Step 1
Indications for Surgical Therapy
- ♦
Thyroidectomy is the most common endocrine operation performed, and nodular thyroid disease is the most common endocrine disorder.
- ♦
Nodular thyroid disease affects 500 to 600 million people worldwide, with iodine deficiency as the most important etiologic factor.
- ▴
In the United States, which is replete with iodine, palpable thyroid nodules occur in 4% to 7% of the population, underscoring the importance of other etiologic factors that have yet to be definitively identified.
- ▴
The annual incidence of palpable thyroid nodules is approximately 0.1%. Nodules may develop at a higher rate, up to 2% per year, in patients exposed to head or neck radiation.
- ▴
Autopsy series have documented unsuspected thyroid nodules in 50% of patients; recent series, using ultrasonography, have demonstrated a prevalence of nodular thyroid disease as high as 60% to 70%.
- ▴
- ♦
Only 5% of thyroid nodules are malignant, and fine-needle aspiration biopsy (FNAB) is important for distinguishing nodules that can be followed clinically from those that need operative management.
- ♦
Surgical therapy is indicated for a thyroid nodule when FNAB shows a malignancy or is suspicious for papillary carcinoma, consistent with follicular or Hürthle cell neoplasm, or persistently nondiagnostic.
- ♦
Operative therapy for benign thyroid nodules is recommended for:
- ▴
progressive increase in nodule size
- ▴
substernal extension
- ▴
compressive symptoms
- ▴
radiographic documentation of tracheal, esophageal, or major vessel impingement
- ▴
the development of thyrotoxicosis
- ▴
cosmetic issues and patient preference.
- ▴
- ♦
Total thyroidectomy is indicated for patients with a thyroid nodule who have a prior history of low-dose head or neck irradiation because of a known 40% incidence of carcinoma.
Step 2
Preoperative Considerations
- ♦
Patients with nodular thyroid disease should have a complete history and physical examination.
- ▴
They should be questioned about symptoms of hyperthyroidism or hypothyroidism, neck pain, dysphagia, dyspnea, hoarseness, coughing or choking spells, a prior history of head or neck irradiation, and a family history of thyroid cancer and other endocrinopathies.
- ▴
The physical examination should include an assessment of the size and character of the nodule, the position of the trachea, and whether or not there are nodules involving both lobes of the thyroid gland or cervical lymph node metastases.
- ▴
- ♦
Flexible fiberoptic laryngoscopy is recommended for assessment of the vocal cords in all patients with advanced thyroid cancer, a prior neck operation, or hoarseness or other voice changes.
- ♦
Symptoms of hyperthyroidism can be seen in patients with a solitary functioning adenoma or a toxic multinodular goiter. Neck pain and symptoms of hypothyroidism are manifestations of thyroiditis.
- ♦
A prior history of radiation exposure; a history of thyroid cancer in a first-degree relative or other familial syndromes associated with thyroid cancer ( Box 1-1 ); a hard, fixed nodule; vocal cord paralysis; and associated cervical lymphadenopathy are features that are suggestive of thyroid cancer.
BOX 1-1
Familial Syndromes Associated with Thyroid Cancer
- ♦
Multiple endocrine neoplasia, type 1A and 2B
- ♦
Gardner’s syndrome
- ♦
Familial adenomatous polyposis
- ♦
Carney complex
- ♦
Cowden’s syndrome
- ♦
Familial nonmedullary thyroid cancer
- ♦
- ♦
All patients with nodular thyroid disease should have a screening serum thyrotropin (TSH) level measured to assess the functional status of the thyroid gland.
- ♦
Free T 4 and free T 3 levels should be obtained in patients with an abnormal serum TSH level. In patients with thyrotoxicosis, it is important that free T 4 and free T 3 levels be normalized before the operation to prevent thyroid storm, a potentially lethal complication.
- ♦
Hypothyroidism may be associated with delayed anesthetic and drug metabolism and should be treated before thyroidectomy.
- ♦
Before operation, the American Thyroid Association, the American Association of Clinical Endocrinologists, and the National Comprehensive Cancer Network recommend an ultrasound examination of the thyroid gland to determine the location and extent of nodular thyroid disease.
- ♦
Specific sonographic criteria may also be helpful in differentiating benign from malignant thyroid nodules ( Box 1-2 ), although the sensitivity and negative predictive value of ultrasound are considerably higher than the specificity and positive predictive value. No single criterion can distinguish benign from malignant thyroid nodules with 100% reliability.
BOX 1-2
Sonographic Features of a Thyroid Nodule that Are Concerns for Malignancy
- ♦
Marked hypoechogenicity (less echogenic than the strap muscles)
- ♦
Irregular shape with an anteroposterior dimension that is greater than the transverse dimension
- ♦
Spiculated, microlobulated, or ill-defined margins
- ♦
Microcalcifications
- ♦
Increased intranodular blood flow
- ♦
Incomplete peripheral halo
- ♦
- ♦
An ultrasound examination of the central and lateral neck is important for patients with a nodule that is consistent with or suspicious for papillary thyroid cancer to identify associated lymph node metastases. Physical examination can miss macroscopic cervical lymph node metastases that are visible on ultrasound in up to 40% of patients.
- ▴
The preoperative identification of cervical lymph node metastases may alter the surgical approach and minimize persistent or recurrent disease.
- ▴
- ♦
There are well-described sonographic features of a lymph node that raise suspicion for malignancy ( Box 1-3 ).
BOX 1-3
Sonographic Criteria that Increase Suspicion for a Metastatic Lymph Node
- ♦
Diameter >1 cm
- ♦
Irregular rounded shape, characterized by a ratio of the long axis to the short axis of a lymph node <1.5
- ♦
Loss of the hilum (absent hilar echoes)
- ♦
Heterogeneous echogenicity
- ♦
Cystic necrosis
- ♦
Irregular margins
- ♦
Microcalcifications
- ♦
- ♦
Ultrasound is also of value for guiding FNAB in patients with a nondiagnostic conventional FNAB or a difficult to palpate or nonpalpable nodule and to confirm suspected lymph node metastases.
- ♦
Patients should be instructed to discontinue aspirin, nonsteroidal anti-inflammatory drugs, and clopidogrel (Plavix) 7 days before surgery. Patients should also be instructed to discontinue vitamin E and any herbal supplements that may affect coagulation 10 days before surgery. Warfarin (Coumadin) should be stopped 5 days before surgery.
- ♦
Neck hematoma, although uncommon, is a life-threatening complication of thyroidectomy. When blood accumulates in the neck, the venous drainage of the larynx may become impaired; patients develop glottic narrowing or closure, which manifests with stridor, acute respiratory compromise, and death. Consequently, we do not use subcutaneous heparin for prophylaxis against deep vein thrombosis because of the risk of wound hematoma.
- ♦
A sequential compression device is preferentially used for prophylaxis against deep vein thrombosis in all patients.
Surgical Therapy
- ♦
In patients with nodular thyroid disease and an FNAB that is malignant, total thyroidectomy is the usual treatment. The exception is a patient with a papillary thyroid cancer smaller than 1 cm that is confined to the thyroid gland without metastases, for whom a thyroid lobectomy and isthmusectomy is adequate therapy.
- ♦
Patients with medullary thyroid carcinoma are treated with total thyroidectomy and a central neck dissection with or without unilateral or bilateral modified neck dissection.
- ♦
Patients with differentiated thyroid cancer and documented prelaryngeal, pretracheal, paratracheal, or anterior mediastinal lymph node metastases should undergo a central neck dissection. Some authorities recommend routine central neck dissection in patients with papillary or Hürthle cell cancer.
- ♦
A modified neck dissection is performed for patients with differentiated thyroid cancer when macroscopic cervical lymph node metastases are present.
- ♦
Patients with a thyroid nodule and an FNAB that is suspicious for papillary thyroid cancer or persistently nondiagnostic are treated with thyroid lobectomy, isthmusectomy, and frozen section examination.
- ♦
Total thyroidectomy is performed when frozen section examination establishes a diagnosis of carcinoma.
- ♦
Patients with a thyroid nodule that is consistent with a follicular or Hürthle cell neoplasm are treated with a thyroid lobectomy and isthmusectomy without frozen section examination. A completion thyroidectomy is recommended for a final pathologic diagnosis of invasive follicular or Hürthle cell carcinoma.
- ♦
A thyroid lobectomy and isthmusectomy is appropriate for a “minimally invasive” follicular cancer, defined as an encapsulated follicular cancer with minor capsular invasion only.
- ♦
In patients with benign nodular thyroid disease who undergo operative therapy, surgical resection consists of thyroid lobectomy and isthmusectomy for patients with disease limited to one lobe. In all patients undergoing operative therapy, contralateral disease is excluded by preoperative palpation, ultrasound examination, and intraoperative palpation. Patients with bilateral benign nodular thyroid disease are treated with near-total or total thyroidectomy.
Clinical Anatomy
- ♦
The term thyroid is derived from the Greek word thyreos, which means shield. The shape of the normal thyroid gland resembles a shield ( Fig. 1-1 ).
- ▴
The thyroid consists of two lobes and an isthmus and weighs approximately 15 to 20 grams. Approximately 30% to 50% of patients also have a pyramidal lobe, which represents a persistence of the embryologic thyroglossal duct ( Fig. 1-2 ).In Figure 1-2 , P indicates the pyramidal lobe and N indicates the nodule.

Figure 1-2
- ▴
The pyramidal lobe extends superiorly from the isthmus or from one of the lateral lobes of the thyroid gland. If overlooked at surgery, the pyramidal lobe can be a source for persistent iodine 131 uptake in patients with cancer. It may also become enlarged in patients with sporadic or endemic goiter.
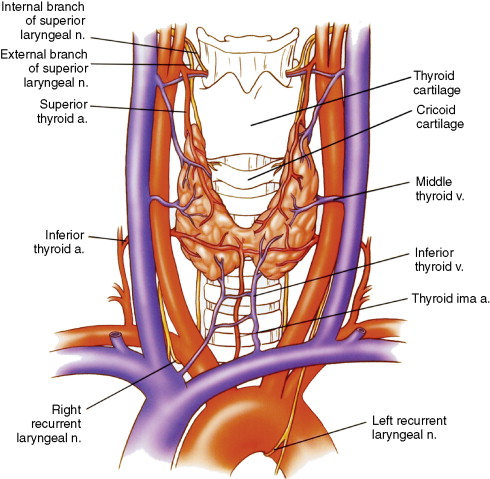
Figure 1-1
- ▴
- ▴
The thyroid gland is situated on the anterolateral aspect of the upper trachea and the larynx.
- ▴
The isthmus of the thyroid gland lies just inferior to the cricoid cartilage (see Fig. 1-1 ).
- ▴
The thyroid gland is fixed to the upper tracheal rings and the cricoid cartilage by a posterior suspensory ligament known as the ligament of Berry.
- ▴
- ♦
The blood supply to the thyroid gland is derived principally from the superior and inferior thyroid arteries (see Fig. 1-1 ).
- ▴
The superior thyroid artery is the first branch of the external carotid artery. It gives off a large branch to the pyramidal lobe and the isthmus of the thyroid gland.
- ▴
The inferior thyroid artery is a branch of the thyrocervical trunk from the subclavian artery.
- ▴
A thyroid ima artery may also be present. It comes directly from the innominate artery or the arch of the aorta.
- ▴
- ♦
In humans, there are typically four parathyroid glands. Five or more parathyroid glands may be present in 10% to 15% and only three parathyroid glands in 3% of individuals.
- ♦
Normal parathyroid glands are oval, bean-shaped, or spherical; yellow-tan in color; and surrounded by adipose tissue ( Fig. 1-3 ).
- ♦
Each parathyroid gland is approximately 5 mm in greatest dimension and weighs approximately 35 mg. It may be flattened in appearance when located within the capsule of the thyroid gland.
- ♦
The blood supply to the parathyroid glands comes from the inferior thyroid artery, superior thyroid artery, and small vessels from the capsule of the thyroid gland as documented by laser Doppler flowmetry.
- ♦
The superior parathyroid gland is normally present approximately 1 cm superior to the junction of the recurrent laryngeal nerve and the inferior thyroid artery at the level of the cricoid cartilage, where the recurrent laryngeal nerve enters posterior to the inferior pharyngeal constrictor muscle ( Fig. 1-4 ). The superior parathyroid gland lies posterior and superior to the recurrent laryngeal nerve.
- ♦
The inferior parathyroid gland is located at the posterior-lateral aspect of the inferior pole of the thyroid gland approximately 1 cm inferior to the junction of the recurrent laryngeal nerve and the inferior thyroid artery (see Fig. 1-4 ). The inferior parathyroid gland is most often anterior to the recurrent laryngeal nerve and less often subcapsular. The inferior parathyroid gland is more likely to be found in an ectopic location related to its more extensive embryologic migration.
- ♦
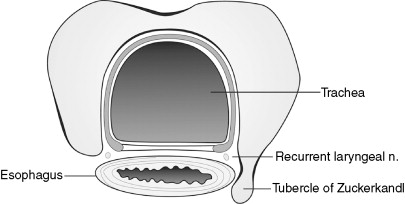
In 85% to 90% of patients, a portion of the thyroid parenchyma protrudes from the posterior lateral margin of one or both lobes of the thyroid gland; this is known as the posterior horn or the tubercle of Zuckerkandl ( Fig. 1-5 ). It is an important anatomic landmark because of its relationship to the recurrent laryngeal nerve and the parathyroid glands. It is usually only 8 to 10 mm in size.
- ▴
The recurrent laryngeal nerve typically passes in the tracheoesophageal groove between the main body of the lateral lobe of the thyroid gland and the inferior portion of the tubercle of Zuckerkandl before it turns posteriorly and passes into the larynx. In most patients, the superior parathyroid gland is adherent to or within 5 mm of the cranial portion of the tubercle of Zuckerkandl behind the recurrent laryngeal nerve and the inferior thyroid artery.
- ▴
The inferior parathyroid gland is located adjacent to the caudal portion of the tubercle of Zuckerkandl in front of the recurrent laryngeal nerve and the inferior thyroid artery. Recognition of this anatomic landmark is important in the preservation of the recurrent laryngeal nerve and the parathyroid glands during thyroid surgery.
- ▴