Step 1
Surgical Anatomy
- ♦
Thyroid reoperations are among the most technically demanding and morbid procedures in endocrine surgery. The additive effect of postoperative adhesions, the altered relationship between the recurrent laryngeal nerve, parathyroid glands, and the thyroid remnant or recurrence, and the difficulty in differentiating normal parathyroid tissue from a recurrent thyroid nodule or lymph node all contribute to the challenges of thyroid reoperations.
- ♦
In this chapter we discuss the indications for thyroid reoperations, the preoperative evaluation for these patients, and some intraoperative strategies to optimize the safe conduct of the operation.
Indications ( Box 4-1 )
Benign Disease
- ♦
Although recurrences of multinodular goiter (MNG) after total thyroidectomy are essentially nonexistent, the recurrence rate after less than total thyroidectomy may be as high as 42%. For Graves’ disease, recurrence rates of 16% are described with less than total thyroidectomy.
- ♦
For both MNG and Graves’ disease, the indications for reoperation are similar to the indications used for the initial operation, with the caveat that the risks are magnified up to fivefold: dyspnea or dysphagia due to tracheal or esophageal compression, hoarseness due to recurrent laryngeal nerve stretch or traction, and extensive substernal extent of the goiter. A relative indication for reoperation is the cosmetic effect of a recurrent cervical goiter. For patients with Graves’ disease, recurrent hyperthyroid symptoms may be an indication for reoperation, particularly if radioiodine ablation is contraindicated in the patient.
Benign Disease
Multinodular Goiter
- ♦
Tracheal compression
- ♦
Esophageal compression
- ♦
Superior vena cava compression
- ♦
Hoarseness from recurrent laryngeal nerve stretching
- ♦
Substernal extension
- ♦
Cosmetic
Graves’ Disease
- ♦
Recurrent hyperthyroid symptoms
Thyroid Cancer
Local Recurrence
Lymph Node Recurrence
- ♦
Central or lateral neck
Thyroid Cancer
- ♦
Recurrent thyroid cancer, whether papillary, follicular, or medullary, is an indication for reoperative neck surgery. Death from well-differentiated thyroid cancers, although rare, is most commonly due to airway compression from local recurrences that can no longer be resected. Therefore, early detection and resection of differentiated thyroid cancer recurrences are of paramount importance.
- ♦
In medullary thyroid cancer, recurrent disease is evident in approximately half of patients who undergo total thyroidectomy, bilateral central node dissection, and lateral functional lymph node dissections. Reoperation is indicated in all patients whose disease can be controlled surgically.
- ♦
Another category of patients who should be considered for reoperation are those who have had prior cervical operations for other reasons: patients who have had parathyroid surgery, carotid endarterectomy, cervical disk fusion, or surgery for a Zenker’s diverticulum, for example, should all be considered to be high risk, and all of the precautions described here should be taken.
Step 2
Preoperative Considerations
- ♦
All patients who undergo thyroidectomy for thyroid cancer should have ultrasound evaluation of the neck, directed specifically at lymph nodes. Ultrasound alters the operative approach in as many as 39% of patients; future reoperation for the eventual clinical detection of lymph nodes that actually were present at the time of initial operation may be avoided.
- ♦
Postoperatively, all patients should be enrolled in a surveillance program to facilitate early detection of recurrent disease. The combination of serum thyroglobulin measurement and serial cervical ultrasound examinations has been demonstrated to be effective in early detection of recurrent thyroid cancer. After thyroidectomy for benign disease, patients should undergo routine physical examinations, with ultrasonography for evaluation of symptoms.
- ♦
Previous operative reports should be obtained and reviewed for any patient who will undergo cervical reoperation. Knowledge of the extent of mobilization and resection of the thyroid gland, the number of positively identified (and preserved) parathyroid glands, and the previous identification of the recurrent laryngeal nerve are critically important. This information should be correlated with the final pathology report.
- ♦
In addition to the standard preoperative evaluation for the surgical patient, any patient who is scheduled to undergo thyroid reoperation should have an outpatient preoperative laryngoscopy.
- ▴
Up to 32% of patients with unilateral recurrent laryngeal nerve injury are clinically asymptomatic because of the relatively medial resting position of a paralyzed vocal cord. In these patients, endotracheal intubation alone may be enough to induce hoarseness and increase the risk for aspiration.
- ▴
Moreover, the functional status of both vocal cords is a critical factor in preoperative and intraoperative decision making: whereas knowledge of a paralyzed vocal cord on the same side as the patient’s pathology would allow the surgeon to be more aggressive, a contralateral paralysis should prompt the surgeon to exercise extreme caution intraoperatively, because every effort should be made to avoid bilateral vocal cord paralysis and the need for postoperative tracheostomy.
- ▴
Step 3
Operative Steps
Patient Positioning
- ♦
Patient positioning for reoperative thyroid surgery is the same as for the initial operation. Both the supine position with the head in extension and the beach chair position offer excellent exposure to the central and lateral compartments of the neck, as well as excellent access to most substernal goiters.
- ♦
If necessary, a partial or complete sternotomy can be performed. In our experience, turning the head to the contralateral side of the pathology does not substantially improve visualization and alters the anatomic relationships that are essential for identification of the recurrent laryngeal nerves and parathyroid glands.
Recurrent Laryngeal Nerve Monitoring
- ♦
Although no study has definitively demonstrated that intraoperative monitoring of the recurrent laryngeal nerve reduces the injury rate, there is ample anecdotal evidence that this may be a useful adjunct for the identification of the recurrent laryngeal nerve. Because most monitoring systems require a specialized endotracheal tube, the decision to use this technology is best made preoperatively. Alternatively, a standard nerve stimulator can be used to directly stimulate the suspected recurrent laryngeal nerve while the surgeon’s finger is in the retropharyngeal space feeling for the evoked contraction of the cricopharyngeus muscle.
- ♦
In situations in which the recurrent laryngeal nerve cannot be identified at the conclusion of the case, the surgeon may stimulate the vagus directly.
- ▴
The carotid sheath is opened using electrocautery, and the vagus is identified deep in the sheath, between the carotid artery and the jugular vein.
- ▴
If stimulation of the vagus fails to elicit contraction of the cricopharyngeus muscle, either the stimulator probe is malfunctioning, the endotracheal tube is malpositioned, or the recurrent laryngeal nerve has been injured.
- ▴
Preoperative Antibiotics
- ♦
Although tissues that have been previously operated on are relatively hypoxic during reoperation, no specific recommendations for antibiotic prophylaxis exist, and there is no evidence to suggest that postoperative surgical site infections are more common after reoperations in the neck. In our practice, we do not routinely administer prophylactic antibiotics for cervical operations, and we do not alter this policy based on the number of previous operations the patient has undergone.
Lymph Node Recurrences
- ♦
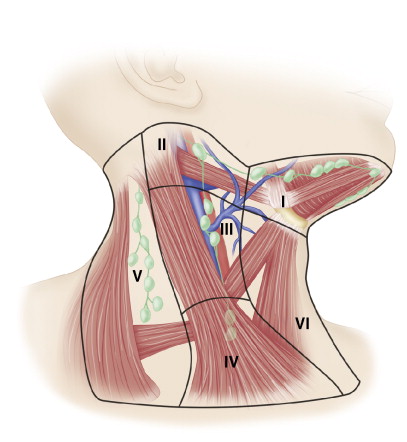
Nodal spread of papillary thyroid cancer occurs in a predictable, stepwise progression.
- ▴
The ipsilateral central compartment (level VI) is involved in almost three fourths of cases and is the only site of metastases in one fourth.
- ▴
The ipsilateral lateral compartment (levels II to V) is involved in 37% to 54% of patients; the contralateral central compartment is involved in only 10% to 20% of cases.
- ▴
- ♦
Clear evidence exists that in the setting of lymph node metastasis, a compartment-directed lymph node dissection or a selective lymph node dissection is preferable to “ berry picking, ” which is defined as resection of only palpable lymph nodes. This practice is associated with a high early recurrence rate.
Central Neck
- ♦
An increasing number of surgeons are proponents of routine prophylactic central neck (level VI) lymphadenectomy for patients with papillary thyroid cancer ( Fig. 4-1 ).
- ▴
The arguments in favor of this aggressive surgical approach include the high (up to 90%) incidence of lymph node metastases and the fact that 10% to 15% of patients treated with total thyroidectomy will ultimately develop central neck recurrences.
- ▴
Opponents of this approach cite the higher incidence of hypoparathyroidism after central neck lymph node dissection, the questionable impact of lymph node recurrences on survival, and the fact that most of the lymph node metastases are microscopic and could be effectively treated by radioiodine.
- ▴