9912
Social Isolation and Caregiver Burden
Linda Mathew and Carolyn Fulton
INTRODUCTION
More than 16 million Americans are currently living with a diagnosis of cancer; accordingly, the need for cancer caregiving have increased. Shorter hospital stays and the transition of cancer treatment to the ambulatory setting have only added to the complexity of this burden. Despite this fact, caregiver burden is greatly underidentified by medical professionals. Generally speaking, more women than men become caregivers and most caregivers are aged 55 years or older (1,2). Caregiving seems to affect genders differently. Women are at greater risk for isolation, loneliness, and decreased satisfaction and men are at greater risk of psychological distress (3).
CAREGIVER ROLE
The caregiver is defined as the primary person upon whom the patient relies for assistance with physical care, symptom management, and psychosocial needs and who does not receive financial remuneration for caregiving (4). The caregiver is not always a blood relative or a household member. Caregiving can be related to bonds of attachment and can be affected by cultural norms or feelings of guilt and obligation. Because many cancer patients are living longer due to improved treatments, the emotional implications of long-term caregiving are significant.
THE BURDEN OF CAREGIVING
Caregiver burden is the result of caring for someone with a chronic illness. Caregivers have their own emotional responses to patients’ diagnoses and prognoses, and they may require problem-solving and emotional support separate from that offered to patients. Caregivers are often balancing work and family demands, along with emotional, physical, financial, and spiritual distress, as they help patients cope with cancer. Caregiver roles and caregiver burden are profoundly affected by a patient’s prognosis, stage of illness, and goals of care. The physical and emotional demands of caregiving reach their peak as the disease progresses to the end-of-life phase. In the context of recurrent and advanced illness, the caregiver must meet a new set of challenges 100in dealing with increasing functional limitations and increasing dependence of the patient, as well as greater need for symptom management (4). In addition, uncertainty is a constant companion throughout all stages of disease. The trajectory of cancer is fraught with uncertainty and inflicts turmoil on everyday life. This uncertainty can increase caregivers’ anxiety and stress levels, which in turn can impact the burden they feel placed on them. The high stress associated with this uncertainty, the demands of multiple medical appointments, and the physical needs of the patient add to this increased physiological and psychological burden as well. Acknowledgment of caregiver burden is often overlooked by clinicians who are treating the patients.
For cancer patients’ caregivers, psychological and physical outcomes are mediated by the juxtaposition of the caregiver burden with the positive aspects of the role. Caregiver burden is associated with inadequate information and education, the disruptions it can cause to daily life, and the restrictions it imposes on outside activities that lead to social isolation (5). The physical effects in caregivers include behaviors such as not getting enough rest or exercise and neglecting their own health, which can sometimes mimic depression (6). The financial consequences of caregiving can include lost salaries, insurance deductibles, copayments, and uncovered services such as transportation and home care. Patients and caregivers have parallel spiritual tasks when dealing with cancer, such as finding meaning and hope in the disease process while also examining existential questions about life. As mentioned earlier, there are positive aspects to the role of caregiving, which can function as an opportunity for growth and satisfaction. It allows caregivers to become closer to the ones they are caring for, to repay care that they may have received earlier, can increase intimacy, and often provides an increased sense of purpose or meaning.
CAREGIVER-PATIENT DYAD EFFECTS ON CARE
An aspect that must be addressed is the parallel relationship that exists between caregivers’ and patients’ physical and emotional reactions to cancer. There is limited research focusing on this specific relationship, although a few studies have found that caregiver-patient responses to cancer were interdependent: each person affected the other’s level of emotional and physical well-being (5). The research proposed that specific interventions can significantly improve patients’ and caregivers’ physical health, mental health, and communication and at the same time improve the caregivers’ knowledge, preparedness, self-efficacy, and coping (7). Some interventions that were identified to help improve physical and emotional responses included: (a) psychoeducation that provides information about management of patient’s symptoms, physical aspects, and emotional aspects of care; (b) skills training that addresses the development of caregivers’ coping, communication, and problem-solving skills; and (c) therapeutic counseling that focuses on strengthening the patient-caregiver relationship.
SOCIAL ISOLATION
In a review of both geriatric and oncology literature, social isolation has been linked to an increased risk of mortality (8,9). Caregivers must cope with the combined challenge 101of aging and illness when they experience personal losses, such as a family member or friend. Caregivers can experience isolation from their social networks. Studies have shown that more than half of caregivers reported reduced socializing with others because of the demands of caregiving, and a lack of satisfaction with perceived levels of social support (10). This lack of social support is attributed to the older caregivers becoming enmeshed in the care situation; by doing so, they isolate themselves from social and family roles and are consumed with providing care. Caregivers also have limited time to engage in activities outside of the caregiving role, particularly when they are the only person available for the patient. This decrease in social activities also produces a sense of interpersonal loss for the caregiver and can lead to a lack of intimacy and affection; increased symptoms of depression and increased feelings of resentment can also occur (11). Caregivers speak about feeling very alone in the caregiving role even when they are engaging with family, friends, and members of their community (12).
A further element of social isolation in the context of caring for an older loved one is the inability to provide care in other areas of the caregiver’s life. Many caregivers have partners and children, but because of the multiple demands primary caregivers have to manage, primary caregiving does not allow them to fully be present for any of their various roles. The inability to fully commit can increase feelings of stress, anxiety, anger, resentment, and extreme sadness (13). Unfortunately, these constraints, along with multiple levels of social isolation, make it difficult for caregivers to work on familial relationships. These tensions can manifest in the therapeutic setting, where it can be helpful to identify and normalize these challenging circumstances associated with caregiving.
One last component of social isolation relates to siblings or other family members. Caregivers may have to negotiate with siblings and family members in order to make medical decisions. This pressure often adds to the primary caregiver’s distress and increases isolation, as the negotiation process can create challenges to relationships and communication within the family system (14).
The social impact of cancer and pain can be ameliorated by social support, financial security, and stability at work. It is clear that caregivers need guidance on how to respond to each of these elements of social support.
IMPLICATIONS FOR HEALTH CARE PROVIDERS
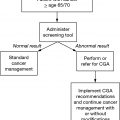
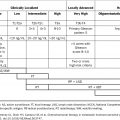
As the population continues to age, it will be crucial that we identify older adults who are caring for a patient with cancer. Integrating a geriatric caregiver assessment (see Box 12.1) at the initial patient visit might provide a way to identify those who have the greatest need (15). The complexities associated with loneliness, social isolation, and caregiver burden are all interconnected and must be supported and understood by medical professionals. The nature and quality of the preexisting patient-caregiver relationship are important considerations in the assessment and treatment of caregiver burden. If the impact of cancer caregiving is identified and assessed early on in the treatment trajectory, effective interventions to meet the needs of caregivers can be implemented.
102BOX 12.1: Fundamental Principles for Caregiver Assessment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree