Pancreatic adenocarcinoma (PDA) is one of the cancers that is resistant to most conventional anticancer therapies. PDA-affected patients show a poor prognosis. The 5-year survival rate for PDA is 5% and has changed little over the past few decades. This has prompted extensive research to identify new agents that can be used for anticancer therapy. The only cytotoxic drug that has been approved by the Food and Drug Administration (FDA) is gemcitabine, which offers marginal benefits to patients in terms of symptom control and prolongation of life. Various strategies like targeting the epidermal growth factor receptor pathway and vascular endothelial growth factor receptor pathway have been researched upon. But these strategies have not provided promising results and none of the FDA-approved targeted agents have added any substantial clinical benefit to gemcitabine except for a marginal benefit from erlotinib. This article discusses various possible new targets and new agents for the anticancer therapy for PDA.
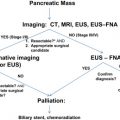
Pancreatic adenocarcinoma (PDA) remains a disease with poor prognosis. The 5-year survival rate is less than 5%, and has changed little over the past few decades despite improvements in diagnostic and surgical techniques. A major reason for the failure of therapy is the advanced stage of the disease at the time of diagnosis in most patients, and the presence of micrometastases in those who undergo curative surgical resection for radiographically localized disease.
Systemic therapy is therefore considered the only therapeutic option for most patients with PDA and an adjunctive treatment in patients with localized and resectable disease. However, PDA has shown marked de novo and acquired resistance to conventional cytotoxic therapies. The only cytotoxic drug approved by the Food and Drug Administration (FDA) for the treatment of PDA is gemcitabine, which offers patients a marginal benefit with respect to symptom control and prolongation of life. Attempts to significantly improve the outcome of patients treated with gemcitabine by the addition of other cytotoxic agents have repeatedly failed. For these reasons the median survival of patients with metastatic (stage IV) disease remains less than 6 months and less than 1 year for those with localized but unresectable disease. Patients with resectable PDA have a median of survival less than 2 years that may be modestly improved by the addition of gemcitabine.
Targeted therapies in pancreas cancer
With the advent of the targeted therapy in cancer treatment it was anticipated that novel drugs would be tested at a rapid rate in patients with PDA, given the lack of benefit from conventional cytotoxic therapies. Indeed several of these agents were tested in phase 2 and phase 3 trials in patients with advanced PDA. These drugs were investigated either as an add-on to gemcitabine and occasionally as a replacement for gemcitabine. Unfortunately, none of these drugs showed clinical benefit to patients with advanced pancreas cancer. Some of these drugs were chosen based on the knowledge of the molecular biology of PDA. For example, the high frequency (>85%) of K-RAS mutations in this disease rationalized the testing of farnesyltransferase inhibitors to interrupt the RAS-mediated oncogenic signaling that is an early event in pancreatic carcinogenesis. Tipifarnib was the first putative ras inhibitor to undergo clinical testing in PDA. The study design, however, did not include testing of in vivo tumoral modulation. It was also not known to what extent (if any) farensyltransferase inhibition or RAS inhibition would influence the natural history of advanced PDA. These drugs did not seem to have single agent activity that was clinically significant in PDA and other cancers. Another class of drugs that underwent phase 3 testing included the matrix metalloproteinase inhibitors. These agents did not add benefit to gemcitabine and were not superior when tested against gemcitabine. Other targeted molecules have been tested in pilot trials in molecularly unselected cohorts of patients with locally advanced and metastatic PDA without any encouraging efficacy signals to justify undertaking phase 3 testing. Despite limited interest in studying some of these targets (eg, COX-2), additional studies with better patient selection and combined targeted approach is still required.
Targeting the Epidermal Growth Factor Receptor Pathway
The epidermal growth factor receptor (EGFR) pathway has generated much interest as a target in PDA, based on (1) the frequent expression of the EGFR protein by these tumors, (2) the association of EGFR expression with a poorer outcome, (3) evidence that EGFR blockade has antitumor activity in preclinical systems, and (4) the availability of anti-EGFR drugs that have established single agent activity in other tumor types (eg, colorectal and lung cancer). Two strategies of targeting EGFR have been tested in patients with advanced PDA: small molecule tyrosine kinase inhibitor therapy using erlotinib and monoclonal antibody against the extracellular domain of EGFR using cetuximab.
A phase 2 trial of cetuximab suggested that it may have activity in combination with gemcitabine. In this study, the survival rate at 1 year was increased compared with historical data of single agent gemcitabine. This concept was therefore studied in a phase 3 trial run by the Southwest Oncology Group (SWOG) during which 762 patients were randomized to receive gemcitabine alone or gemcitabine plus cetuximab. The study was reported in 2007 and showed no survival benefit of adding cetuximab in patients with advanced PDA when compared with gemcitabine alone. There were also no differences in objective responses or time taken for disease progression between the 2 study arms. Another randomized phase 2 study of cetuximab from Europe failed to show a worthwhile benefit from the addition of cetuximab to gemcitabine and cisplatin therapy in patients with advanced PDA.
Moore and colleagues from the National Cancer Institute of Canada tested erlotinib in combination with gemcitabine versus gemcitabine plus placebo in patients with advanced PDA in a phase 3 setting (NCIC.PA3). Unlike cetuximab, which was first tested in pilot phase 2 trial to be followed by a phase 3 trial, erlotinib was tested in only a phase 3 trial. Although the magnitude of benefit in median survival reported in this study was just under 2 weeks, it did achieve statistical significance in favor of erlotinib (Hazard ratio = 0.82, P = .038). Erlotinib did add toxicity to gemcitabine, primarily causing skin rash and diarrhea. The presence and intensity of the rash (≥grade 2) correlated with the survival of patients. Erlotinib was approved by the FDA for the treatment of patients with advanced PDA in combination with gemcitabine. However, its adoption by community oncologists is not uniform as the magnitude of benefit must be balanced against its cost, and the additional side effects. This is particularly pertinent in older patients and those with unfavorable performance status. No data are available to justify use of erlotinib as a single agent or in combination with other cytotoxic drugs (eg, fluoropyrimidines) in patients with advanced PDA. Its benefit in the adjuvant setting will be determined in an upcoming international collaboration (RTOG 0848) led by the Radiation Therapy Oncology Group (RTOG), SWOG, and European Organization for Research and Treatment of Cancer in patients who undergo curative surgical resection of pancreatic head adenocarcinoma.
Targeting Angiogenesis
As the benefits of targeting the vascular endothelial growth factor (VEGF) and vascular endothelial growth factor receptor (VEGFR) were being shown in several solid tumors (eg, colon, renal cell cancer), there was great enthusiasm to test anti-VEGF/VEGFR drugs in patients with advanced PDA. Indeed a pilot trial suggested a potential benefit of adding bevacizumab, a monoclonal antibody against VEGF to gemcitabine in patients with advanced PDA, selected on the basis of absence of history of major thromboembolic and cardiovascular disease. Soon after communicating the phase 2 study results, a phase 3 trial was launched by the Cancer and Leukemia Group B, randomizing patients with advanced PDA for testing the effect of gemcitabine plus placebo or bevacizumab added to gemcitabine. Unfortunately, results of the study reported in 2007 showed no benefit of bevacizumab when added to gemcitabine. An international phase 3 study in patients with advanced PDA tested the combination of gemcitabine with aflibercept, a VEGFR-like molecule to trap free VEGF, but the combination did not meet its primary end point of improving overall survival.
The multikinase inhibitor axitinib was also tested in advanced pancreas cancer. Axitinib is a small molecule targeting receptor tyrosine kinase of VEGFR 1-3 in addition to c-KIT and PDGFRβ. After a pilot randomized phase 2 trial suggesting possible activity for the agent in combination with gemcitabine, the same regimen was quickly moved to phase 3 testing in patients with advanced PDA against gemcitabine. However, the combination of axitinib and gemcitabine failed to improve the primary end point of survival in patients with advanced PDA according to a press release by the sponsor.
Another antiangiogenesis strategy is to target the endothelial cell by cytotoxic drugs (cationic liposomal paclitaxel), target the molecules in the endothelial cell (cilengitide), or the tubulin support (ZD6126). Cationic liposomes bind and internalize at tumor endothelial cells, producing an antivascular effect. In a pilot study, the combination of cationic liposomal paclitaxel with gemcitabine suggested an added but modest antitumor effect that cannot be confirmed to be a result of vascular interruption or simply an added cytotoxic effect against the tumor cells. A study of cilengitide that inhibits the binding of vitronectin to the integrin avb3 failed to show benefit when added to gemcitabine in a randomized phase 2 trial.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree