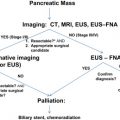
Borderline resectable pancreatic cancer is an emerging stage of disease defined by computed tomogrpahy criteria, patient (Katz type B), or disease characteristics (Katz type C). These patients are particularly well suited to a surgery-last strategy with induction therapy consisting of chemotherapy (gemcitabine alone or in combination) followed by chemoradiation. With appropriate selection and preoperative planning, many patients with borderline resectable disease derive clinical benefit from multimodality therapy. The use of a standardized system for the staging of localized pancreatic cancer avoids indecision and allows for the optimal treatment of all patients guided by the extent of their disease. In this article, 2 case reports are presented, and the term borderline resectable pancreatic cancer is discussed. The advantages of neoadjuvant therapy and surgery are also discussed.
Case reports
Case 1
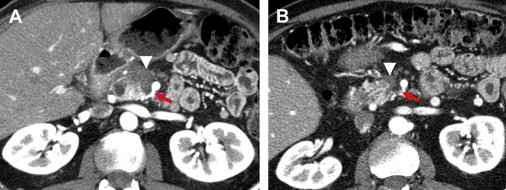
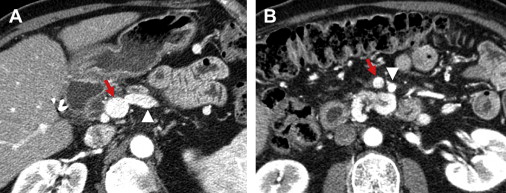
A 63-year-old man who was otherwise healthy presented with epigastric pain and new onset diabetes. The diagnosis of pancreatic adenocarcinoma was established following endoscopic ultrasound (EUS)-guided fine-needle aspiration (FNA) biopsy. The patient was treated with standard fractionation 5-fluorouracil-based chemoradiation for presumed locally advanced, inoperable pancreatic cancer. Thereafter, he received additional systemic therapy (gemcitabine and cisplatin) while he sought opinions from various medical centers regarding the resectability of his primary tumor. After neoadjuvant therapy his status on the Eastern Cooperative Oncology Group (ECOG) performance scale was 0 to 1, he was not jaundiced, and he had no signs of gastric outlet obstruction. Serum carbohydrate antigen 19-9 (CA 19-9) went from 77 U/mL before neoadjuvant therapy to 8.9 U/mL after therapy. On repeat computed tomography (CT) ( Figs. 1 and 2 ) the tumor did not extend to the celiac axis or the hepatic arteries, but there was tumor abutment (≤180° of tumor artery contact) of the superior mesenteric artery (SMA). A short-segment occlusion of the confluence of the superior mesenteric vein (SMV) and the portal vein (PV) was present at the splenic vein junction; however, there was a normal PV cephalad to the obstruction and a normal SMV caudal to the area of occlusion. The jejunal branch of the SMV was inseparable from the caudal extent of the tumor, but the ileal branch diameter was adequate for grafting.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree