(1)
State University of New York at Buffalo Kaleida Health, Buffalo, NY, USA
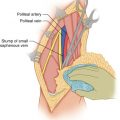
Retroperitoneal sarcomas present technical difficulties in their resection. The tumors are discovered when they are quite advanced locally, and their complete surgical resection is difficult because of their large size, inaccessible location, and infiltration of adjacent retroperitoneal structures. Often the patient or the physician will palpate a large, asymptomatic abdominal mass, or the diagnosis is triggered by mild abdominal pain or discomfort. In the pelvis, pressure by the tumor on the femoral nerve may cause pain in the distribution of this nerve in the anterior thigh and/or the anterior leg (via the saphenous branch of femoral nerve), or in the lateral thigh (lateral femoral cutaneous nerve), or medial thigh (obturator nerve), or groin (genitofemoral nerve). Pressure on the iliac vein may cause swelling of the ipsilateral extremity. Preoperative CT scans of the abdomen and pelvis or MRI tends to outline the extent of the tumor and its location quite effectively. A chest x-ray and preferably a CT scan of the chest are also performed, to rule out the presence of pulmonary metastases.
At present, the best available treatment for retroperitoneal sarcoma is complete resection, preferably with en bloc resection of adjacent tissues and organs if they are close to the tumor. A review published in 1991 of the results of treatment of several series of patients at major institutions in the United States found that the complete resection rate of retroperitoneal sarcomas was only 53 % [1]. Complete resection was the chief determinant of subsequent survival for the patient. A high rate of local recurrence was also identified, obviously because microscopic disease was left behind at the time of the presumed definitive resection. For local recurrence, it is important to operate promptly and resect the recurrent tumor as completely as possible. Survival of these patients varies according to the completeness of surgical resection and the grade of the tumor. Whether the tumor is resected completely depends on factors related both to the tumor itself and to the operative approach. Factors related to the tumor are the location of the tumor, the size of the tumor, the involvement of important structures near the tumor, the vascularity of the tumor, and whether the tumor is well circumscribed or tends to be diffuse and infiltrative of the adjacent structures. Factors related to the operative approach are the incision used, the positioning of the patient on the operating table, the strategy pursued in removing the tumor, and flexibility in the approach to resecting the tumor (Table 35.1).
Table 35.1
Position on the operating table and incisions for the resection of large retroperitoneal sarcomas
Location of sarcoma | Position | Incision |
|---|---|---|
Upper quadrant | Lateral | Thoracoabdominal and midline |
Flank | Lateral | Flank and midline |
Midline upper | Supine | Midline |
Pelvis | Supine | L or T |
Pelvis, iliac fossa, groin, pubic bone, adductors | Supine | Abdominoinguinal |
For large upper quadrant sarcomas, a midline incision from the xiphoid to below the umbilicus is often useful, which is combined with a thoracoabdominal incision from the costal margin to the midline incision just above the umbilicus. The exact placement of this incision of course depends on the location of the tumor. Therefore, when the midline incision is made, palpation of the area of the tumor is carefully carried out upon entering the abdomen, so as to select the appropriate placement of the thoracoabdominal incision. Whether the incision will be extended into the chest wall depends on the precise location of the tumor mass and whether it involves the diaphragm. For upper quadrant tumors, or at least for larger ones filling up the entire space, it is preferable that the patient is placed in a lateral position so that gravity works in concert with the surgeon and not in opposition (Figs. 35.1 and 35.2). Important anatomical structures posteriorly are of course the abdominal aorta and the inferior vena cava. It has been advocated by some surgeons that in the resection of retroperitoneal sarcomas, one should use a midline incision with the patient supine on the operating table, and one should identify early on whether the tumor mass can be separated from the aorta or the inferior vena cava, thus determining the resectability of the tumor [1]. It is true that these are two important structures that need to be separated off the tumor, but in reality, placing the patient in a supine position and using a midline incision as an early attempt to separate the tumor from the aorta or inferior vena cava is bound to cause a retreat by the surgeon due to the perception that it is too dangerous to proceed with resection. It is obviously very difficult to create a plane between the tumor mass and the aorta if a large retroperitoneal sarcoma is abutting the aorta for several centimeters and the tumor is packed in that area and is not amenable to retraction in a lateral direction because there is no available space laterally. Should some bleeding occur from a lateral branch of the aorta, such as a lumbar artery, it may be very difficult to see the area of the bleeding and control it. Therefore, this approach would tend to cause a high unresectability rate for such tumors. On the other hand, with the patient in a lateral position, the posterolateral aspects of the tumor can be mobilized off the lateral abdominal wall (transverse abdominis) and the posterior abdominal wall musculature, such as the quadratus lumborum and psoas, removing as needed the inner muscle layers attached to the tumor, en bloc with the tumor and adjacent structures. When the diaphragm is involved, it is incised around the tumor mass, entering the pleural space, which exposes the superior surface of the diaphragm usually not infiltrated through by the tumor. With this exposure it is easy to cut the diaphragm around the tumor at a distance of 1–2 cm. No attempt is made to dissect within the thickness of the diaphragm to separate the tumor. Such an approach results in deficient, or no margin and a thinned out diaphragm unsuitable for its function. Removal of the involved diaphragm with the tumor mass mobilizes significantly the latter. The whole mass is displaced anteriorly. Anteriorly and medial to the tumor, other abdominal structures such as the tail of the pancreas and the spleen or colon may be separated or included as need be in the planned procedure of resection, further facilitating the mobilization of the tumor. One then would be able to retract the tumor mass sufficiently to create a plane a few millimeters wide between the tumor and the aorta and separate the tumor mass from the aorta, starting from the inferior pole of the tumor. Organs that may have to be resected in the left upper quadrant en bloc with the tumor are the spleen, the distal pancreas, the left kidney and adrenal, the splenic flexure of the colon and part of the left transverse or descending colon, part of the stomach, and the left hemidiaphragm. On the right side, structures that may be included with the tumor mass would be the right kidney and adrenal, the hepatic flexure of the colon, the right hemidiaphragm, and part of the right lobe of the liver or the entire lobe (Figs. 35.3, 35.4, and 35.5).


Fig. 35.1
Large retroperitoneal sarcoma in the left upper quadrant, resected through a combination of midline and left thoracoabdominal incision with the patient in a lateral position