Step 1
Surgical Anatomy
- ♦
The pancreas is located in the lesser sac, with its anterior surface in the peritoneum and its posterior surface in the retroperitoneum. It is divided into four main portions: the head, neck, body, and tail.
- ▴
The head is bordered by the duodenum and contains the uncinate process.
- ▴
The neck is demarcated by the thinning out present where the portosplenic vessels run.
- ▴
The body runs from the border of the neck to the point where the splenic artery moves from running posterior to the pancreas to running anterior to the pancreas.
- ▴
The area from this point to the distal-most portion of the pancreas is known as the tail.
- ▴
- ♦
The head and neck of the pancreas receive their blood supply from the anterior and posterior superior pancreaticoduodenal arteries that come off the gastroduodenal artery superiorly and the superior mesenteric artery inferiorly. The body and tail of the pancreas receive their blood supply from the splenic artery ( Fig. 14-1 ).
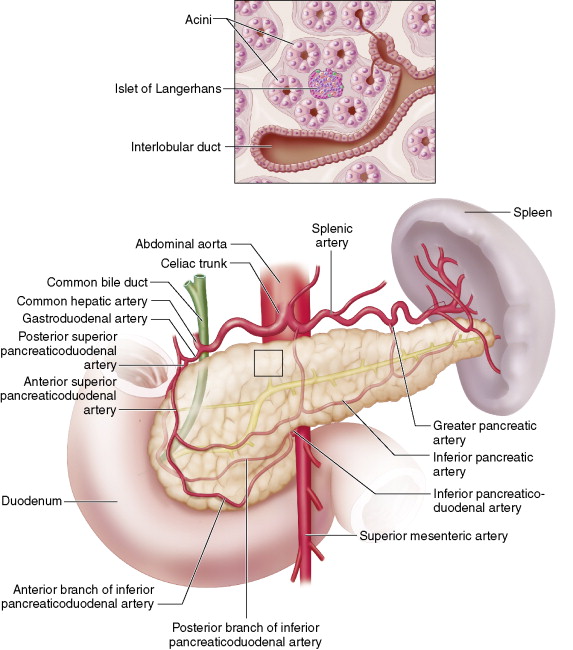
Figure 14-1
- ♦
The pancreas has an exocrine function, releasing zymogens such as enteropeptidase, necessary for activation of digestive enzymes such as lipase and amylase.
- ♦
The pancreas is unique in that it also has a complex endocrine profile. Functioning tumors can present with up to nine different clinical syndromes, insulinoma and gastrinoma being the most common; however, nonfunctioning tumors are the most frequent overall.
Step 2
Preoperative Considerations
- ♦
When a pancreatic endocrine neoplasia (PEN) is considered, we obtain chromogranin A levels, but hold off on other serum hormonal levels in the absence of a clinical syndrome.
- ♦
Although intraoperative ultrasound is the method of choice for localizing PENs, sometimes larger lesions can be seen on preoperative imaging. All patients get a chest x-ray to look for pulmonary primary and secondary lesions, and abdominal spiral computed tomography (CT) scans with a pancreatic protocol to see if the lesion can be localized and to rule out any hepatic metastases.
- ♦
In patients with a family or clinical history suggestive of an endocrine syndrome, such as multiple endocrine neoplasia type 1, neurofibromatosis 1, or Von Hippel-Lindau disease, we obtain genetic counseling and testing for the patient.
- ♦
Preoperatively, all patients undergo spiral CT scanning with intravenous contrast and thin slices through the pancreas. Neuroendocrine tumors of the pancreas are classically hypervascular; they have increased contrast on arterial phase images (black arrow; Fig. 14-2A ) and may leave a filling defect on venous phase images (white arrow; Fig. 14-2 ). Magnetic resonance imaging is at least equivalent to CT scan in its ability to localize PENs and can be used in patients with renal failure so that intravenous contrast can be avoided.

Figure 14-2

- ♦
If the diagnosis remains uncertain, endoscopic ultrasound is done with a 5 to 10 MHz transducer; this can be used to visualize the pancreas and duodenal wall. Because many gastrinomas present in the submucosa of the duodenum, this modality is indispensable for the proper preoperative localization of PENs. Lesions greater than or equal to 5 mm can be visualized with endoscopic ultrasound. PENs appear sonolucent on ultrasonography.
- ♦
If the diagnosis is suspected but the tumor is still not localized, we then proceed with intraoperative ultrasound of insulinoma. In Figure 14-3 , a pancreatic duct stent (small white arrow) can be seen running posterior and superior to the insulinoma (large blue arrow).
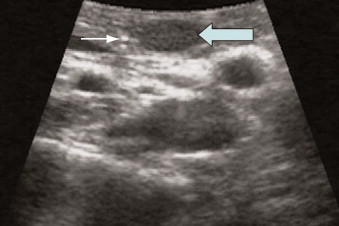
Figure 14-3
- ♦
Pancreatic endocrine neoplasias that express the somatostatin subtype-2 receptor (SSTR2) can be detected by standard octreotide scanning. This modality uses 111 indium-labeled octreotide to identify primary and secondary PENs. It is important to remember that although the sensitivity of octreotide scanning is approximately 90%, not all PENs express SSTR2, which is only one receptor out of the five known subtypes. This problem is especially pronounced in insulinomas because approximately half of these PENs do not express enough SSTR2 to be detected during octreotide scanning.
- ♦
In general, selective angiography and portal venous sampling have been relegated to cases that fail intraoperative localization with pancreatic sonography and palpation.
- ♦
Positron emission tomography scan is a promising new modality that appears to be more sensitive than the above-mentioned preoperative imaging techniques.
Step 3
Operative Steps
- ♦
A monopolar laparoscopic spatula (Storz, Tuttlingen, Germany), shown on the left in Figure 14-4 , can be particularly useful for laparoscopic enucleations (blue arrow; Fig. 14-4 ). Other surgical equipment that will be necessary includes a bipolar cautery forceps (Medtronic France S.A.S., Boulogne-Billancourt, France) for safe hemostasis and ultrasonic shears (SonoSurg, Olympus Optical, Tokyo), which are particularly useful for entering the lesser sac, performing the Kocher maneuver, and dissecting around the portal, superior mesenteric, and splenic veins and gastroduodenal, superior mesenteric, and splenic arteries.
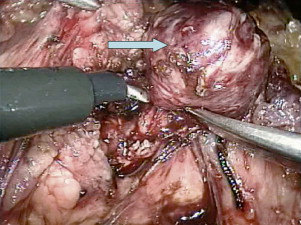
Figure 14-4 
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree