Abstract
Over the past 30 years, new and advanced breast cancer multimodality treatments have resulted in improved median survival times for patients with metastatic breast cancer. Breast cancer most commonly metastasizes to bone, followed by lung, brain, and liver. Until now, the treatment focus for metastatic breast cancer has been on palliative care rather than cure. However, a more aggressive treatment approach may be appropriate for patients with metastatic disease limited to a solitary lesion or to multiple lesions at a single organ site. Improved diagnostic, staging, and surgical techniques may allow curative surgery in these carefully selected patients with acceptable morbidity and very low mortality. In addition, studies have shown that the molecular phenotype of breast cancer determines the timing, pattern, and outcome of metastatic disease, and metastatic lesions may alter their receptor expression profile from their primary tumor. The main goal of such curative surgery would be prolonged disease-free survival and improved quality of life. Provided that the breast cancer primary is controlled, there is a long disease-free period, and the patient has a good performance status, surgery is an important component in the multimodality approach to breast cancer solitary metastases.
Keywords
breast cancer, solitary metastasis, metastasectomy, stage IV breast cancer
Over the past 30 years, new and advanced breast cancer multimodality treatments have resulted in improved median survival times for patients with metastatic breast cancer. Breast cancer most commonly metastasizes to bone, followed by lung, brain, and liver. Until now, the treatment focus for metastatic breast cancer has been on palliative care rather than cure. However, a more aggressive treatment approach may be appropriate for patients with metastatic disease limited to a solitary lesion or to multiple lesions at a single organ site. Improved diagnostic, staging, and surgical techniques may allow curative surgery in these carefully selected patients with acceptable morbidity and very low mortality. In addition, studies have shown that the molecular phenotype of breast cancer determines the timing, pattern, and outcome of metastatic disease and metastatic lesions may alter their receptor expression profile from their primary tumor. The main goal of such curative surgery would be prolonged disease-free survival (DFS) and improved quality of life. Provided that the breast cancer primary is controlled, there is a long disease-free period, and the patient has a good performance status, surgery is an important component in the multimodality approach to breast cancer solitary metastases.
Liver
The liver is an uncommon site for solitary first metastasis in breast cancer, having been reported to occur only 3% to 9% of the time. Eventually, breast cancer liver metastases are found in 55% to 75% of autopsies performed on patients who died of breast cancer. Hepatic metastases usually occur at later stages of disseminated disease and carry a poor prognosis, with a median survival of 6 months. These patients are not candidates for resection and can be treated only with systemic therapy. Even with systemic chemotherapy, the median survival for patients with metastatic disease to the liver only or with limited disease elsewhere is approximately 19 months, using pretaxane chemotherapy regimens or 22 to 26 months with taxane-containing regimens. Hormonal therapy is generally of limited use because most hepatic metastases are hormone receptor–negative; however, estrogen receptor–positive hepatic metastasis is not a rare phenomenon. Hence, surgery has been proposed as a potential therapeutic tool for increasing survival in patients with isolated liver metastasis.
Abbott and colleagues from the MD Anderson Cancer Center studied their institutional experience with 86 breast patients with metastases limited to the liver who underwent hepatic resection. The primary aims were to document overall survival (OS) and DFS and to identify predictors of survival that could be assessed preoperatively to optimize patient counseling, risk-benefit analyses, and outcome. Fifty-nine patients (69%) had estrogen receptor– or progesterone receptor–positive primary breast neoplasms. Fifty-three patients (62%) had a solitary breast cancer liver metastasis, and 73 (85%) had breast cancer liver metastases 5 cm or smaller. Sixty-five patients (76%) received prehepatectomy hormonal and/or chemotherapy. Four patients (6%) had progressive disease as the best response, and 19 patients (30%) had progressive disease before hepatectomy ( p < .001). Seventy percent of patients who received preoperative chemotherapy or hormonal therapy had either response or stable disease immediately before hepatectomy. No postoperative deaths were observed. At a 62-month median follow-up, the DFS and OS were 14 and 57 months, respectively. On univariate analysis, estrogen receptor/progesterone receptor status of the primary breast neoplasm, best radiographic response, and preoperative radiographic response were associated with overall survival. On multivariate analysis, estrogen receptor–negative primary breast disease and preoperative progressive disease were associated with decreased overall survival. From their study, they concluded that resection of breast cancer liver metastases in patients with estrogen receptor–positive disease that is responding to chemotherapy is associated with improved survival. The timing of operative intervention may be critical; resection before progression is associated with a better outcome.
Van Walsum and colleagues on behalf of the Dutch Liver Surgeons Group evaluated the effectiveness and safety of resection of liver metastasis from breast cancer and to identify prognostic factors for overall survival. A total of 32 female patients were identified. Intraoperative and postoperative complications occurred in 3 and 11 patients, respectively. There was no postoperative mortality. After a median follow-up period of 26 months, 5-year and median OS after partial liver resection was 37% and 55 months, respectively. The 5-year DFS was 19% with a median time to recurrence of 11 months. Solitary metastases were the only independent significant prognostic factor at multivariate analysis. Van Walsum and collaborators concluded that resection of liver metastases from breast cancer is safe and might provide a survival benefit in a selected group of patients. Especially in patients with solitary liver metastasis, the option of surgery in the multimodality management of patients with disseminated breast cancer should be considered.
Adam and associates offered hepatic resection to all patients with breast cancer liver metastases, provided that curative resection was feasible and extrahepatic disease was controlled with medical and/or surgical therapy. The outcomes of 85 consecutive patients with breast cancer liver metastases treated from 1984 to 2004 were reviewed. Breast cancer liver metastases were solitary in 38% of patients and numbered more than three in 31%. After a median follow-up of 38 months, the median and 5-year survivals were 32 months and 37%. Median and 5-year DFS were 20 months and 21%. Study variables associated with a poor survival were failure to respond to preoperative chemotherapy, an R2 resection, and the absence of repeat hepatectomy. In addition, patients who were treated with repeat hepatectomy had a higher 5-year overall survival rate (81%), compared with patients with unresectable liver recurrences and patients without any hepatic recurrence after first hepatic resection but with extrahepatic metastatic disease. Their analysis determined that DFS was not an independent prognostic factor. Interestingly, the median survivals were longer in the group of patients treated from 1994 to 2004 versus 1983 to 1993. This improved survival might be a reflection of better diagnostic technology and surgical techniques. Adam and investigators concluded that favorable outcomes can be achieved even in patients with medically controlled or surgically resected extrahepatic disease, indicating that surgery should be considered more frequently in the multidisciplinary care of patients with breast cancer liver metastases.
Patient selection and operative criteria for hepatic resection are still controversial; however, important criteria are likely to be fewer than four metastases, no extrahepatic disease, and demonstrated disease regression or stability with systemic therapy before resection. At a minimum, a patient should have a normal performance status and normal liver function tests. Pocard and Selzner agreed that the size and number of hepatic metastasis was an important factor. Patients in whom liver metastasis was found more than 1 year after resection of the primary cancer had a significantly better outcome than those with early (<1 year) metastatic disease. The type of liver resection, the lymph node status at the time of the primary cancer resection, and the use of neoadjuvant high-dose chemotherapy had no significant impact on patient survival in their series. Martinez and coworkers showed that survival was greater in patients with estrogen receptor–positive primary tumor and metastases, HER2/neu-positive metastases, two or fewer metastases, and age greater than 50 years at metastasectomy.
The preference is for patients to receive chemotherapy before hepatic resection. Extensive preoperative staging evaluation before considering hepatic resection for breast cancer liver metastases is recommended. Diagnostic laparoscopy is recommended to avoid a nontherapeutic laparotomy if extrahepatic disease based on preoperative imaging is suggested. Hepatic resection is preferable if metastases can be safely removed with a negative surgical margin. Radiofrequency ablation should be reserved for those patients with tumors not amenable to safe resection or used as an adjunct to resection. Radiofrequency ablation has been used for local control of breast cancer liver metastasis (BCLM); the reported series show a median survival of between 30 and 60 months, with no treatment-related deaths and only three serious treatment-related adverse events in 164 patients reported. Despite this, skepticism remains over the efficacy of BCLM ablation due to the heterogeneity of patient inclusion and selective nature of reporting. Randomized trials are needed to formulate robust evidence-based recommendations and direct the necessary allocation of health care resources. Transarterial catheter embolization has emerged as a potential treatment option for direct liver delivery and possible better systemic toxicity profile.
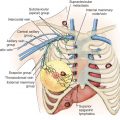
Lung
Isolated lung metastases have been reported to occur in 10% to 20% of all women with breast cancer. Approximately 3% of all women with breast cancer develop a solitary pulmonary lesion detectable by chest radiograph, of which 33% to 40% are breast metastases. Considering the low morbidity and mortality rate, lung metastasectomy is the best treatment option in selected patients with lung metastases from breast cancer.
Meimarakis and colleagues investigated whether OS in patients with primary breast cancer is prolonged by pulmonary metastasectomy and which prognostic criteria may facilitate the decision in favor of thoracic surgical intervention. The study assessed the median OS of 81 women after resection of pulmonary primary breast cancer metastases and matched patients who had not undergone resection from the Munich Tumor Registry served as controls.
In 81.5% of the patients R0 resection was achieved, which was associated with significantly longer median OS than occurred after R1 or R2 resection (103.4 months vs. 23.6 months vs. 20.2 months, respectively; p < .001). Multivariate analysis revealed R0 resection, number (n ≥ 2), size (≥3 cm), and estrogen receptor and/or progesterone receptor positivity of metastases as independent prognostic factors for long-term survival. Presence of metastases in mediastinal and hilar lymph nodes correlated with decreased survival only in the univariate analysis. Matched pair analysis confirmed that pulmonary metastasectomy significantly improved survival. The investigators concluded that OS in patients with isolated pulmonary primary breast cancer metastasis is prolonged by metastasectomy. Patients with multiple pulmonary lesions or metastases with negative hormone receptor status are at greater risk of disease relapse and should be followed closely. Moreover, additive treatment tailored to the biological subtype defined by hormone receptor expression should be considered for this group.
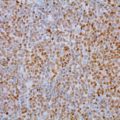
Resection of pulmonary metastases is a common treatment in other primaries, but the role of breast cancer metastasectomy is still unclear. Welter and colleagues investigated the clinical outcome of operated patients with pulmonary breast cancer metastases and the different indications for metastasectomy. Retrospective analysis of 47 patients with histologically proven pulmonary metastases from breast cancer showed the grading of the metastases was higher than the primary tumor in 26.7% and lower in 13.3% patients. R0, R1, and R2 resections were achieved in 27, 6, and 14 cases. The estrogen receptor status of the metastases differed from the primary tumor in 28.2% tested cases. HER2/neu receptor status differed in 4 of 16 tested patients. The histologic reports described a tumor spread around the metastasis in lymph or blood vessels in at least one resection specimen in 53.2% patients. The rate of major complications was 5.8%. The OS from the first pulmonary metastasectomy was 32 months with a 5-year survival of 36%. The main prognostic factor was the estrogen receptor status with a 5-year survival for receptor positive patients of 76% and 12.1% for receptor negative ones ( p = .002). A similar survival difference was found for the status of HER2/neu receptor ( p = .037). No prognostic influence could be demonstrated for age, number of metastases, initial tumor stage, complete versus incomplete resection, lymphatic spread, or lymph node or parietal pleural involvement. Welter and colleagues concluded that the gain in life expectancy in breast cancer patients with pulmonary metastases is based on chemotherapy and antihormone treatment. Tissue of the lung metastasis is needed to adjust medical therapy to estrogen receptor and HER2/neu expression and to reliably rule out primary lung cancer. In case of proven pulmonary metastases, the level of evidence for a curative approach is low, but some patients might benefit.
Friedel and colleagues evaluated the data from the International Registry of Lung Metastasis, including 467 patients who had lung metastases from breast cancer, with regard to long-term survival and prognostic factors. In 84%, a complete resection was possible, with 5-, 10- and 15-year survival rates of 38%, 22%, and 20%, respectively. Positive prognostic factors were a disease-free interval of longer than 36 months, with 5-, 10-, and 15-year survival rates of 45%, 26%, and 21% respectively. Solitary lung metastasis was associated with a survival rate of 44% after 5 years and 23% after 10 and 15 years, but this was not statistically different compared with the outcome of patients undergoing resection of multiple metastases. In the Friedel study, there were no significant differences between the kind of resection used (wedge or segmental resection, lobectomy, pneumonectomy) in completely resected patients.
Kycler and associates reviewed retrospectively data for 33 patients who underwent 43 curative resections of breast cancer pulmonary metastases. Potential prognostic factors affecting survival, namely survival after lung metastasectomy, assessed were disease-free interval (DFI), the number and location of lung metastases, the diameter (in millimeters) of metastases, and the extent of pulmonary resection. The median survival for 33 patients with pulmonary breast cancer metastatic lesions after metastasectomy was 73.2 months. Mean 5-year survival was 54.5%. There was a statistically significant difference in survival time with better prognosis for patients with DFI greater than 36 months ( p = .0007), complete metastasectomy ( p = .0153), unilateral pulmonary metastases ( p = .0267), and for patients who underwent multiple operations ( p = .0211). In multivariate analysis, there was significant influence for long-term prognosis for patients with DFI greater than 36 months ( p = .0446) and for complete resection of the metastases ( p = .0275). Analysis of the survival rates for patients with solitary pulmonary metastasis, with different size of tumors and after different types of pulmonary resection showed no significant differences. It was concluded that resection of lung metastases from breast cancer may offer a significant survival benefit for selected patients. The identified prognostic factor for survival after metastasectomy is DFI longer than 36 months and complete resection of the metastases. Also, the results showed that lung metastasectomy by conventional surgery is a safe procedure with low perioperative morbidity and mortality rate. Significant prognostic factors associated with survival include the number of metastases, DFI longer than 12 months, and complete resection. Yoshimoto and coworkers demonstrated that the surgical approach to lung metastases from breast cancer may prolong survival in certain subgroups of patients to a greater extent than with systemic therapy alone. In addition, survival times were significantly longer for patients who initially presented with clinical stage I at breast surgery than those with stage II to IV.
As part of the metastatic workup, it is important to obtain histologic diagnosis and differentiate between a metastatic lesion and a primary lung cancer. Early identification of the tumor is critical for appropriate treatment strategies. Proper aggressive evaluation can afford treatment of lung cancer and influence survival. Rena and colleagues studied the role of surgery in the diagnosis and treatment of a solitary pulmonary nodule (SPN) in patients who had received previous surgery for breast cancer. A total of 79 consecutive patients between 1990 and 2003 who had previously undergone curative resection for breast cancer and subsequently underwent surgery for an SPN were reviewed. Surgical diagnosis was obtained by open procedure before 1996 (37 cases), as well as by video-assisted thoracoscopic surgery (VATS) after 1996 (33 of 42 cases, nine open procedures) and intraoperative evaluation. Histology of SPN was primary lung cancer in 38 patients, pulmonary metastasis of breast cancer in 27, and benign condition in 14. The researchers concluded that VATS is a good procedure for diagnostic management and pathologic confirmation of peripheral SPN to determine appropriate surgical treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree