Abstract
The importance of regional lymph nodes in breast cancer and their appropriate treatment has undergone dramatic changes in a relatively short period. Although oncologists once considered them the gold standard for patient prognosis and prediction of who may benefit from systemic therapy, they have now turned to tumor markers, breast cancer intrinsic subtypes, and the “score” from several available tumor gene sets, such as such as the Oncotype Score (Genomic Health), the Mammoprint, and others. As well, the century-old Halsted concept of the regional lymph nodes as the “next step” toward spread of cancer from the breast to the nodes and ultimately to distant sites has been replaced with other models, resulting in a marked change in the nodal surgery recommended for a woman with a new breast cancer diagnosis. These concept changes have had a major impact on the role of radiotherapy in the management of breast cancer, in addition to changes in surgical approach. As is clear from recent studies, these new paradigms are applicable to both women who choose breast conservation surgery and those who choose mastectomy. This chapter focuses on recent studies in patients with early-stage breast cancer and the interpretation of the results for radiation treatment planning after breast conservation surgery.
Keywords
breast conservation surgery, whole breast radiation, regional lymph node treatment.
The importance of regional lymph nodes in breast cancer and their appropriate treatment has undergone dramatic changes in a relatively short period. Although oncologists once considered them the gold standard for prognosis for a patient and prediction of who may benefit from systemic therapy, they have now turned to tumor markers, breast cancer intrinsic subtypes, and the “score” from several available tumor gene sets, such as such as the Oncotype Score (Genomic Health), the Mammoprint, and others. As well, the century-old Halsted concept of the regional lymph nodes as the “next step” toward spread of the cancer from the breast to the nodes and ultimately to distant sites has been replaced with other models, resulting in a marked change in the nodal surgery recommended for a woman with a new breast cancer diagnosis.
These concept changes have had a major influence on the role of radiotherapy (RT) in the management of breast cancer, in addition to the changes in surgical approach. As is clear from recent studies, these new paradigms are applicable to both women who choose breast conservation surgery and those who choose mastectomy. This chapter focuses on recent studies in patients with early-stage breast cancer and the interpretation of the results for radiation treatment planning after breast conservation surgery.
Studies conducted in the 1980s demonstrated the benefit of RT to the chest wall and lymph nodes in women with positive lymph nodes who had a mastectomy followed by systemic chemotherapy and were randomized to receive or not receive postmastectomy RT. These studies demonstrated both a marked reduction in local-regional recurrence and a small but statistically improved survival for those assigned to receive RT. Those studies were criticized, however, especially in the United States, for the quite high locoregional recurrence rate in the women who received only surgery as local treatment.
Two new trials, the National Cancer Institute of Canada Clinical Trials Group (NCIC-CTG) MA20 trial and the European Organisation for Research and Treatment of Cancer (EORTC) trial, were conceived to reevaluate the role of nodal RT in women with earlier-stage breast cancer (high-risk node-negative and 1–3 positive nodes), in both patients opting for breast-conservation surgery and those who had a mastectomy.
For women with locally advanced breast cancer (stage III; T3/T4 N1 and T1–4 N2–3), it is generally agreed that the regional lymph nodes should be irradiated, regardless of the type of surgery the patients undergo. This is based primarily on the benefit demonstrated in the randomized postmastectomy radiotherapy (PMRT) trials, which included comprehensive nodal irradiation. The primary debate in the patients with stage III disease is whether the internal mammary node (IMN) chain requires coverage. The debate over the IMN chain is centered around the fact that isolated IMN recurrences in practice are quite rare and that IMN coverage is technically challenging, often increasing unwanted exposure to the heart, lung, and contralateral breast. This topic is discussed briefly in this chapter and also addressed in the chapter on PMRT.
Patient Selection
The debate over the need for nodal coverage in patients undergoing breast conservation with earlier-stage disease (mostly stage II) remains unanswered and is the focus of this chapter. We will consider two distinct groups of patients when considering those who have one to three axillary positive nodes: (1) one to three positive axillary sentinel nodes without completion dissection and (2) one to three positive axillary nodes with completion axillary dissection.
Positive Sentinel Node Without a Completion Axillary Dissection
An important group of patients is those who are clinically node negative and have a positive sentinel node biopsy with minimal disease burden in the axilla. The American College of Surgeons Oncology Group (ACOSOG) Z0011 study was conceived at a time when sentinel node dissection (SLND) was accepted as treatment for women with a negative sentinel node result, but those with a positive sentinel node were routinely undergoing a follow-up full axillary dissection (ALND). This prospective randomized trial was designed to compare completion axillary dissection to no further surgery in women undergoing breast conservation surgery with clinical T1 or T2 N0 M0 breast cancers found to have one or two positive sentinel nodes. Patients with three or more involved sentinel nodes were excluded from the study, as were those “with matted nodes or gross extranodal disease.” Approximately 40% of patients in this trial had micrometastases. The primary end point was survival, and the secondary end point was locoregional recurrence. Adjuvant systemic therapy was determined by the treating physician, and whole breast radiation was required, specifically without the use of a “third field” over the supraclavicular region. The originally planned accrual was 1900 patients, but the trial was closed in 2004 with 891 patients randomized, due to “lower than expected accrual and event rates.” Published results at a median follow-up time of 6.3 years showed no difference in survival, and no difference in locoregional recurrence between those women randomized to completion ALND and those who received only the sentinel node procedure. The study conclusion was “SLND without ALND can offer excellent regional control and may be reasonable management for selected patients with early-stage breast cancer treated with breast conserving therapy and adjuvant systemic therapy. “
But controversy over this study surfaced soon after the practice-changing surgical results were published, with implications for consideration of postlumpectomy radiation field design. One observation centered on the possibility that some radiation from the tangent breast fields was in fact treating the Level I–II region of the axilla. Was the use of “high tangents” more common in patients who were randomized in the study to the SLND arm only? To address these issues, completed case report forms from the Z 0011 study were reviewed in detail, and more detailed radiation field design information was requested, in a follow-up study by Jagsi and colleagues. Surprisingly, 15% of all women in the study were treated with a third field over the supraclavicular nodes, and from the smaller subset of patients for whom details of radiation field design were known, about half of those with breast tangent fields only had “high tangents,” defined as a superior field edge with 2 cm or less from the humeral head, including more of the axilla nodal region. No significant differences in radiation field design were noted between the two Z0011 treatment arms, but the findings of this study confirmed the hypothesis that some of the patients in the study had more nodal irradiation than the Z0011 study design had intended.
The International Breast Cancer Study Group (IBCSG) 23-01 trial had a design similar to the Z0011 trial but included only women with micrometastatic nodal disease and T1-T2 tumors. Additional axillary disease was identified in 13% of patients who had a completion dissection (vs. the 27% in Z0011). This study showed added morbidity with completion dissection and no benefit in terms of disease control, providing additional evidence that ALND is not needed for women with T1–T2 tumors and micrometastases.
For some patients, axillary treatment is still deemed useful. For patients with more than two positive sentinel nodes, axillary treatment is needed. In addition, treatment is recommended for those with high-risk features based on tumor size, type, grade, vascular invasion, and extracapsular extension of cancer in the sentinel nodes. The risk of additional axillary disease can be estimated with the use of a nomogram, which takes these risk factors into account. Several retrospective studies showed that in well-selected, low-risk women, axillary radiation can offer excellent axillary control. In 2001, EORTC initiated the 10981-22023 AMAROS trial, a randomized, multicenter, open-label, phase III noninferiority trial in patients with T1–T2 primary, unifocal, invasive breast cancer, with no palpable lymphadenopathy. Patients with tumors of up to 5 cm diameter were eligible. Radiation included the breast/chest wall, axilla, and supraclavicular (with only 10% of patients receiving IMN irradiation). Patients were randomly assigned before any surgery to axillary dissection or axillary radiation if they had a positive sentinel node biopsy. Of the 4806 patients randomized, 30% had positive sentinel nodes. A median of two sentinel nodes were removed and a median of one sentinel node was positive. Approximately 60% of patients had a macrometastasis, and 40% had a micrometastasis or isolated tumor cells. In the axillary dissection arm, 33% of patients had additional axillary metastases. Five-year axillary recurrence was 0.43% (95% confidence interval [CI] 0.00–0.92) after axillary lymph node dissection versus 1.19% (0.31–2.08) after axillary RT. Axillary dissection more than doubled the rate of clinical lymphedema at 5 years (11% vs. 23%). Thus this study concluded that if further axillary treatment is needed in clinically node-negative, sentinel-node–positive patients, axillary RT could be chosen instead of axillary lymph node dissection because it provides comparable axillary control and less morbidity. Although the National Surgical Adjuvant Breast and Bowel Project B04 trial was conducted many years ago, before sentinel node biopsies and routine use of systemic therapy, that study also showed that, for clinically node-negative women, axillary RT and axillary dissection offer similar rates of long-term axillary control.
Positive Sentinel Node and Completion Axillary Dissection With a Total of One to Three Positive Nodes
For patients who have a sentinel node and completion dissection with one to three positive nodes, there are a number of historical trials, several recent publications, and a few large retrospective series to help guide management. The original rationale for regional node irradiation (RNI) in women with one to three nodes came from the data from the randomized PMRT trials. These trials included all node-positive women, including those with one to three nodes. They found a locoregional control, disease-free survival, and overall survival benefit for the entire patient population. However, several large series from Eastern Cooperative Oncology Group trials conducted in the United States in which radiation was not used after mastectomy for women with one to three nodes showed that the locoregional failure rate was much lower than was reported in the randomized trials. This led to a number of subset analyses for patients with one to three nodes only, and these analyses continued to show a benefit for this subset of patients. However, the subset analysis had the same limitations as the original trials, which were criticized for outdated chemotherapy and inadequate axillary dissections with only an average of eight nodes removed at the time of dissection. The Early Breast Cancer Trialists’ Collaborative Group (EBCTG) meta-analysis specifically showed a benefit for women with even just a single positive node. This corroborates prior data showing that the relationship with the most impact may be between a reduction in locoregional recurrence and decreased breast cancer morality in women with a smaller burden of nodal metastases. Women with one to three positive lymph nodes likely have a lower competing risk of distant metastases than those with four or more positive lymph nodes; therefore, a reduction in locoregional recurrence due to locoregional therapies can result in a relatively greater impact on cancer-specific survival.
In an effort to better identify criteria for RNI in women with one to three nodes, a number of large retrospective trials from British Columbia and the MD Anderson Cancer Center identified risk factors that place patients at increased risk for locoregional recurrence. MD Anderson had several publications in the early 2000s on a cohort of 1031 women treated with mastectomy and Adriamycin-based chemotherapy without radiation. The goal of these studies was to identify risk factors after mastectomy to better select women for PMRT/RNI. These studies identified close or positive margins, microscopic invasion of the nipple, pectoral fascial involvement, presence of lymphovascular space invasion, and gross multicentric disease (>20% nodal involvement, tumors >4 cm, extranodal extension >2 mm) as risk factors for locoregional recurrence. A similar study was published by Truong and colleagues based on 821 treated in British Colombia with mastectomy and systemic therapy but no radiation. They found greater than 25% positive nodal ratio, estrogen receptor (ER) negativity, medial tumor location, and age less than 45 years to be risk factors. On the basis of these factors, clinicians can better estimate the risk of recurrence and potentially avoid overtreating patients at low risk for recurrence.
A randomized study from the Intergroup was launched in 2000 to better characterize the benefit of PMRT in women with T1–T2 lesions and one to three nodes. This study was designed to randomize women, after mastectomy, axillary dissection, and chemotherapy, to PMRT to the chest wall and regional nodes (supraclavicular/axillary apex and IMN chain) but closed due to poor accrual. It is unlikely that this study will be attempted again, and Level I evidence for this particular group of women will not be available.
More modern series from Memorial Sloan Kettering Cancer Center (MSKCC) and MD Anderson have shown that it is possible to identify patients at low risk for locoregional recurrence after mastectomy and chemotherapy. Moo and coworkers from MSKCC studied a group of 1087 women with T1/T2 tumors and one to three positive nodes treated at MSKCC from 1995 to 2006. Of this group, 924 did not receive PMRT and 163 received PMRT. Patients who received PMRT were younger, had larger tumors, higher grade, lymphovascular invasion, extranodal extension, and a greater number of nodes. The 5-year rate of locoregional recurrence was equally low in these two groups of patients: 3.2% for RT versus 4.3% for no RT. This suggests that the vast majority of women with one to three nodes do not require PMRT, and those with higher-risk features can have their risk effectively reduced with radiation. This study should not be used to justify that PMRT is not needed in women with one to three nodes. Rather, it supports the selective use of PMRT/RNI in women with risk factors identified in the original MD Anderson and British Columbia papers.
In 2015, three large national trials looking specifically at the question of RNI in lower-risk patients were reported. The data from these trials have lent more support for the use of RNI in women with one to three nodes, although there is still clearly controversy. Given that both also support the use of IMN irradiation (even in relatively low-risk patients), this will likely further the increasing trend of IMN irradiation in the United States. In 2006 a patterns-of-care study showed that IMN irradiation was relatively rare for women with less than 4 nodes. A more recent survey (unpublished Radiotherapy Comparative Effectiveness Consortium [RADCOMP] survey, 2015) showed that there has likely been some more adoption of IMN irradiation in the United States over the past decade.
The NCIC-CTG MA 20 randomized high-risk, node-negative or node-positive breast cancer patients who underwent breast-conservation surgery to whole breast irradiation or whole breast irradiation and regional lymph node irradiation, which included the internal mammary nodes in the first three intercostal spaces, the supraclavicular, and high axillary lymph nodes. High-risk patients were defined as having a 5-cm or larger breast primary or a 2-cm or larger primary with fewer than 10 lymph nodes removed and one of the following higher-risk features: ER-negative, grade III disease, or lymphovascular invasion. Median patient age was 53 years old, and 85% of patients had one to three positive lymph nodes. The primary tumor was larger than 2 cm in 48% of patients, and 43% of patients had grade III disease. Fifty percent of patients had only a single positive node and 75% of patients had ER-positive disease. Nearly all patients received adjuvant chemotherapy (91%), and the majority received adjuvant endocrine therapy (77%). This trial failed to show a survival benefit, although it did show benefits in locoregional control (95.2% vs. 92.2%), disease-free survival (82% vs. 77%), and distant disease-free survival (86.3% vs. 82.4%). In a prespecified subgroup analysis, patients with ER-negative disease in the nodal irradiation group had a higher 10-year rate of overall survival than did patients in the control group (81.3% vs. 73.9%), a difference that approached statistical significance (hazard ratio 0.69; 95% CI 0.47–1.00; p = .05).
Ten-year results from the EORTC 22922 trial were also published in the New England Journal of Medicine in 2015 and demonstrated similar results. This trial found that the use of an internal mammary and medial supraclavicular field resulted in a statistical reduction in regional recurrence (4.2% vs. 2.7%) and distant recurrence (19.6% vs. 15.9%), and a trend toward improved overall survival (82.3% vs. 80.7%, respectively; p = 06). Eligible patients had pathologically positive axillary lymph nodes or were node negative with central or medial tumors. Median patient age was 54 years. Sixty percent had pT1 tumors, 45% of patients were N0 and an additional 55% had one to three positive nodes, and 74% of patients had ER-positive disease. More than 90% of patients in each study group underwent partial or total axillary lymph node dissection, and the majority of patients received systemic therapy. Although details regarding lymphovascular invasion, extranodal extension, and tumor grade are not available, this seems to be a relatively low-risk patient population to demonstrate a benefit of IMN RT. In the United States, it is relatively rare to offer node-negative patients with small tumors IMN RT. Thus it could be extrapolated that if a group of higher-risk women were included, with higher rates of IMN involvement, the absolute benefit of RT would be greater with a similar relative-risk reduction.
The Danish Breast Cancer Group (DBCG) published a large population-based study demonstrating a survival benefit for IMN RT versus no IMN RT. Although this study was not randomized, its unique design was able to account for biases. In 2003 a decision was made to abandon IMN RT for all left-sided women based on a concern over cardiotoxicity risks of IMN RT and anthracycline use, but to continue to treat all node-positive patients with right-sided breast cancer with IMN RT. Thus although this was not a randomized trial, the unique study design had a naturally random allocation of patients to IMN RT or not. Between 2003 and 2007 3089 patients were treated as part of this study, with 1492 allocated to receive IMN RT based on right-sided disease and 1597 allocated to no IMN RT based on left-sided disease. The patient characteristics were nearly identical between the two groups, as would be expected from a randomized trial. In this study, 60% of patients had one to three positive nodes, 40% were medially located, 42% had T1 tumors, 29% were grade 3, and 20% were ER negative. IMN RT reduced 8-year breast cancer mortality from 23.4% to 20.9%, and overall survival was improved from 72.2% to 75.9% with IMN RT. Subset analysis showed that the benefit was greatest for patients with medially located tumors and four or more positive nodes, with the smallest benefit for women with one to three positive nodes and laterally located tumors. Based on surgical data, it would be expected that patients with medial tumors and larger axillary burden are at greatest risk for IMN involvement.
Although the aforementioned trials have shed significant light on the role of RNI in women with intermediate-risk disease, the community is struggling with the different conclusions reached regarding the need to treat the regional nodes in women with one to three positive lymph nodes, when comparing the Z0011 study to the MA 20 and EORTC trials discussed earlier. However, entry criteria and patient characteristics for these three studies were not identical. The Z0011 study was limited to women with T1–T2 lesions, and the majority, 70%, had T1 breast cancers. In comparison, the EORTC and MA 20 trials allowed up to T3 lesions, with the proportion of T1 cancers in the MA 20 trial about 50%, and in the EORTC trial about 60%. Also, 83% of Z0011 patients were ER positive, an important favorable prognosis marker, compared with only 75% in MA 20. Adjuvant therapy was used in a greater proportion of the Z0011 patients, 96% to 97%, compared with 85% in the other two trials. So in part, the different conclusions can be explained by the Z0011 patients having both a more favorable breast cancer, and a higher likelihood of receiving adjuvant therapy, a treatment recognized to contribute to local and regional control, than MA 20 and EORTC patients.
Accepting the Z0011 surgical conclusions, what should be considered when designing the breast radiation fields? For those women with breast cancer characteristics similar to the more favorable women in the Z0011 study, namely those with T1 lesions, which are ER positive, with involvement of only one axillary lymph node, and who will also be receiving appropriate systemic treatment, the intended breast tangent fields in the Z0011 study should yield the same excellent local-regional control as was demonstrated in the Z0011 study. However, because approximately 50% of patients received high tangents and nearly 20% received a third supraclavicular field, it is possible that it was primarily the 40% of patients with micrometastatic disease who only received breast radiation.
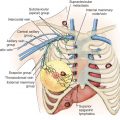
For patients with larger tumors, those with very extensive replacement of the involved sentinel nodes or with extranodal extension, and those with high-grade or estrogen-negative tumors, deliberate inclusion of the lymph nodes at level I–II is a radiation technique to consider because those patients will be at higher risk. Factors such as oncotype score, intrinsic subtype, lymphovascular invasion in the tumor specimen, young age, and ability to tolerate appropriate systemic therapy can also guide the radiation oncologist to design appropriate regional nodal radiation fields in addition to breast radiation. Once a decision is made to treat the nodes, technique is driven by the decisions to include only the level I–II nodes, which can usually be included in the “high-tangent” breast fields, and to include as well the supraclavicular regions and possibly the internal mammary nodes. The techniques discussed in the MA 20 and EORTC section of this chapter are appropriate when more extensive nodal coverage is planned; key to this is contouring the nodes to be included in the patient’s treatment plan.
In summary, the Z0011, AMAROS, MA 20, and EORTC trials did not address exactly the same patient populations, and were designed to ask quite different treatment questions. Thus patients with a limited number of positive axillary nodes after breast conserving surgery should be considered in the context of these trials and treated in a way that is consistent with the trial that is most representative of their disease characteristics.
The Z0011 and IBCSG clearly demonstrated that some patients, especially those with micrometastatic disease undergoing breast conservation therapy, do not require axillary surgery or radiation. For patients with slightly higher-risk disease, AMAROS and the modified Z0011 RT fields showed that axillary radiation can safely replace axillary dissection in many patients with one to two positive sentinel nodes and T1–T2 tumors. For patients who still undergo a complete axillary dissection and have one to three positive nodes, the MA 20, EORTC, and DBCG trials established that RNI including IMN RT will improve outcomes for some patients with one to three nodes and T1/T2 tumors, although these studies did not clearly answer which patients need IMN RT and which do not. However, based on the consistency of these results, it is clear that IMN RT can improve breast cancer and overall survival in some patients, and it is important not to undertreat women who can benefit from this. Several recent editorials have shown that there is still significant uncertainty on how to manage the axilla for intermediate-risk patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree