11914
Screening Tools in Geriatric Oncology
Daniel W. Yokom, Cindy Kenis, Shabbir M. H. Alibhai, and Martine T. E. Puts
INTRODUCTION
The current gold standard for assessment of older adults with cancer is a comprehensive geriatric assessment (CGA). A CGA is a multidimensional, interdisciplinary process to determine the medical, psychosocial, and functional capabilities of an older person, with the aim of optimizing health and well-being (1,2). When applied to patients with cancer, CGA has been shown to identify previously unknown health problems, predict treatment-related toxicity, and predict oncologic outcomes, including overall survival and influence of cancer treatment decisions (2–4).
Implementing CGA in an oncology setting is resource intensive, which ultimately limits its widespread use. CGA requires an interdisciplinary team of specialized professionals to perform an assessment that can take up to 1 to 2 hours (5). Given that the majority of oncology patients are over age 65, in most clinical oncology settings it is not practical to perform a CGA for all older patients. Therefore, it has been suggested to restrict the use of CGA specifically to complex older adults (6–8). To select patients who would benefit from a CGA, a number of clinical screening tools have been developed.
The primary purpose of a screening tool in geriatric oncology is to provide a busy clinician with a means to quickly identify patients in need of a CGA. Screening tools are commonly short questionnaires administered by any health care provider, not necessarily a geriatric specialist, and some tools can be administered by the patients themselves (9). CGA assesses multiple domains, commonly: functional status, falls, cognition, mood, comorbidities and polypharmacy, social and financial support, preferences, and goals of care. Conversely, screening tools typically assess only a few domains from the CGA or assess each of the domains superficially. Certain screening tools, including the G8 and Vulnerable Elders Survey (VES-13), have also been assessed for their ability to predict chemotherapy toxicity; however, this is not their primary purpose. More specific chemotherapy toxicity prediction tools have been developed, including the Cancer and Aging Research Group (CARG) tool (10,11) and the Chemotherapy Risk Assessment Scale for High-Age patients (CRASH) score (12). Both the CARG and CRASH 120tools are more accurate at predicting risk of chemotherapy and have been validated in larger prospective cohort studies. CARG and CRASH are discussed further in Chapter 13.
The International Society for Geriatric Oncology (SIOG) provided a consensus statement to recommend the use of screening tools to identify patients who should be further assessed with a CGA. At least 17 different screening tools for older oncology patients have been developed; however, the G8 and VES-13 are the mostly widely studied (9,13). There are a variety of benefits and challenges with each screening tool that must be weighed against one another. No particular screening tool was recommended by SIOG; rather, it is left to the discretion of the health care providers to choose the tool that fits best with their practice model and patient population. The caveat to the SIOG statement is that screening tools cannot replace the CGA: an abnormal screening result should always be followed up with a CGA (9). In this chapter, we:
■ Outline the G8, VES-13, and other screening tools used for older adults with cancer
■ Discuss the evidence for the benefits and limitations of these screening tools
■ Provide recommendations for how to implement geriatric screening tools into routine oncology practice
SCREENING TOOLS
G8
The G8 (Table 14.1) is a screening tool that was specifically developed for use in adults with cancer over age 70 on first-line chemotherapy (14,15). It can be administered by any health care professional and takes about 5 minutes to complete (16). The G8 covers a number of domains from the CGA, including functional capacity, health, nutritional status, and cognitive impairment, as well as self-rated health. The maximum total score for the G8 is 17 and a score of 14 or lower is considered abnormal (14).
Compared to other screening tools, the G8 is one of the most sensitive screening tools; however, it has only modest specificity (9). A systematic review of different screening tests showed that among seven studies on the accuracy of the G8, the average sensitivity was 82.8% (65%–95%) and specificity was 61.1% (3%–75%) (9).Variations of the G8 have been developed to improve the specificity, but these versions have not been widely studied, validated, or accepted in clinical practice (17,18).
When using the G8, it is important to acknowledge a few of its limitations. To begin, the G8 includes a score for “neuropsychological problems.” Although this item is very important, the definition of a neuropsychological problem is open to interpretation and may require further cognitive or psychological assessment or access to prior assessments. Furthermore, the G8 may not yield similar results across tumor types and stages. For example, one study showed that the sensitivity of the G8 was 95% for upper gastrointestinal (GI) cancers whereas it was only 65% sensitive for prostate cancer (19).
121TABLE 14.1 The G8 Screening Tool
Items | Points | |
1 | Has food intake declined over the past 3 months due to loss of appetite, digestive problems, chewing or swallowing difficulties? | 0: severe decrease in food intake 1: moderate decrease in food intake 2: no decrease in food intake 0: weight loss >3 kg |
2 | Weight loss during the last 3 months | 1: does not know 2: weight loss between 1 kg and 3 kg 3: no weight loss |
3 | Mobility | 0: bed- or chair-bound 1: able to get out of bed/chair but does not go out 2: goes out |
4 | Neuropsychological problems | 0: severe dementia or depression 1: mild dementia or depression 2: no psychological problems |
5 | BMI (weight [kg]/height [m²]) | 0: BMI < 19 1: BMI = 19 to BMI < 21 2: BMI = 21 to BMI < 23 3: BMI = ≥ 23 |
6 | Takes more than three medications per day | 0: yes 1: no |
7 | In comparison with other people of the same age, how does the patient consider his or her health status? | 0: not as good 0.5: does not know 1: as good 2: better |
8 | Age | 0: >85 1: 80–85 2: <80 |
TOTAL SCORE | 0–17 | |
Abnormal score | ≤14 |
BMI, body mass index.
Source: Ref. (15). G8 screening tool. Available at: http://siog.org/content/comprehensive-geriatric-assessment-cga-older-patient-cancer.
122In addition to being used as a screening tool, the G8 has also been studied to predict the following:
1. Treatment toxicity: Several studies assessing its usefulness in predicting chemotherapy-related toxicity have shown mixed results (20,21).
2. Functional decline and falls: Two prospective studies have shown that an abnormal G8 is predictive of falls or functional decline within 3 months of a cancer treatment decision (22,23).
3. Overall survival: Multiple studies have determined that an abnormal G8 is associated with worse overall survival compared to patients with a normal G8 (16,19,22).
Although the G8 requires some experience to administer correctly, it is an effective, highly sensitive tool to predict for an abnormal CGA.
Vulnerable Elders Survey-13
The VES-13 (Table 14.2) was originally designed to assess adults over age 65 living in the community who were at increased risk of functional decline (24,25). Domains of the CGA included in the VES-13 are limited to functional capacity, although this is covered in more detail than the G8. Self-reported health and age are also included. The maximum score is 10, with a score of 3 or higher considered abnormal. Notably, an age of 85 or older scores 3 points, which automatically puts those patients into an abnormal range.
Unlike most screening tools, the VES-13 is a self-administered test, which means a health care professional is not required to administer the tool. The VES-13 can be mailed to patients prior to an appointment and takes 4 to 5 minutes to complete (16,26). A small percentage of patients may not be able to complete the survey independently due to a language barrier, cognitive impairment, or low level of education (27,28).
The SIOG systematic review of 10 studies that compared VES-13 to CGA found these studies to have an average sensitivity of 68.3% (39%–87%) and specificity of 71.6% (61%–100%) (16,26,29–35). This review determined that the VES-13 is less sensitive but more specific for an abnormal CGA compared to other screening tools (9).
Investigators have also assessed the predictive ability of the VES-13 in older patients with cancer:
■ Treatment-related toxicity: A pooled analysis of four observational and prospective studies involving 648 patients over age 65 showed that patients with an abnormal VES-13 were at double the risk of chemotherapy toxicity (36).
■ Overall survival: Two studies have shown mixed results regarding the prognostic value of the VES-13 (16,37).
The VES-13 tool is specific for an abnormal CGA, with the added advantage of being self-administered, which allows this tool to be easily incorporated into any clinical practice. These benefits must be balanced by a lower sensitivity, meaning that a number of patients with a normal screening VES-13 would have an abnormal CGA.
TABLE 14.2 VES-13 Screening Tool
123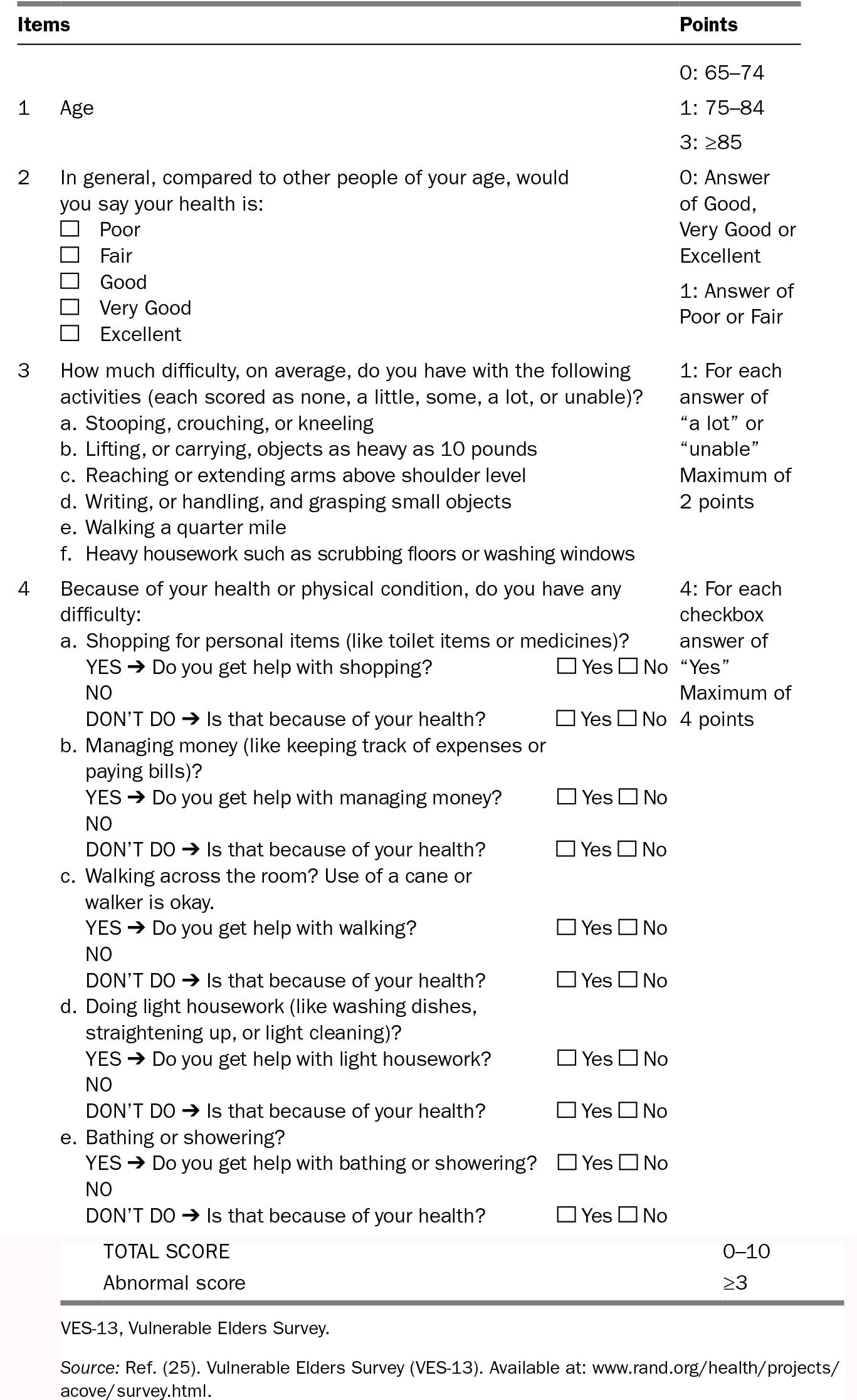
124TABLE 14.3 Comparing G8 and VES-13
G8 | VES-13 | |
Original target population | Oncology patients over age 70 scheduled for first-line chemotherapy | Community general geriatric patients 65 and over |
Who administers the test | Health care professional | Self-administered ± health care professional |
Location of administration | Clinic | Home Waiting room Clinic |
Cost of the test | Free | Free |
Domains covered | Functional status Self-rated health Comorbidities Nutrition Cognitive function | Functional status Self-rated health |
Time to perform | ~5 min | 4–5 min |
Number of studies comparing to CGA | 8 | 11 |
Average sensitivity for an abnormal CGA (range) | 82.8 (65–92) | 61.1 (39–87) |
Average specificity for an abnormal CGA (range) | 68.3 (3–75) | 71.6 (62–100) |
Abnormal score predictive for: Chemotherapy-related toxicity Functional decline Falls | Mixed results Yes Yes | Yes Not studied Not studied |
Abnormal score prognostic for overall survival | Yes | Mixed results |
Limitations | May require special assessment regarding “neuropsychosocial problems” | Some patients may be unable to self-administer test |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree