Step 1
Surgical Anatomy
- ♦
The anatomy associated with a gamma probe–guided approach to minimally invasive parathyroidectomy (MIP) is no different than for an MIP alone or traditional parathyroidectomy with bilateral exploration. Please refer to Chapters 6 and 8 for a complete review of the clinical anatomy involved with this procedure.
Step 2
Preoperative Considerations
- ♦
Preoperative preparations do not differ from those for a standard MIP. The use of the gamma probe should be thought of as an intraoperative adjunct, comparable to intraoperative ultrasound, methylene blue dye injection, or selective venous sampling. Please refer to Chapters 6 and 8 for additional preoperative considerations.
Indications
- ♦
The indications for a gamma probe–guided MIP include all causes of primary hyperparathyroidism (HPT): single adenoma, double adenoma, parathyroid hyperplasia, and parathyroid carcinoma.
- ▴
Secondary, tertiary, and familial HPT also are considered indications for a radioguided MIP.
- ▴
Imaging and Preoperative Parathyroid Localization
- ♦
For a minimally invasive approach, a preoperative localizing study is generally required for all patients to identify the hyperfunctioning parathyroid.
- ♦
Technetium (Tc) 99m sestamibi single-photon emission computed tomography scanning is the procedure of choice ( Fig. 10-1 ). Hyperfunctioning parathyroid glands have overactive cells with increased numbers of mitochondria that sequester the Tc 99m sestamibi and retain the radiotracer longer than the surrounding tissue, allowing visualization or detection of the gland. This phenomenon is the physiologic basis for both sestamibi imaging and gamma probe–guided surgery.
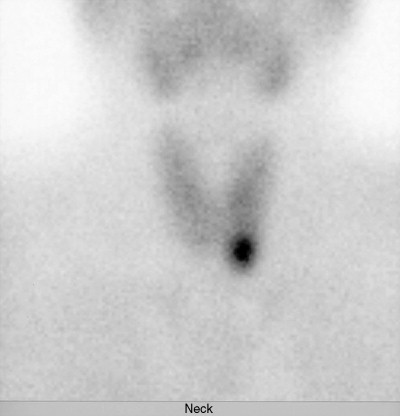
Figure 10-1
- ♦
Thallium-technetium subtraction scintigraphy was used more frequently before the introduction of sestamibi imaging and may aid localization in patients with otherwise negative studies. This imaging depends heavily on the size of the adenoma.
- ♦
Cervical ultrasonography is another method used to localize the enlarged parathyroid. It is less expensive and no radiation is involved, but it requires an experienced operator for good results.
- ♦
Internal jugular localization can also be used to isolate the side of the neck that harbors the hyperfunctioning parathyroid if sestamibi scanning is unsuccessful. This procedure is performed intraoperatively by obtaining venous blood samples from both internal jugular veins and sending them for rapid parathyroid hormone (PTH) assay ( Fig. 10-2 ). The PTH levels are lateralizing if values for one side are more than 5% greater than values for the opposite side. The sensitivity of bilateral internal jugular venous sampling is approximately 80%.

Figure 10-2
Anesthesia
- ♦
General endotracheal anesthesia is the standard anesthetic traditionally used during a bilateral four-gland exploration. However, the decreased operative times and minimal dissection associated with a gamma probe–guided MIP have allowed this procedure to be performed under local anesthesia with the supplementation of intravenous (IV) sedation when needed.
- ♦
Advantages of local anesthesia include decreased use of postoperative IV narcotics and antiemetics along with less reported postoperative nausea or vomiting. This approach is particularly advantageous in patients with contraindications to general anesthesia.
- ♦
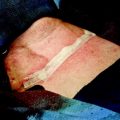
Most radioguided MIPs can be accomplished using superficial cervical block anesthesia on the ipsilateral side of the prelocalized hyperfunctioning parathyroid. Approximately 30 mL of 1% lidocaine or anesthetic of choice is infiltrated posterior and deep to the sternocleidomastoid muscle ( Fig. 10-3A ) and locally along the anterior border of the muscle. In addition, a local field block is attained with subcutaneous administration of the local anesthetic ( Fig. 10-3B ). The black dots in Figures 10-3A and B represent these sites of injection for the local anesthetic.
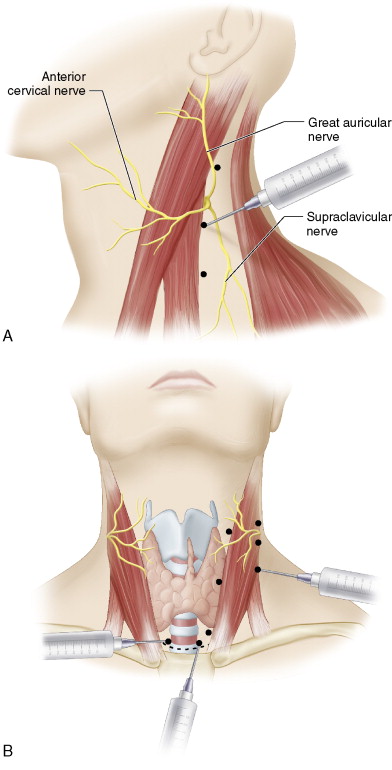
Figure 10-3
- ♦
Conversion to general endotracheal anesthesia should be performed without hesitation when necessary (e.g., when unexpected intraoperative findings are encountered or the patient experiences discomfort).
Surgical Equipment
- ♦
For this procedure, we use an 11-mm collimated gamma probe (Neoprobe 2000, Ethicon Endo-Surgery, Cincinnati, Ohio).
Step 3
Operative Steps
Injection of Radiotracer
- ♦
For a gamma probe–guided parathyroidectomy, patients receive a 10-mCi IV injection of Tc 99m sestamibi approximately 1 hour before surgery. This injection is only for intraoperative gamma detection, because images are not obtained on the day of surgery.
- ♦
Many patients with primary HPT have had a previous 20-mCi dose of Tc 99m sestamibi for a scan, to verify that they qualify for the minimally invasive approach. Surgery is rarely performed within 3 days of the initial injection so that the radiotracer has time to wash out.
- ♦
Preoperative sestamibi imaging is not practical for all patients, including those who do not live near a scanning facility or those who present emergently with hypercalcemic crisis. In these isolated instances, we have successfully administered a single 20-mCi dose of radiotracer, obtained images at 15 and 90 minutes, and proceeded with surgery approximately 2 to 2.5 hours after injection.
- ♦
The timing of radiotracer injection is essential for a successful gamma probe–guided MIP. Localization of the parathyroid ideally occurs between 1 and 3 hours postinjection. Therefore, patients are usually scheduled for sestamibi injection 1 hour before surgery.
Background Counts
- ♦
The first step intraoperatively during a gamma probe–guided parathyroidectomy is setting the background counts before skin incision. The thyroid isthmus is palpated manually through the skin. The gamma probe is then placed at a 90-degree angle to the skin over the thyroid isthmus and the background counts are recorded ( Fig. 10-4 ).
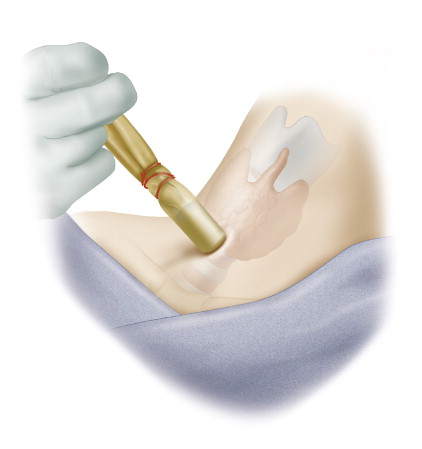
Figure 10-4
- ♦
Setting the background counts is important because localization of overactive parathyroid tissue, which is often posterior to the thyroid lobes, depends on the probe’s ability to detect radiotracer counts above the background. Sestamibi washes out of hyperfunctioning parathyroid tissue slower than out of thyroid tissue, allowing the gamma probe to reveal the parathyroid’s location.
Incision and Dissection
- ♦
This step is the same for all minimally invasive approaches regardless of adjunctive techniques. A transverse cervical incision approximately 2 cm in length is made over the site of the localized parathyroid tissue in accordance with the sestamibi scan. When possible, the incision is made along a pre-existing skin fold to conceal later scarring.
- ♦
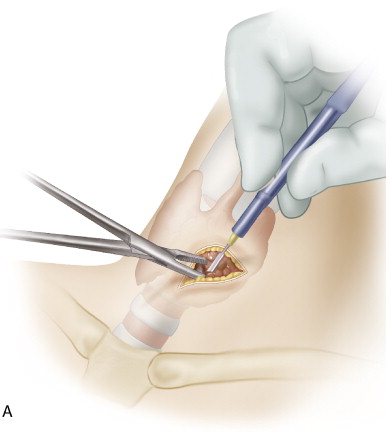
Bovie cautery is used to divide the platysma ( Fig. 10-5A ).