Step 1
Surgical Anatomy
- ♦
One of the most common criticisms of the laparoscopic retroperitoneal approach is a seeming lack of anatomic landmarks. This is in contrast to the anatomically familiar view and orientation for the laparoscopic transabdominal approach. However, once one becomes accustomed to the layout and landmarks of the retroperitoneal space, it becomes clear that the anatomy of this space is well defined and consistent.
- ♦
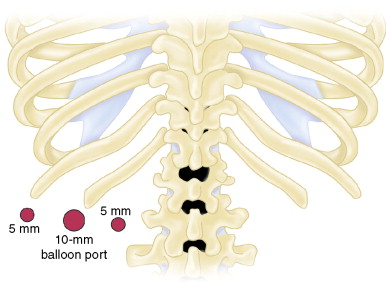
The retroperitoneal space is bounded by the following structures ( Fig. 12-1 ):
- ▴
Peritoneum laterally
- ▴
Paraspinous muscle medially
- ▴
Kidney/adrenal/peritoneum anteriorly (i.e., closer to the operating table)
- ▴
Rib cage posteriorly (i.e., away from the operating table).
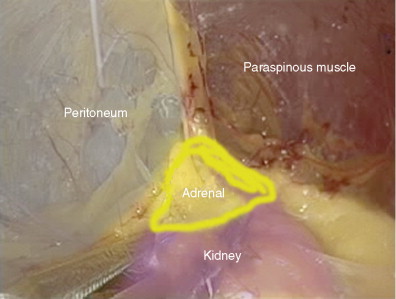
Figure 12-1
- ▴
- ♦
The superior pole of the kidney serves as the major landmark and focus point for the dissection.
Step 2
Preoperative Considerations
- ♦
The indications and contraindications for laparoscopic retroperitoneal adrenalectomy are similar to those for laparoscopic transabdominal adrenalectomy.
- ▴
This retroperitoneal technique is particularly good for patients who have had previous abdominal surgery because it avoids the peritoneal space and potential adhesions entirely. The main contraindications for this technique include body mass index greater than 40 (a large pannus can make it difficult to create a large enough retroperitoneal working space), tumors larger than 6 cm, and large adrenocortical cancers.
- ▴
- ♦
A urinary catheter should be placed for the duration of the operation. Due to the increased pressure from insufflation around the kidney, urine output during the operation may be lower than normal.
- ♦
The insufflation pressure can range from 15 to 30 mm Hg, depending on how much pressure is required to expand the intraperitoneal space. The average insufflation pressure is approximately 20 mm Hg. Of note, if one encounters bleeding during the operation, the pressure may be increased to 30 mm Hg to achieve tamponade. The surgeon and anesthesiologists should be in close communication to make sure that the patient’s CO 2 levels do not rise unacceptably.
- ♦
Specific preoperative considerations depend on the indication for resection.
Pheochromocytoma
- ♦
Preoperative blunting of the body’s response to catecholamine excess is essential. Most surgeons recommend α-blockade for 10 to 14 days before the operation in conjunction with adequate rehydration and sometimes with increased sodium intake. Due to catecholamine-mediated vasoconstriction, these patients are in essence volume-depleted and require increased oral intake to replete the intravascular space as this α-mediated vasoconstriction is relaxed.
- ♦
If the patient is still tachycardic after adequate hydration and α-blockade, a β-blocker may be added a few days before the operation. It is important to not institute β-blockade before effective α-blockade because unopposed α-mediated vasoconstriction may precipitate a hypertensive crisis.
Cushing’s Syndrome
- ♦
Patients should receive prophylactic antibiotics covering skin flora because patients have a higher incidence of wound infections due to the cortisol excess.
- ♦
Patients should receive a stress dose of steroids before induction of anesthesia as well as just before ligating the adrenal vein.
- ♦
It is important to remember that these patients will often require a long steroid taper to avoid addisonian crisis while the other adrenal gland resumes function.
Step 3
Operative Steps
Anesthetic Induction
- ♦
Appropriate vascular access and hemodynamic monitoring depend on the pathology. For example, resection of a pheochromocytoma may require central venous access and an arterial line. In contrast, resection of a nonfunctioning adenoma may simply require noninvasive monitors and peripheral intravenous lines.
- ♦
The patient is intubated on the stretcher to facilitate the prone positioning. A prone positioning mask or brace should be placed around the patient’s face to allow for proper positioning of the endotracheal tube once the patient is facedown.
Positioning
- ♦
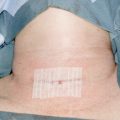
Patients are placed in the prone position with the hips and chest on bolsters to create a space in which the abdomen and pannus can lie. Creating this space is crucial to allowing the retroperitoneal space to fully expand ( Fig. 12-2 ).
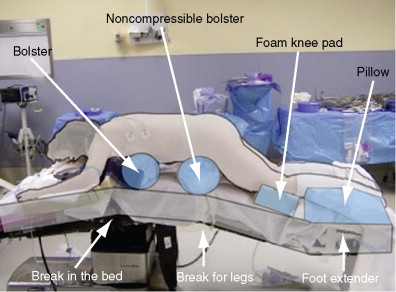
Figure 12-2
- ♦
The patient’s hips are placed on a noncompressible bolster at the joint for the leg portion of the bed. The leg portion of the bed is lowered roughly 30 to 45 degrees. An extension is placed at the foot of the bed and angled horizontal to the floor so that the shins and feet can rest on it. The bed is flexed slightly to allow the patient’s back to be completely parallel to the floor.
- ♦
Each area of contact with the bed is padded generously. The arms are placed in a neutral position flexed at the elbows. The patient’s side should be flush with the edge of the table so that the table will not interfere with the instruments.
- ♦
The patient’s back is prepared and draped from midchest to just above the buttocks.
Port Placement ( Figs. 12-3 and 12-4 )
- ♦
Three ports are used for this operation (one 10-mm port with donut-shaped balloon and two 5-mm ports).
- ♦
The following steps are taken when entering the retroperitoneal space:
- ▴
The first port is placed using a direct cutdown technique just inferior to the costal margin, halfway between the edge of the paraspinous muscle and lateral port (which is placed as far lateral as possible just inferior to the costal margin).
- ▴
A horizontal skin incision is made at this point large enough to admit a finger.
- ▴
The subcutaneous space is bluntly dissected with Metzenbaum scissors until the fascia is reached. The fascia is pierced bluntly to enter the retroperitoneal space. The opening is expanded by spreading with the Metzenbaum scissors as they are withdrawn. The retroperitoneal space is then bluntly dissected laterally and medially to allow for insertion of the remaining ports under direct palpation. Much like placing a chest tube, feeling a smooth surface directly over the ribs ensures dissection in the correct plane.
- ▴
- ♦
The steps for inserting the remaining ports are as follows:
- ▴
The lateral 5-mm port is placed as far lateral as possible just inferior to the costal margin.
- ▴
The medial port is placed just lateral to the paraspinous muscle. The skin incision should be made roughly in a horizontal line with the other ports and 4 to 5 cm inferior to the tip or inferior edge of rib 12. The port is then aimed on a bias into the retroperitoneal space just inferior to the tip or edge of rib 12 to achieve the proper orientation for this port.
- ▴