of a CA 19–9 level as an eligibility requirement is an attempt for it to serve as a prognostic factor that could reflect biology and allow for a more level playing field within and across trials. CA 19–9 is also not perfect as a predictor of prognosis because it may be affected by biliary obstruction and is not uniformly produced in humans. Better prognostic markers that reflect biologic behavior and the risk for occult metastatic disease are needed to accurately compare various neoadjuvant treatment regimens. This is particularly important given that neoadjuvant regimens cannot stratify patients based on pathologically derived TNM ( t umor, n ode, m etastasis) staging. Until such markers are identified, it is incumbent on the investigators of future trials and reports to define imaging-derived resectability properties of each of the patients studied, and their initial and posttreatment CA 19–9 values. Also no prognosis for patients whose tumors are defined as borderline resectable and then undergo successful resection after neoadjuvant treatment has been defined. This makes it difficult to create appropriate power calculations for sample size determination. The appropriate endpoints for such studies are also extremely difficult to define. Some investigators have proposed using overall resectability or R0 resection rates. However, these are flawed by the difficulties inherent in pathologic margin and surgical quality assessment. At this point, survival represents the most easily obtainable and least biased endpoint, particularly considering the lack of effective salvage therapies in this disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree