Adjuvant therapy for pancreatic cancer remains a controversial topic, with a paucity of randomized controlled trials in this area and various limitations in the trials that have been conducted to date, leaving many questions as to a true “standard of care” for patients with resectable or potentially resectable disease. Several large and well-conducted phase 3 trials have reported results recently and have helped to solidify the role of chemotherapy, with either 5-fluorouracil or gemcitabine, as an effective intervention in the adjuvant setting. The role of radiotherapy remains unclear, but it does seem to be feasible and safe, and there are trials in development that may shed more light on this question. Many small trials have pointed to the potential utility of neoadjuvant strategies in selecting the patients who are most likely to benefit from surgery and in improving outcomes by providing systemic therapy early on. Larger trials are ongoing in hopes that they will give more definitive answers as to when this strategy should be used. It is hoped that trials using novel agents, either alone or in combination with more traditional therapies, will better define the best strategy for improving outcomes in patients with resectable disease.
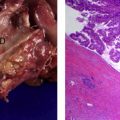
Although pancreatic cancer is the 11th most common cancer in the United States, it remains the 4th most common cause of cancer death. There were an estimated 38,000 new cases of pancreatic cancer in 2008, with more than 34,000 deaths, resulting in a case fatality index of more than 90%. Surgical resection remains the only chance of cure, and advances in surgical and perioperative care have led to markedly decreased morbidity and mortality rates. Most patients present with unresectable disease, and surgery is feasible only in approximately 15% to 20% of these patients. Even after potentially curative resection, recurrence rates remain as high as 90%, and most patients eventually succumb to their disease. This high recurrence rate implies that pancreatic cancer is a systemic disease in most patients at the time of diagnosis, and therefore surgical resection alone is not adequate. As a result, investigations into multimodality treatment, including chemotherapy and/or chemoradiation, have been actively pursued. These treatments can be given both in the adjuvant (postoperative) setting and in the neoadjuvant (preoperative) setting. This article reviews the data that are currently available on adjuvant and neoadjuvant strategies in the treatment of pancreatic cancer.
Adjuvant therapy
Historical Perspective
In the United States, the standard of care for adjuvant therapy for pancreatic cancer has been based largely on several small trials, the first significant one being the Gastrointestinal Tumor Study Group (GITSG) trial published in 1985. This trial, which randomized a total of 49 patients between 1974 and 1982, enrolled only patients with negative surgical margins and who had pancreatic adenocarcinoma confirmed by histology (excluding patients with periampullary carcinoma, islet cell carcinoma, or cystadenocarcinoma). Patients were randomized after resection to receive 5-fluorouracil (FU) chemotherapy plus radiotherapy or observation alone. Patients were stratified at the time of randomization by the type of surgical procedure, degree of differentiation, stage of disease, and location of primary tumor. Ninety-five percent of patients had primary cancer of the head of pancreas, and 28% had node-positive disease. Radiotherapy was given in 2 courses of 20 gray (Gy) each, separated by a 2-week interval, for a total of 40 Gy. Chemotherapy with 5-FU (500 mg/m 2 intravenous bolus) was administered at the beginning of each course of radiotherapy for 3 consecutive days and then continued on a once-weekly basis for 2 years or until disease recurrence was noted. With 43 patients in the final analysis, median survival was improved (20 months vs 11 months) with the addition of adjuvant therapy, and this did meet statistical significance ( P = .035). However, problems noted with this trial include the small sample size, slow accrual rate, and a radiotherapy regimen felt to be inferior by modern methodology. In addition, this trial was not designed to examine the benefits of the individual components of adjuvant therapy (chemotherapy vs chemoradiotherapy); so it is unclear from where most benefit, if any, was derived.
Most subsequent trials have been limited in size or have had other methodologic problems ( Table 1 summarizes important phase 3 adjuvant trials). In 1999, the Gastrointestinal Tract Cancer Cooperative Group of the European Organization for Research and Treatment of Cancer (EORTC) published a phase 3 trial comparing radiotherapy plus 5-FU with observation alone in the adjuvant setting. Two hundred eighteen patients were randomized from 1987 to 1995, to receive either observation alone or a combination of 5-FU as a continuous infusion (CI) concomitantly with radiotherapy. After chemoradiation was completed, patients were followed and received no more chemotherapy unless they relapsed. The median survival was 19 months for the observation group and 24.5 months for the treatment group, but this result was not statistically significant (logrank, P = .208) and was further confounded by the inclusion in this trial of patients with periampullary tumors, who made up almost half of the cohort. In a subset analysis, there was a nonsignificant trend toward improved survival in the pancreatic cancer cohort when adjuvant therapy was given (17.1 months vs 12.6 months, P = .099). Although the EORTC trial gave some additional hints of benefit with adjuvant therapy, it also left several important questions unanswered.
| Trial | Recruitment (Margins/Nodes) | Comparison | Adjuvant Treatment | Number of Patients Randomized | Published Conclusions |
|---|---|---|---|---|---|
| GITSG, 1985 | 1974–1982 All R0 28% node (+) | CRT vs Obs | 2 × (20 Gy in 10 fractions + 500 mg/m 2 5-FU d1-3) + weekly 5-FU to recurrence | 49 pancreas patients | Of 43 patients analyzed, significant increase in median survival (20 vs 11 mo, P = .035) |
| EORTC, 1999 | 1987–1995 20% R1, 38% node (+) | CRT vs Obs | 2 × (20 Gy in 10 fractions + 25 mg/kg 5-FU/FA d1-5) | 218 patients (55% pancreas, 45% periampullary) |
|
| ESPAC-1, 2001, 2004 | 1994–2000 19% R1, 54% node (+) |
|
| 289 pancreas patients | In 289 analyzed patients, NS decrease in survival for CRT ( P = .053), but significant increase in survival for CT ( P = .009) |
| ESPAC-1 plus, 2001, updated 2008 | 1994–2000 23% R1, 51% node (+) |
|
| 261 pancreas patients |
|
| CONKO-001, 2007, updated 2008 | 1998–2004 17% R1, 72% node (+) | CT vs Obs | 6 mo × (1000 mg/m 2 gemcitabine d1, 8, 15 qd) | 368 pancreas patients | In 354 analyzed patients, significant increase in survival for gemcitabine, 13.4 vs 6.9 mo, P <.001). Estimated DFS at 3 and 5 y 23.5% and 16% vs 8.5% and 6.5% |
| RTOG 97-04, 2008 | 1998–2002 34% R1, 66% node (+) | 5-FU CT plus CRT vs gemcitabine CT plus CRT |
| 451 pancreas patients | NS difference in overall survival or DFS. In pancreatic head subgroup, median survival of 20.5 mo and 3-year survival of 31% in gemcitabine group vs 16.9 mo and 22% in 5-FU group (HR = 0.82, P = .09) |
Modern Trials
Since the publication of these early trials, several large studies have helped to clarify some of the issues related to adjuvant therapy for pancreatic cancer. The first was the European Study Group of Pancreatic Cancer–1 (ESPAC-1) trial, a complex trial designed to answer several questions about adjuvant therapy for pancreatic cancer. This trial was initially designed with a 2 × 2 factorial design to compare adjuvant chemoradiotherapy, 6 months of adjuvant chemotherapy, and a combination of these, with an additional observational control arm. The results of this trial were published during a span of years, with the first report in 1997 detailing the study design. In the radiotherapy group, a course of 40 Gy was given with 5-FU as a sensitizing agent, using the same schedule and doses as were used in the GITSG trial. In the chemotherapy arm, patients received folinic acid with bolus 5-FU at a dose of 425 mg/m 2 for 5 consecutive days every 28 days for 6 cycles, for a total of 28 weeks. Patients randomized to both treatment arms were to receive chemoradiation first, followed by the full course of chemotherapy. Patients were stratified by margin status at initial randomization. The primary endpoint was to look for an improvement of 20% to 40% in the 2-year survival rate in patients with negative margins for each of the 2 randomizations. The investigators estimated that 220 margin-negative patients would give a power of 90% with an α level of .05 for each randomization procedure. This analysis means that the study was not powered to perform comparisons between each of the 4 arms that result from the 2 × 2 randomization schema. Because this trial did allow the enrollment of margin-positive patients, the accrual plan was to enroll 280 patients in the analysis to reach the goal of 220 margin-negative patients in each arm. Other patients were allowed “on study” and to participate in only 1 of the 2 randomizations but not both. However, these patients were never a part of the planned analysis and were appropriately excluded from the final results, which is fortunate because this cohort included periampullary cancers and nonductal carcinomas and would have introduced significant heterogeneity into the analysis. The primary endpoint of 2-year survival for margin-negative patients was not reported in the main analysis of this trial, but for the overall group, the 2-year survival for those receiving chemotherapy was 40% and for those not receiving chemotherapy, 30% (no P value reported). The 2-year survival rate for patients receiving chemoradiation was 29%, compared with 40% for those not receiving chemoradiation. For chemotherapy randomization, a secondary end point analysis demonstrated that the hazard ratio (HR) for death was statistically significantly improved in patients receiving chemotherapy compared with those not receiving chemotherapy (HR = 0.71, P = .0009), and median survival for the chemotherapy arm was 20.1 months versus 15.5 months for the no-chemotherapy arm, with no P values reported. The same analysis was performed in the chemoradiotherapy arm, and this analysis suggested worse outcomes for patients receiving chemoradiotherapy, with an HR for death of 1.28 ( P = .05). Median survival was 15.9 months for patients receiving chemoradiotherapy and 17.9 months for patients who did not receive chemoradiotherapy. Five-year survival rate was 21% among patients who received chemotherapy and 8% among patients who did not receive chemotherapy ( P = .009), and it was 10% among patients randomized to receive chemoradiotherapy and 20% among patients who did not receive chemoradiotherapy ( P = .05).
The ESPAC-1 trial helped in establishing a clear role for chemotherapy in the adjuvant setting, but it also introduced a controversy regarding the role of radiotherapy. The authors of the trial have suggested that the chemoradiation protocol used in this trial may have been detrimental because it delayed the start of full-dose chemotherapy and used a 2-week rest period in the middle of the therapy that is considered suboptimal, as it potentially allows for the growth of tumor cells during this period of time. Compliance issues with the chemoradiotherapy administration were also present, with patients receiving variable doses of radiotherapy despite a recommendation for 40 Gy. There was no central review of radiation ports for quality assurance purposes; so this trial may not tell us much about the role of modern radiotherapy regimens in the adjuvant setting. Additional data from this trial and some composite data from the ESPAC-1 plus trial and ESPAC-3 (v1) trial were reported online in January 2009, and these results recapitulate the results reported in 2004. The ESPAC-1 plus trial is a cohort of 192 patients who were entered into a direct randomized comparison between 5-FU and observation alone with clinician’s choice of background chemoradiotherapy, if indicated. This cohort was conducted as part of the ESPAC-1 trial and adhered to the same eligibility criteria and treatment schedules, and it was intended to be additional evidence and was thus not powered for analysis apart from the larger ESPAC-1 cohort. The ESPAC-3 (v1) trial was initially a 3-arm study of adjuvant 5-FU versus gemcitabine versus observation alone. After the publication of the results of the larger ESPAC-1 trial, the observation arm was dropped from ESPAC-3 (v2), and some preliminary results were published after the accrual of 122 patients to this substudy. The combined analysis pooled data from each of these component studies, and again the benefit of adjuvant chemotherapy is seen, with overall survival in patients randomized to receive 5-FU exceeding that of patients treated with surgery alone and with a pooled HR for death of 0.70 in the chemotherapy arm ( P = .003). The composite 2-year survival rate was reported as 49% for the 5-FU arm and 37% for the observation arm (no P value reported).
Since the publication of the ESPAC-1 data, 2 additional randomized phase 3 trials have been reported that have given more insight into how to provide best care for patients with pancreatic cancer after resection. The first of these was Charité Onkologie (CONKO)-001, a multicenter trial comparing adjuvant chemotherapy with gemcitabine with observation alone. Patients were randomized on a 1:1 basis and stratified for resection status (R0 vs R1), T status (T1–2 vs T3–4), and nodal status (N + or N − ). Patients in the gemcitabine group received 3 weekly infusions of gemcitabine at a dose of 1000 mg/m 2 for 3 weeks on and 1 week off, for a total of 6 cycles. The primary endpoint of the trial was disease-free survival, with a secondary endpoint of overall survival. A sample size of 368 patients was required to detect a difference of 6 months in disease-free survival, with a statistical power of 90% at a 2-sided α level of .05. Estimated disease-free survival was 13.4 months in the gemcitabine group compared with 6.9 months in the control group ( P = .001), and this finding held up regardless of margin status, tumor size, or nodal involvement. At the time of initial publication, there was no statistically significant benefit seen in overall survival numbers, but these results were updated at the 2008 ASCO Annual Meeting, and it was reported that patients receiving adjuvant gemcitabine had a median survival rate of 22.8 months, versus 20.2 months for patients receiving observation alone ( P = .005). Estimated 5-year survival for the gemcitabine arm was 21% compared with 9% for the observation arm. It is likely that this benefit was also somewhat diluted in patients receiving gemcitabine at the time of relapse, and thus it is all the more encouraging that this result held up despite the crossover.
At about the same time as CONKO-001, Radiation Therapy Oncology Group (RTOG) 97-04 began to accrue patients in North America. RTOG 97-04 was a large intergroup trial conducted by the RTOG, the Eastern Cooperative Oncology Group (ECOG), and the Southwest Oncology Group, inclusive of Canadian affiliates. This trial included 451 patients with pancreatic adenocarcinoma, with 75% of patients having T3 or T4 disease and approximately 66% of patients having node-positive disease. One-third of patients had positive margins. Randomization was performed after surgery and was stratified by tumor diameter (<3 cm or ≥3 cm) and surgical margins (33% of patients had positive surgical margins). Patients were randomly assigned to either 5-FU (group 1) or gemcitabine (group 2). Chemotherapy before chemoradiotherapy in group 1 consisted of CI of 5-FU (250 mg/m 2 ) daily for 3 weeks, and in group 2 it consisted of a 30-minute infusion of gemcitabine (1000 mg/m 2 ) once weekly for 3 weeks. Within the next 2 weeks, both groups began identical chemoradiation regimens (50.4 Gy with a CI of 250 mg/m 2 of 5-FU daily through the course of radiotherapy). An additional phase of chemotherapy was initiated 3 to 5 weeks after the completion of chemoradiation, with group 1 receiving 3 months of infusional 5-FU daily for the next 3 months (4 weeks on and 2 weeks off for 2 cycles) and group 2 receiving 3 months of gemcitabine (3 weeks on and 1 week off). Prospective quality assurance procedures were used, including central review of preoperative computed tomography scans and radiation therapy fields, before the initiation of chemoradiation. For the primary analysis, 330 patients were needed to detect a 33% reduction in the hazard rate of overall survival for the chemoradiation plus gemcitabine group compared with that of the chemoradiation plus 5-FU group, with 80% power and a 2-sided α level of .05. In early 2001, the protocol was amended because of unexpectedly rapid accrual, and the sample size was increased to find a smaller treatment effect with more power. For the final analysis, 451 evaluable patients were included, and there was found to be no difference in the overall or disease-free survival rates among treatment groups. As part of the second primary objective of the study, a subgroup analysis of patients with tumors in the head of the pancreas was performed, and these patients had a median survival of 20.5 months and a 3-year survival of 31% in the gemcitabine group compared with 16.9 months and 22% in the 5-FU group (HR = 0.82, P = .09). However, after adjusting for prespecified stratification variables of nodal status, tumor diameter, and surgical margin status, the treatment effect yielded an HR of 0.80 ( P = .05). At the time of relapse, 82% of patients in the 5-FU group received gemcitabine chemotherapy; so it is speculated that the use of salvage gemcitabine may have reduced the effect observed for overall survival. Although this trial was large and adequately powered, it did not clearly demonstrate an advantage for gemcitabine over 5-FU in the adjuvant setting and certainly did not address the more pressing issue of whether chemoradiotherapy added any benefit or was detrimental to patients as suggested in ESPAC-1.
Taken together, the results of the trials detailed earlier suggest that patients with resected pancreatic cancer are likely to benefit from adjuvant chemotherapy with 5-FU or gemcitabine, irrespective of margin status or nodal status. Further support for this statement comes from ESPAC-3 (v2), reported at the 2009 ASCO Annual Meeting. In this study, more than 1000 patients were randomized either to 5-FU 425 mg/m 2 daily for 5 days given every 4 weeks with leucovorin 20 mg/m 2 on the same schedule or to gemcitabine given on the same schedule as in the CONKO-001 study. There was no difference in either disease-free survival or overall survival between the 2 treatment arms, with 23 months median survival in the 5-FU arm compared with 23.6 months median survival in the gemcitabine arm. However, the role of chemoradiation in the adjuvant setting is still somewhat unclear. Although RTOG 97-04 was a well-designed and conducted study, it did not answer the question about the benefit, or perhaps potential detriment, of adding chemoradiation. A new, EORTC randomized phase 2 trial (40013) comparing gemcitabine alone with gemcitabine plus radiation using modern chemoradiation techniques was reported at the 2009 ASCO Annual Meeting. Ninety patients were randomized to chemotherapy or to chemoradiation. The overall survival for both arms was 24 months; however, there was a significant improvement in local control with the use of chemoradiation. Because local control is of limited benefit when systemic disease is the main driver of survival, it may be difficult to demonstrate benefit for radiation until the systemic treatment of pancreatic cancer improves. Thus, several important questions remain to be answered, and fortunately, there are a few trials ongoing or yet to be reported that may shed some light on several of these issues.
- •
RTOG 0848 randomizes patients with adenocarcinoma of the head of the pancreas to receive either gemcitabine alone or gemcitabine plus erlotinib after surgery. After 5 months of this therapy, if patients have not developed progressive disease, they are randomized to receive either another month of their respective chemotherapy alone or another month of their respective chemotherapy followed by a course of chemoradiation with either 5-FU or capecitabine. This trial is in the final stages of development, and its design will answer 2 questions: benefit of the addition of erlotinib to standard gemcitabine and benefit of the use of consolidation chemoradiation therapy. This will be an intergroup study conducted in the United States, Canada, and Europe.
- •
ECOG 2204 is a completed trial that randomized patients to receive either gemcitabine plus bevacizumab or gemcitabine plus cetuximab, followed by 5.5 weeks of chemoradiation with capecitabine, followed by 3 additional cycles of the original chemotherapy regimen. Results of this trial are expected in 2010.
- •
American College of Surgeons Oncology Group (ACOSOG) Z5041 is ongoing and is evaluating the use of gemcitabine plus erlotinib pre- and postresection.
New Directions
Combinations of chemotherapy regimens with or without various radiotherapy regimens are clearly useful and needed, but previous experience suggests that there is no panacea in these types of agents for this lethal disease and that innovative therapeutics are sorely needed. As more targeted agents are being evaluated in the metastatic and locally advanced (LA) setting, it is hoped that a few promising agents may make their way to evaluation in the adjuvant setting, and these may offer new options for patients with resectable disease. A safety and efficacy trial of lethally irradiated allogeneic pancreatic tumor cells transfected with the granulocyte-macrophage colony-stimulating factor gene, along with adjuvant chemoradiotherapy, was presented at the Gastrointestinal Cancer Symposium in 2007, and immune correlative data were presented at the 2008 ASCO Annual Meeting; so it will be interesting to see if this immune approach may lead to new classes of therapeutics for resected patients.
Neoadjuvant therapy
Rationale of Neoadjuvant Therapy for Pancreatic Adenocarcinoma
The use of neoadjuvant or preoperative therapy for the treatment of resectable pancreatic adenocarcinoma offers several potential advantages over adjuvant strategies ( Table 2 ). First, the use of neoadjuvant therapy may lead to downsizing of the tumor that may afford improved margin-negative resection rates and lower local-recurrence rates. This may be particularly important in patients who are considered “borderline resectable” in addition to those who seem resectable at diagnosis. Second, it may allow one to select patients who would benefit the most from pancreatic resection and to avoid unnecessary surgery and its associated morbidity in those patients with rapidly progressive disease. Third, it may allow one to deliver treatment to better-perfused and better-oxygenated tissues before surgical manipulation, thereby enhancing the effects of chemotherapy or radiation. The use of neoadjuvant strategies may also result in better patient tolerance and a decrease in complications (such as pancreatic leak with the use of preoperative radiation). Multiple studies and trials show that a significant number of patients, up to 20% to 30%, fail to receive planned adjuvant therapy after pancreatic resection. This may be because of perioperative complications that result in poor tolerance of cytotoxic therapy and patient refusal after a major operative procedure and recovery. Even in patients who are able to receive adjuvant therapy, there is often a delay of several weeks before receiving their first dose. Moreover, in a disease with such a high local and distant relapse rate, the use of neoadjuvant therapy allows systemic therapy to be given early to treat occult metastases.
| Advantages | Disadvantages |
|---|---|
| Potential ability to downsize tumors and increase margin-negative resection rates | Often requires biliary stenting for drainage and its associated complications |
| Avoidance of surgery in patients with rapidly progressive and occult metastatic disease | Requires tissue confirmation of tumor |
| Potentially better tolerance of chemotherapy and radiation than in the adjuvant setting | Local progression of disease making the tumor nonresectable |
| Ability to reduce the risk of pancreatic anastomotic leak (radiation) | Potential overtreatment in patients with early disease |
| Ability to deliver systemic therapy early (chemotherapy) to a systemic disease | Potential need to obtain neoadjuvant therapy at a specialized center |
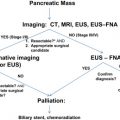
The use of neoadjuvant therapy also has potential disadvantages and pitfalls, however (see Table 2 ). In patients with jaundice, for example, reliable preoperative biliary drainage, such as stenting, must be established before receiving chemotherapy. The use of preoperative stents has been associated with an increase in perioperative complications in several reports. In addition, a pathologic confirmation of pancreatic adenocarcinoma is required before administering cytotoxic chemotherapy. Although there have been improvements in techniques such as endoscopic ultrasound with fine needle aspiration, this technique is operator dependent and is not always readily available outside of major referral centers. In patients who are resectable, ineffective neoadjuvant strategies may lead to local progression of the tumor, thereby resulting in an inability to perform surgery. Proponents of neoadjuvant therapy argue, however, that among patients who progress while receiving therapy, surgical resection would rarely result in a survival benefit in patients with such aggressive disease. Finally, neoadjuvant therapy is often given under the context of a clinical protocol and may require patients to be referred to a major center to undergo therapy.
A prospective randomized trial would be required to directly compare the efficacy of neoadjuvant therapy with that of adjuvant therapy. To date, there have been no randomized comparisons, and therefore it is difficult to reach definite conclusions. In addition, varying definitions of what is considered resectable, LA, and borderline resectable have led to the inclusion of a heterogeneous group of patients in neoadjuvant studies, thus making comparisons even more difficult. Nevertheless, there have been several well-performed single-institution trials and a few multi-institutional trials suggesting that neoadjuvant strategies may be an effective approach to patients with pancreatic cancer and that they are worthy of continued investigation.
Neoadjuvant Therapy for Resectable Disease
The first reported trials using neoadjuvant therapy for resectable pancreatic cancer were published in the early 1990s ( Table 3 ). Initial experience involved the use of 5-FU–based chemoradiation using a standard 50 Gy given over 5.5 weeks and a rapid fractionation course of 30 Gy. Most patients tolerated these regimens well, and about 60% ultimately underwent successful resection with median survivals around 2 years. Of the patients who were found to be unresectable at laparotomy, nearly all were due to metastatic disease rather than local progression alone. Although these initial results compared favorably with the results from adjuvant studies, the reported survival was only for the select patients who were able to undergo successful resection.
| Author, Year | Number | Regimen | Resection Rate | Positive Margin | Median Survival | |
|---|---|---|---|---|---|---|
| All Patients | Resected Patients | |||||
| Yeung et al, 1993 a | 26 | MMC, 5-FU + 50.4 Gy | 38% | 0% | 11 mo | NR |
| Staley et al, 1996 | 39 | 5-FU + 50.4 Gy/30 Gy + IORT | 100% c | 18% | 19 mo c | 19 mo |
| Hoffman et al, 1998 a | 53 | 5-FU, MMC + 50.4 Gy | 45% | 33% | 11 mo | 16 mo |
| Pisters et al, 1998 | 35 | 5-FU + 30 Gy + IORT | 57% | 10% | NA | 25 mo |
| Pisters et al, 2002 | 37 | Paclitaxel + 30 Gy + IORT | 54% | 32% | 12 mo | 19 mo |
| White and Tyler, 2004 | 96 | 5-FU, 50.4 Gy ± MMC ± cis | 55% | 25% | NA | 39 mo |
| Moutardier et al, 2004 | 61 | Cisplatin, 5-FU + 45–60 Gy | 66% | 7.5% | 13 mo | 27 mo |
| Mornex et al, 2005 | 41 | Cisplatin, 5-FU + 50 Gy | 63% | NA | 12 mo | 13 mo |
| Talamonti et al, 2006 | 20 | Gem + 36 Gy | 85% | 6% | NA | 26 mo |
| Palmer et al, 2007 | 24 | Gem | 38% | 25% b | 9 mo | 28 mo |
| 26 | Gem, cisplatin | 70% | 25% b | 16 mo | ||
| Evans et al, 2008 | 86 | Gem + 30 Gy | 74% | 11% (6%) b | 23 mo | 34 mo |
| Varadhachary et al, 2008 | 90 | Cisplatin, Gem + 30 Gy | 58% | 4% (2%) b | 17 mo | 31 mo |
a Also included patients with LA disease.
b Posterior (retroperitoneal) margin-positive rate.
Other reported combinations have included the use of CI 5-FU, mitomycin C (MMC), and concurrent external beam radiotherapy (XRT). Yeung and colleagues reported on 26 patients with resectable and LA pancreatic adenocarcinoma who were treated with 50.4-Gy XRT, CI 5-FU, and MMC. The overall resectability rate was 38%, but the margins were negative in all cases, and at the time of publication with a median follow-up of 29 months, the median survival for resected patients had not been reached. In an ECOG trial reported in 1998, 53 patients with potentially resectable and LA lesions also received neoadjuvant 50.4-Gy XRT along with CI 5-FU and MMC. Although most patients completed treatment, the regimen was noted to have significant toxicity, with 51% of patients requiring hospitalization and 43% developing grade 3–5 hepatic toxicity. Twenty-four patients (45%) ultimately underwent resection, and the median survival of the resected patients was 15.7 months. Although these results are less impressive than others, both of these trials included patients with resectable and LA diseases, highlighting the importance of designing trials that separate these patients depending on well-defined criteria of resectability.
Other combinations include the use of CI 5-FU along with cisplatin and XRT. In the trial by Moutardier and colleagues, 40 of 60 patients (65.5%) went on to resection, and the median disease-free survival for the resected group was 27 months, whereas the overall median survival for the entire group was 13 months. Of note, of the 40 patients who went on to surgery, 6 had a major response, 3 had a complete response, and 5 had tumor progression. Similarly, in a French trial of 41 patients using a similar regimen, 26 patients (63%) went on to resection. One complete pathologic and 12 partial responses were noted, and the margins were negative in 80% of the patients. The median survival for all patients was 11.5 months and 12.5 months for the resected patients. These results were somewhat disappointing in comparison with others, although the authors noted a 32% 2-year survival for resected patients.
Gemcitabine has also been used in combination with radiation in the neoadjuvant setting. Based on an earlier phase 1 trial, Talamonti and colleagues reported on a cohort of resectable patients as part of a multi-institutional phase 2 trial of nonmetastatic pancreatic cancer (see later discussion) using full-dose gemcitabine and 36 Gy of limited field XRT. Of the 20 patients with potentially resectable disease, 17 underwent resection. A negative (R0) margin was achieved in 94%, and the median survival for the resected patients was an impressive 26 months. Although this study was small and not designed as a neoadjuvant trial, these results compared favorably with those using 5-FU-based chemoradiation and suggested that gemcitabine-based chemoradiation may be the preferred regimen in the neoadjuvant treatment of pancreatic cancer.
Evans and colleagues recently reported on a phase 2 trial of preoperative gemcitabine-based chemoradiation in 86 patients with stage I/II pancreatic head adenocarcinoma using 30 Gy. Although 41% required hospital admission, a total of 74 patients were eligible for resection, and 64 were successfully resected (74% of the total). All the patients had progressed with metastatic disease rather than local progression. Negative microscopic margins were achieved in 89%. The median overall survival for all 86 patients was 22.7 months and an unprecedented 34 months for the 64 patients who underwent resection. Overall 5-year survival was 36% for the patients who underwent resection and 0% for those who did not. These results, once again, were impressive and lend further support for the use of gemcitabine-based chemoradiation as a neoadjuvant approach for pancreatic cancer.
Varadhachary and colleagues from MD Anderson Cancer Center reported on a phase 2 trial of 90 patients who received preoperative systemic gemcitabine and cisplatin for 4 weeks, followed by gemcitabine-based chemoradiation (30 Gy) in hopes of defining the role for systemic chemotherapy before resection. A total of 79 patients (88%) completed the preoperative regimen, although hospital admission was required for 51%. A total of 62 patients went to the operating room, and ultimately, 52 were successfully resected with a margin-negative rate of 96%. Of the 27 patients who were not resectable after preoperative treatment, 4 were not resected because of local tumor factors alone. Median overall survival was 17.4 months for all 90 patients, 18.7 months for the 79 patients who completed therapy, and 31 months for the 52 patients undergoing successful resection. The median survival for the 27 patients not undergoing resection was only 10.5 months. Although these results were also encouraging, the investigators noted that the addition of systemic gemcitabine and cisplatin did not seem to improve the survival rate when compared with gemcitabine-based chemoradiation alone. Looking at both studies, the investigators also note that a small minority of patients had local progression alone precluding resection without having metastatic disease, implying that the addition of neoadjuvant therapy, particularly chemoradiation, will lead to “losing the window of resection” in only a small minority of patients.
Neoadjuvant Therapy for LA or Borderline Resectable Disease
Most patients diagnosed with pancreatic cancer are not resectable, because of either systemic metastases or LA disease. For a subset of patients with LA or borderline resectable disease, neoadjuvant strategies may be able to downstage patients, improve margin-negative resection rates, and allow one to monitor for progression of occult metastatic disease. The main difficulties in analyzing trials and studies involving borderline resectable and LA lesions are the lack of a standard definition and the lack of consistent preoperative staging techniques and standards.
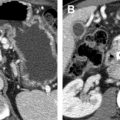
Defining borderline resectable and LA disease
The National Comprehensive Cancer Network (NCCN) defines a tumor as borderline resectable if there is (1) severe unilateral or bilateral superior mesenteric vein (SMV) or portal vein impingement, (2) less than 180° tumor abutment of the superior mesenteric artery (SMA) or celiac trunk, (3) abutment or encasement of the hepatic artery, if reconstructable, or (4) SMV occlusion, if of a short segment, and reconstructable. Although helpful, the use of the term “severe impingement” is troublesome in that it is difficult to precisely quantify. Investigators at MD Anderson Cancer Center have used a similar definition : tumor abutment (180° or less of the circumference) of the SMA or celiac axis; tumor abutment or encasement (>180° of the circumference) of a short segment of the hepatic artery; or short-segment occlusion of the SMV, portal vein, or superior mesenteric vein pressure confluence that was amenable to vascular resection and reconstruction. This definition does not include a degree of involvement or encasement of the SMV but rather relies on the reconstructability of the vessel.
In an attempt to standardize the definition of resectable and borderline resectable lesions, the American Hepatopancreaticobiliary Association held a consensus conference for which the summary statement has been recently published. According to this consensus statement, borderline resectable lesions include (1) those without distant metastases; (2) venous involvement of the SMV or portal vein demonstrating tumor abutment with or without impingement and narrowing of the lumen, encasement of the SMV/portal vein but without encasement of nearby arteries, or short-segment venous occlusion resulting from either tumor thrombus or encasement but with suitable vessel proximal and distal to the area of vessel involvement, allowing for safe resection and reconstruction; (3) gastroduodenal artery encasement up to the hepatic artery with either short-segment encasement or direct abutment of the hepatic artery, without extension to the celiac axis; and (4) tumor abutment of the SMA not to exceed more than 180° of the circumference of the vessel wall. This definition does a good job in attempting to define vascular involvement more precisely, and it is hoped that this definition will be widely used in future trials and studies.
Results of Neoadjuvant Therapy for Borderline Disease
Studies thus far investigating the role of neoadjuvant therapy for borderline resectable lesions ( Table 4 ) have used neither a universal definition nor a preoperative staging and workup. As a result, borderline resectable lesions have often been included in resectable neoadjuvant trials and studies of LA (unresectable) disease. This is clearly evident from the large variability in results, including response and resectability rates, and survival rate. For example, the trial reported by Yeung and colleagues and the ECOG phase 2 trial reported by Hoffman and colleagues, as discussed earlier, included patients with LA disease and resectable disease. As seen in Table 4 , there is a wide variety of resection rates ranging from 1% to as high as 76% and response rates from 3% to 50% regardless of the regimen used. The main reason for such discrepancies, as discussed earlier, is most likely the varying and often subjective definitions of resectability. For example, in the study from Memorial Sloan-Kettering Cancer Center, the criteria for unresectability were strict; patients with localized SMV or portal vein involvement were considered resectable, and only patients with extensive retropancreatic venous involvement or encasement of the celiac axis, hepatic artery, or SMA were included in the study. In contrast, in the study by Allendorf and colleagues in which the conversion rate of 76% was extraordinarily high, 43% of the patients had invasion of the splenic vein/portal vein only, a criterion that may be considered resectable by some, and 16% had short-segment venous occlusion or less than 180° arterial abutment, which is considered borderline resectable by many. In addition, patients were deemed LA either by various radiographic studies (61%) or by previous surgical exploration (39%). Fifty-seven percent of the patients noted to be unresectable at exploration had their exploration at various outside institutions. Despite these limitations, however, if one looks at the median survival of the patients ultimately undergoing resection, it is evident that long-term survival is possible in select patients with LA disease who respond or stabilize with the use of neoadjuvant therapy and undergo successful resection.