19521
Pancreatic Cancer
Elizabeth Won
INTRODUCTION
In the United States, more than 48,000 patients are diagnosed with pancreatic cancer annually, and it is the fourth most common cause of cancer death. Pancreatic cancer is a disease occurring in older adults, with a median age of 71 years at diagnosis and highest incidence among patients age 75 to 84 years (1). However, older patients are less likely to be recommended for surgery and less likely to receive chemotherapy compared with younger patients (2). Clearly, patient-related factors such as comorbidities, functional status, and limited social support affect the ability to deliver and tolerate treatment and thus have a direct effect on the survival of older adults. However, there are data that elderly patients have a lower likelihood of being offered treatment based on age alone (3,4). This review evaluates the current knowledge and the remaining challenges in optimal management of elderly patients with pancreatic cancer.
TREATMENT OF EARLY STAGE PANCREATIC CANCER IN OLDER PATIENTS
Surgery for Pancreas Cancer
The only potentially curative approach for pancreatic cancer is surgical resection. Only 15% to 20% of all patients are candidates for pancreatomy or pancreaticoduodenectomy (Whipple procedure), which is a complex, invasive procedure with high rates of morbidity and mortality. Older patients are less likely to undergo surgery. A study examining the Surveillance, Epidemiology, and End Results (SEER) database for treatment of pancreatic cancer between 1983 and 2007 showed that for patients older than 70 years, the odds of surgery being done were 55% less than for younger patients (4). Single institution reports have demonstrated that Whipple surgery can be performed safely in patients aged 80 years and above (5–7), with lower mortality rates seen at high-volume institutions. However, nationally operative mortality (death before hospital discharge) has been shown to increase proportionally with age: 6.7% of patients aged 65 to 69 years, 9.3% of patients aged 70 to 79 years, and 15.5% of patients aged 80 years or older (8). Unfortunately, the 5-year survival for localized pancreatic cancer remains very poor, approximately 29%, and therefore the benefit of surgery must be weighed carefully with the risks (9).
In a study by Tan et al., the authors examined a national database for the presence of geriatric events after surgery in patients over the age of 65 (10). These events included 196dehydration, delirium, falls, fractures, failure to thrive, and pressure ulcers, which are not commonly reported in the surgical literature. A quarter of all patients undergoing pancreatic cancer surgery experience a geriatric event, with even higher rates seen in those aged 75 years or older. These geriatric events were associated with prolonged hospitalization (odds ratio [OR] 5.97; 95% confidence interval [CI] 5.16–5.80) and higher cost (OR, 4.97; 95% CI 4.58–5.39). This is consistent with the surgical literature reporting higher postoperative complications and longer hospitalizations in older patients (11,12). Furthermore, discharge to an inpatient nursing facility increases from 10.6% to 36.7% when comparing patients aged 65 to 69 to those 80 years and older (8).
There are conflicting data about the overall prognosis after pancreatic surgery, with some studies suggesting decreased overall survival (OS) in older patients (8,13,14). Sho et al. showed median survival of 16.6 months in patients aged 80 years and above compared to 23.2 months in younger patients, with worse disease-specific survival in the older patient group (P = .013) (15). Multiple factors likely play a role in the prognosis after surgery, including tumor biology, ability of elderly patients to complete adjuvant chemotherapy, decreased functional reserve, and geriatric syndromes affecting recovery after pancreatic resection.
Preoperative Geriatric Assessment
Comprehensive geriatric assessment (CGA) has the potential to identify those at risk for postoperative complications, functional disability, and cognitive decline and to provide an opportunity to implement interventions and support before, during, and after surgery (16,17). The University of Chicago team prospectively studied the ability of a CGA to predict surgical outcomes in older patients undergoing Whipple surgery (18). A measure of frailty, self-reported exhaustion, which would have not been identified on a traditional preoperative evaluation, was predictive of major surgical complications (OR = 4.06; P = .01), necessity of intensive care unit (ICU) stay (OR = 4.30; P = .01), and length of overall hospital stay (β = 0.27; P = .02).
Postoperative management of elderly surgical patients must be specialized to avoid geriatric events, including delirium, malnutrition, pressure ulcers, falls, infection, functional decline, and polypharmacy. With adequate and collaborative perioperative care between the surgical and geriatric teams, the risk of morbidity and mortality for older patients may be mitigated.
Adjuvant Chemotherapy
Adjuvant chemotherapy has been shown to improve outcomes compared to surgical resection alone in two large phase 3 studies (Table 21.1). There are limited data regarding the number of elderly represented in these trials; however, both studies reported no differences in survival by age in the multivariable analysis. It is important to note that the median age in these trials was 62 and 63 years, respectively, and the median age at the time of diagnosis of pancreatic cancer in the United States is 71 years. Gemcitabine has been the accepted standard adjuvant chemotherapy and should be considered in a fit patient who has recovered from surgery. Significant common toxicities include myelosuppression, fatigue, diarrhea, nausea, decreased appetite, and flu-like symptoms after infusion. There are no data on dose modifications to improve tolerability for older patients and potential impacts on efficacy. For older patients, close weekly monitoring of toxicity with a low threshold for dose adjustments is recommended.
197TABLE 21.1 Adjuvant Chemotherapy Trials for Pancreatic Cancer
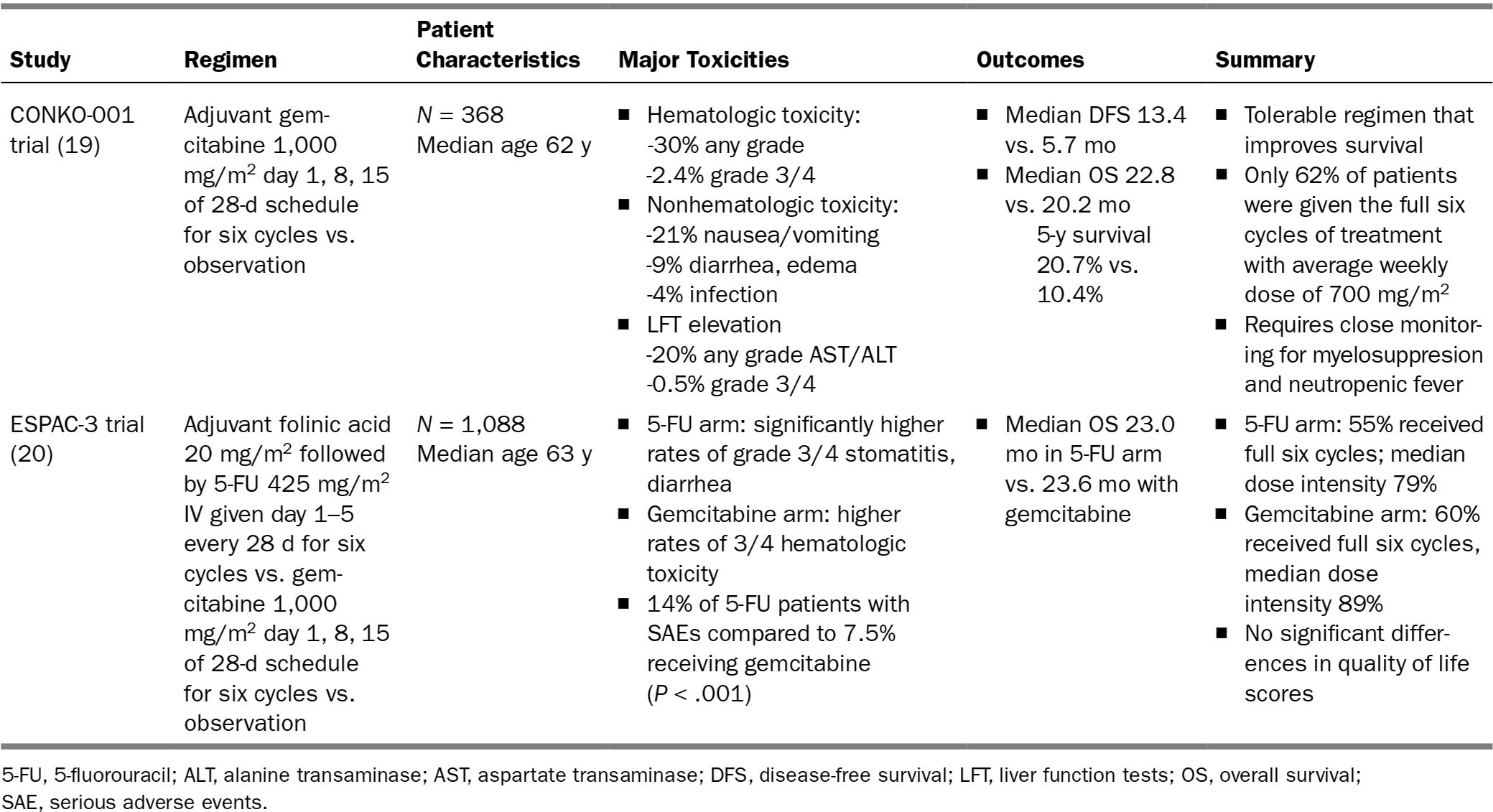
198Although the benefits of adjuvant chemotherapy are evident, the rates of older patients receiving treatment remain low. A SEER analysis showed that less than half of all patients 65 years or older received adjuvant therapy after surgery (21). Not receiving adjuvant chemotherapy has been shown to be an independent poor prognostic factor in older patients. In a community-based cohort, which included 178 patients aged 70 and above, patients who did not receive adjuvant chemotherapy had significantly worse median OS of 13.1 months versus 21.8 months for treated patients (hazard ratio [HR] 1.89, P = .002). In contrast, older patients who did receive adjuvant chemotherapy had similar outcomes to younger patients (21.8 vs. 22.5 months, P = .576) (22). Pancreatic cancer remained the cause of death equally in both groups. Efforts to increase the use of adjuvant chemotherapy in older patients may improve overall outcomes; clearly more research is necessary in this area. Postsurgical geriatric assessments may provide data to better stratify older patients who might benefit from adjuvant therapy.
MANAGEMENT OF ADVANCED/METASTATIC DISEASE
Systemic Chemotherapy
More than half of patients have metastatic disease at the time of diagnosis. The prognosis remains dismal, with a 5-year survival rate of 7% (1). Gemcitabine was considered the standard of care for patients with metastatic pancreas cancer. The MPACT phase 3 trial demonstrated the superiority of gemcitabine and nab-paclitaxel compared with gemcitabine monotherapy, OS 8.5 months versus 6.7 months, respectively, P < .001 (23). The median age of patients in the study was 63 years, with only 42% of patients 65 years of age or older. FOLFIRINOX chemotherapy was compared to gemcitabine monotherapy in the ACCORD-11 trial, showing an OS of 11.1 months versus 6.8 months, P < .001 (24). Treatment-related toxicity for FOLFIRINOX was high, with higher rates of grade 3 or 4 adverse events. This study excluded patients with an Eastern Cooperative Oncology Group (ECOG) score greater than 1 and patients older than 75 years of age. The median age of patients in the study was 61 years, with only 29% of patients between 65 and 75. Although these studies have advanced the treatment options for metastatic pancreatic cancer, the limited representation of older patients in the studies makes it difficult to extrapolate the data to an elderly population.
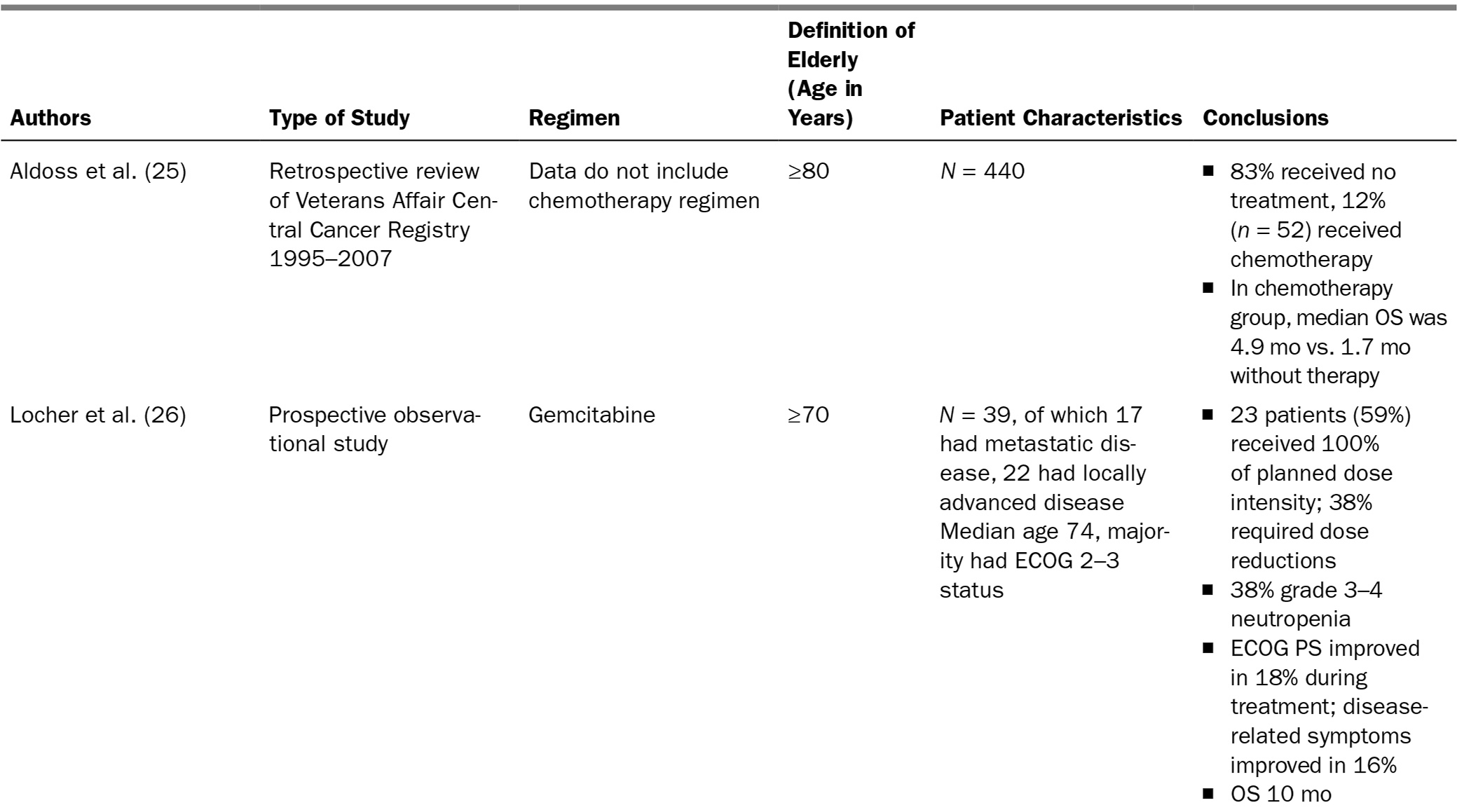
There are few small, mostly retrospective, studies focused on older patients (Table 21.2). These studies suggest not only that chemotherapy is feasible in elderly patients with pancreatic cancer, but also that those with good functional status can obtain palliative benefit comparable to what is seen in younger patients.
There are data showing that dose and schedule attenuations in the combination chemotherapy regimens can reduce side effects without impacting efficacy. A single-institution study revealed that changing the gemcitabine and nab-paclitaxel regimen from weekly to every other week resulted in a median overall survival (OS) of 11.1 months and median progression-free survival (PFS) of 4.8 months. The attenuated schedule reduced the rates of grade 3 neurological toxicity significantly (<2% vs. 17% in the MPACT study) (32). The Memorial Sloan Kettering Cancer Center group has been using FOLFIRINOX with a 20% dose reduction compared to the dosages in the ACCORD-11 trial while showing similar efficacy (median OS 12.5 months) and decreased rates of toxicity reported in the original trial (33).
199TABLE 21.2 Elderly-Specific Trials of Advanced Pancreatic Cancer
200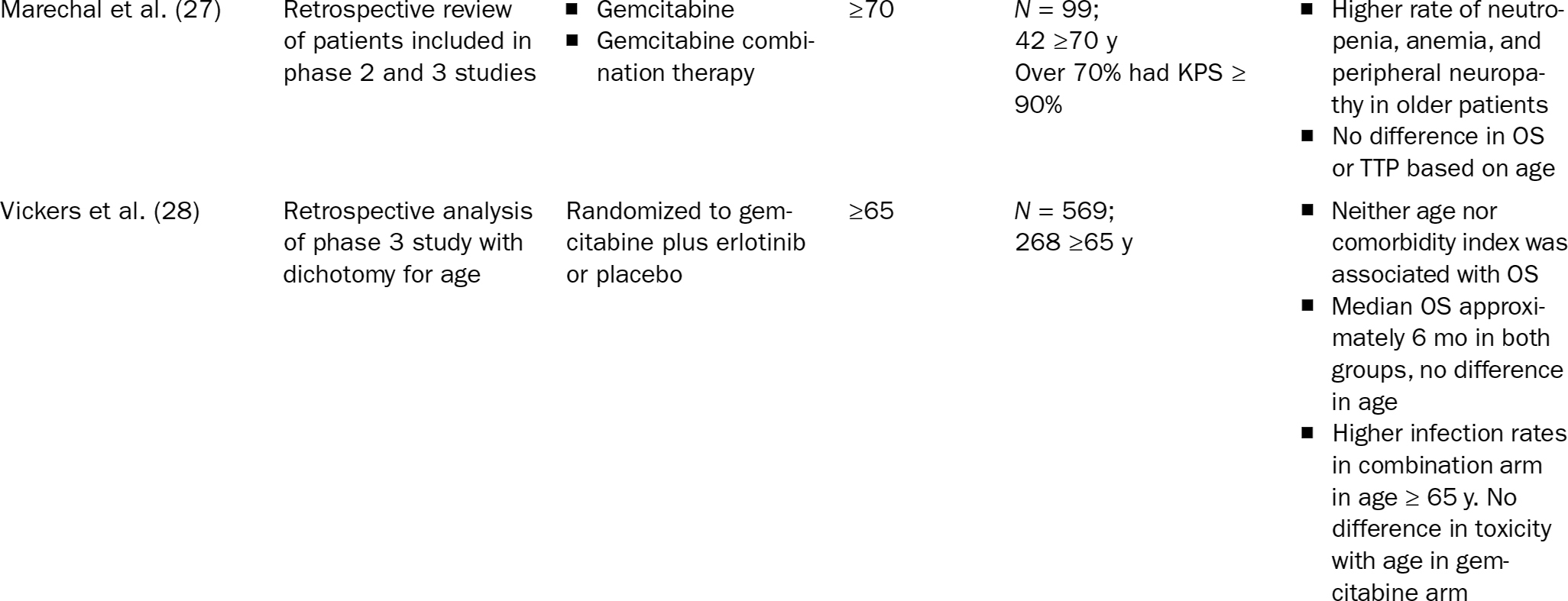
201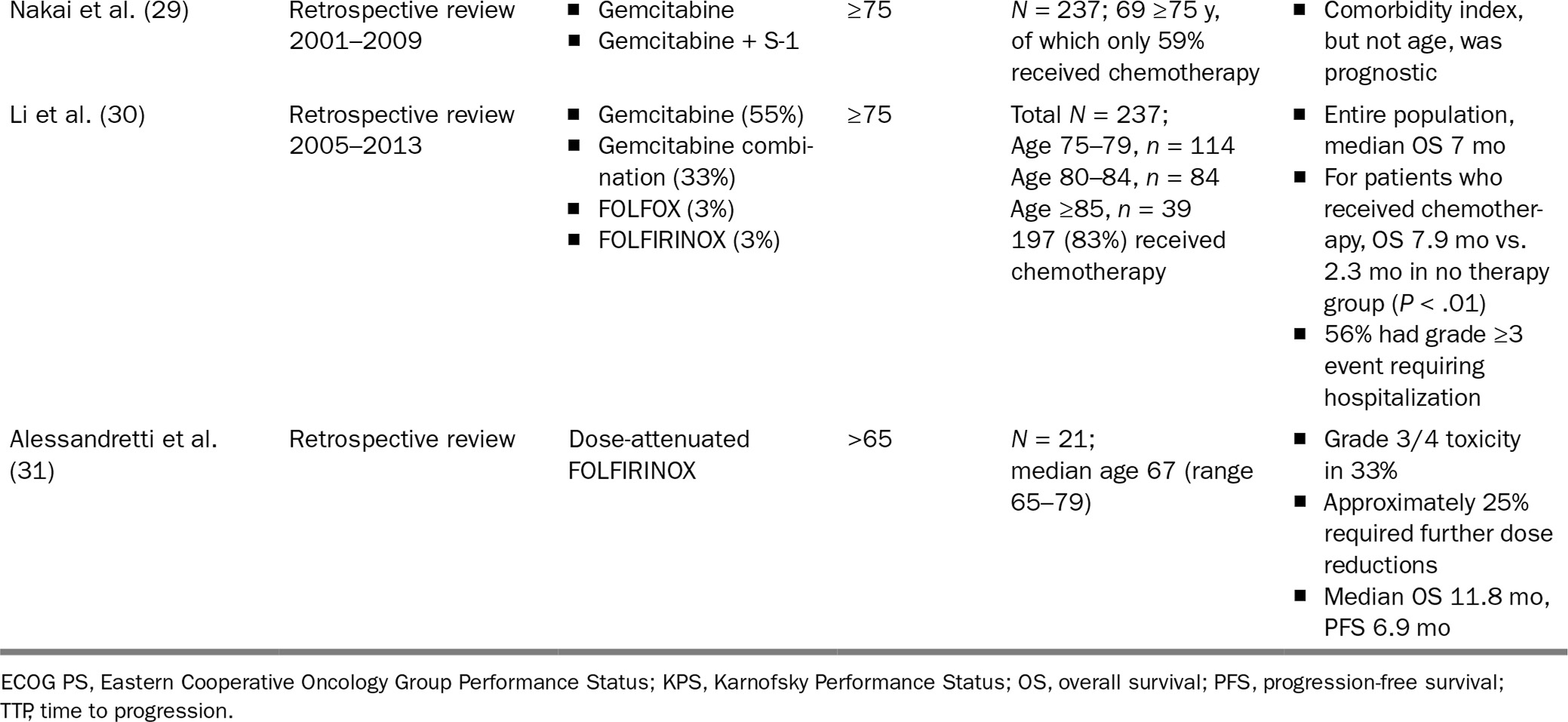
202Considering the data available, a potential algorithm for treatment is proposed in Figure 21.1. For elderly patients who are fully functional and candidates for FOLFIRINOX, dose attenuation is recommended. This proposed algorithm is based on ECOG score, which is commonly used by practicing oncologists to assess patients. There is evidence that ECOG score does not correlate with geriatric assessment results and may misrepresent functional status and/or patient vulnerability to chemotherapy toxicity.
Palliation and Supportive Measures
Patients with advanced pancreatic cancer often present with a high symptom burden, so palliative care is a vital part of the management of these patients. In general, elderly patients with cancer pain are undertreated and many underreport their pain symptoms. Untreated pain can result in worsening of quality of life, depressed mood, and deterioration of functional status (34). Oral narcotics can be very effective for cancer pain control; however, caution should be undertaken to avoid polypharmacy toxicity, delirium, and increasing risk of falls. Another treatment option for control of pain is a celiac block, which may decrease the amount of narcotics necessary. Obstruction is a common complication in pancreatic cancer. Biliary stent placement 203can resolve biliary obstruction in 90% of patients and has been shown to improve quality of life. Duodenal obstructions can be palliated with stents or gastrojejunostomy tubes for comfort. A multidisciplinary approach for addressing the patient’s symptoms, concerns, and personal expectations and goals from the time of diagnosis to end of life is recommended in all pancreatic cancer patients.
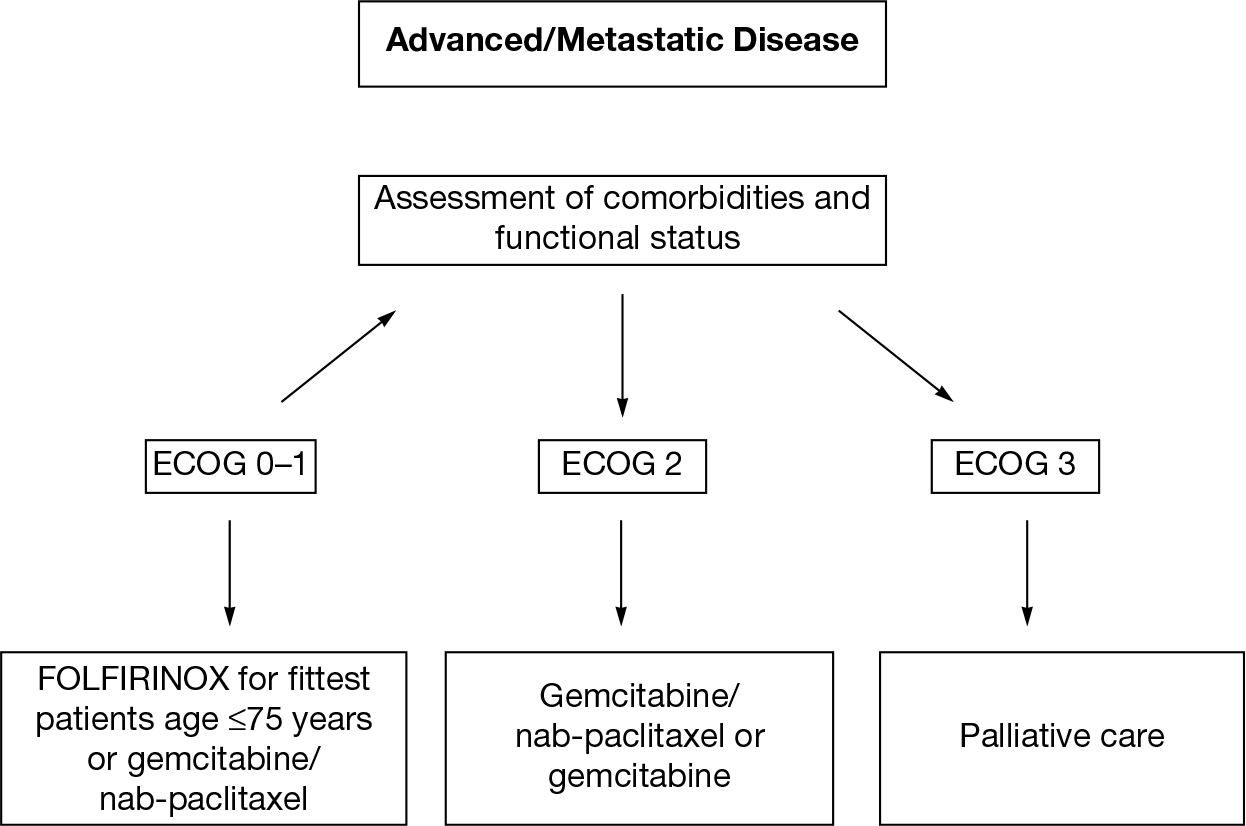
FIGURE 21.1 Choices of chemotherapy regimens for elderly patients with metastatic pancreatic cancer.
ECOG, Eastern Cooperative Oncology Group.
CONCLUSION
As our patient population ages, oncology research and treatment guidelines must adapt accordingly. Age alone should not be the determinant for the selection of patients for treatment in pancreatic cancer. Older patients who receive treatment have improved outcomes similar to those of younger patients. CGAs may help to better tailor treatment approaches in our older patients and provide an avenue for future research into this malignancy.
TAKE HOME POINTS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








