Introduction
Neuropsychiatric sequelae of viral infections have been described in the literature and are well known from studies of influenza pandemics , , human immunodeficiency virus (HIV) infections, and viral encephalitis. Perhaps the most researched neuropsychiatric disorder after a viral infection was the development of encephalitis lethargica after the Spanish flu outbreak in the last century. Encephalitis lethargica had prominent parkinsonian symptoms, psychosis, and catatonia.
Prominent neuropsychiatric syndromes were described in two more current coronavirus pandemics: severe acute respiratory syndrome (SARS) in 2002 and Middle Eastern respiratory syndrome (MERS) in 2012. In the acute stage of SARS or MERS infections, confusion (suggesting delirium) occurred in 27.9% of patients, and depression, anxiety, and insomnia were relatively common. In follow-up studies of patients who had contracted SARS or MERS that ranged from 6 weeks to 39 months after recovery from the acute infection, more than 15% of patients reported sleep disorders, recurrent traumatic memories, emotional lability, impaired concentration, fatigue, or impaired memory. Survivors of critical illnesses had the most risk for psychiatric comorbidities at 1 year, with about one-third experiencing significant anxiety, depression, or posttraumatic symptoms.
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first identified in Wuhan, China in late 2019, and it soon became clear that the virus can spread beyond the respiratory tract to other vital organs, including the central nervous system (CNS). Clinical evidence of CNS involvement was substantiated by the detection of coronaviruses in the cerebrospinal fluid of patients with neuropsychiatric sequelae ; early cases of dizziness, headache, delirium, cerebrovascular disease, encephalopathy, neuromuscular disorders, anosmia, and ageusia , ; and psychiatric disorders, including suicides among older adults.
In terms of psychiatric disorders, the infection presents two potential risks. The risk for psychiatric sequelae is clearly increased by the psychosocial and economic stress associated with the COVID-19 pandemic. In addition, the viral infection of the CNS, the hyperinflammatory state, and medications used to treat the infection (e.g., exogenous corticosteroids) increased the risk for the development of acute psychiatric disorders.
The COVID-19 pandemic is associated with an increase in psychiatric symptoms, most notably anxiety, depression, and posttraumatic stress disorder (PTSD), and these symptoms are disabling. , , Some patients who recovered from the acute phase of COVID-19 had continued neuropsychiatric symptoms. These patients were described in the literature as “long haulers,” who over time develop a variety of neuropsychological symptoms, including poor concentration (or “brain fog”), fatigue, and multiple psychiatric symptoms such as depression, anxiety, PTSD, obsessive-compulsive symptoms, psychosis, and an increased risk for suicide ( Fig. 12.1 ). These patients also have symptoms that can masquerade as psychiatric symptoms (e.g., chronic fatigue, insomnia, concentration difficulties) and lead to significant disability. , This chapter will present the available data on both the acute and long-term incidence of psychiatric diagnoses related to SARS-CoV-2 infections.
Delirium
Coronaviruses target the angiotensin-converting enzyme-2 receptor (ACE2), which is found on glial cells in the brain. SARS-CoV-2 has been shown to enter the CNS though the olfactory epithelium or cribriform bone, by a breakdown of the blood–brain barrier during a viremic phase of the illness, or by peripheral nerve terminals. Once the virus enters neuronal cells, viral RNA replicates and is released into the cerebrovascular circulation.
Delirium is an acute sign of brain dysfunction and has been reported in up to 50% of mechanically ventilated patients. In some patients, particularly the elderly, delirium may be the initial or only presenting symptom of acute COVID-19. , Awareness of delirium as a common symptom of COVID-19 is even more essential in these patients for early diagnosis, treatment, and prevention of further spread of the virus.
In a retrospective study in Italy, over a quarter of patients hospitalized for neurological conditions associated with COVID-19 experienced delirium. This rate was over three times the incidence of delirium in patients hospitalized for other neurological conditions who had not contracted COVID-19 during the same time. A group in the United Kingdom (UK) reported that over 30% of patients hospitalized with COVID-19 experienced altered mental status and more than half (59%) met criteria for a psychiatric diagnosis, including psychosis and affective symptoms. About half of the patients with altered mental status were under 60 years old.
Delirium is associated with higher mortality and long-term cognitive and functional decline. COVID-19 patients are at particularly high risk for delirium given that they are often prescribed higher doses of sedating medication (e.g., benzodiazepines and propofol) than other mechanically ventilated patients and have a higher risk for delirium because of multiple medical complications (e.g., neuroinflammation, cerebrovascular accidents from hypercoagulability, multisystem organ failure, and social isolation). Agitated delirium tends to be the more prominent type of delirium in patients with COVID-19 and has been reported in nearly 70% of patients hospitalized with severe COVID-19 symptoms. This type of delirium is more overt and easily identifiable than hypoactive delirium, and therefore it is likely that patients with hypoactive delirium are underreported.
COVID-19 patients are also at a higher risk for hypoxic brain injury from an immune-mediated reaction described as a cytokine storm. A cytokine storm is the result of the inflammatory response to the infection and can result in vascular leakage and end organ damage. Delirium also can be the primary manifesting syndrome in COVID-19 patients even before the respiratory symptoms are apparent.
Importantly, delirium during hospitalization in COVID-19 patients is linked to an increased risk for death during hospitalization and an increased need for support on discharge from the hospital. Physical functioning after discharge was notably impaired in patients who were diagnosed with delirium during their hospitalization. A COVID-19 post–intensive care syndrome has been identified that includes cognitive impairment, depression, anxiety, and physical signs such as weakness.
In a multicenter cohort study conducted in 69 adult intensive care units (ICUs) with 2000 patients across 14 countries (half the patients were in Spain) admitted with COVID-19, investigators identified variables associated with delirium and coma. In this study, 55% of patients were delirious for an average duration of 3 days. Significant factors associated with delirium included older age, higher Simplified Acute Physiology Score (assessing the risk for death in ICU patients), male sex, smoking or alcohol abuse at baseline, use of vasopressors on day 1, and invasive mechanical ventilation on day 1 (all P < .01). In this study, the investigators identified two modifiable risk factors associated with a decreased incidence of delirium: lower benzodiazepine use and more frequent family visitations in the ICU (either in person or virtually). The investigators outlined interventions to lower the incidence of delirium, including decreasing sedatives, increasing mobility, breathing trials off ventilation, and encouraging families to visit. Other strategies could include circadian rhythm regulation using medications such as melatonin.
The US Food and Drug Administration has not approved any medications to treat delirium. The primary interventions recommended are behavioral, including family involvement. Off-label medication treatments used to manage COVID-19–related delirium include alpha-2 agonists, low-potency antipsychotics, valproic acid, and trazodone.
Impact of Preexisting Psychiatric Disorders on COVID-19 Outcomes
The impact of a preexisting mental health disorder on the emergence of psychiatric symptoms during or after SARS-CoV-2 infection is well documented. Patients with severe mental illness are at particularly high risk for contracting COVID-19 and transmitting the virus. These patients may not adhere to protocols to decrease transmission (e.g., mask wearing), have less access to medical clinics for vaccinations and medical care, and are more at risk for an exacerbation of their underlying psychiatric symptoms.
Two large-scale meta-analyses found associations between COVID-19 mortality and preexisting psychiatric conditions. A recent meta-analysis of studies from seven countries and over 19,000 patients with COVID-19 found an increased risk for mortality (odds ratio [OR], 1.75) in patients with a mental health condition. Patients with more severe psychiatric conditions, such as schizophrenia and bipolar affective disorder, were over two times at risk for mortality from COVID-19 compared to patients without a mental health diagnosis.
A meta-analysis compiling data from 21 studies with 90 million COVID-19 patients detected a higher likelihood of hospitalization and death if a preexisting affective disorder was present (OR, 1.31 and 1.51, respectively). There was no association between mood disorders and risk for infection of SARS-CoV-2. The data from these two meta-analyses make clear that patients with preexisting psychiatric disorders are at high risk for hospitalization and death when infected with SARS-CoV-2. The risk for significant short- and long-term psychiatric symptoms in an individual patient with a premorbid psychiatric diagnosis who contracts SARS-CoV-2 is clearly increased, and these patients should be monitored carefully.
Anxiety, Depression, Mania, and Suicide Risk
Psychopathology is relatively common in patients recovering from COVID-19, with more than half showing significant symptoms of at least one psychiatric disorder 1 month after infection (i.e., PTSD, depression, anxiety, or obsessive-compulsive symptoms). Multiple other studies also found high rates of depression and anxiety after SARS-CoV-2 infection. The reasons for patients developing anxiety and depressive symptoms during and after COVID-19 disease are multifactorial. A previous psychiatric diagnosis, , , female sex, , , , younger age, , lower socioeconomic status, , , and unemployment , are all linked to higher rates of psychological distress after COVID-19. Interestingly, the prevalence of depression and anxiety was similar in health care workers with COVID-19 compared with the general public in one meta-analysis and other reviews, although nurses had a high burden of mood symptoms. ,
The medications used to treat COVID-19 include several with known adverse drug reactions, including mania or hypomania. High-dose steroids are heavily used in hospitalized patients with severe COVID-19, particularly those requiring supplemental oxygen, and case reports suggest that some patients developed mania with grandiosity, hyper-religiosity, elevated energy, and insomnia severe enough to warrant psychiatric hospitalization and treatment with psychotropic medication, including mood stabilizers and antipsychotics. , Furthermore, quinolone antibiotics, which have been initiated to treat secondary infections in patients with COVID-19 are also known to provoke hypomania and euphoria in some patients. At the time of writing, no reports of new-onset mania have been reported in patients with COVID-19 who did not receive medications known to elicit manic symptoms.
Suicide risk is also increased in patients with COVID-19 infections, , , although the data are still preliminary. The precipitants for a potential increase in suicide rates secondary to the pandemic are multifactorial and related to social isolation, socioeconomic stresses such as high rates of unemployment, and the risk for psychiatric symptoms in persons with preexisting psychiatric disorders. , Insomnia is also associated with COVID-19 and can significantly increase the risk for suicide; it should be evaluated and addressed in this patient population.
There are protective factors to prevent the development of depression and anxiety after COVID-19, including sufficient medical resources to manage the illness, current information, confidence in the reports on the status of the pandemic, , being married, connection to family, and exercise. Social isolation is a factor that can potentially be addressed to decrease the risk for depression and anxiety. , The dyad of fear and isolation is a clear precipitant to the development of anxiety, depression, and potentially suicide in this patient population.
There are limited medication trials for anxiety and depression related to COVID-19, but there would be no reason to think that the psychotropic medications used to manage major depression, PTSD, and anxiety disorders would not be effective in this population. In fact, serotonin reuptake inhibitors have been shown to be protective in developing COVID-19 symptoms.
Posttraumatic Stress Disorder and Trauma-Related Symptoms
PTSD in COVID-19 survivors has been diagnosed as early as 7 weeks after discharge from the hospital. At 3 months, 10% of patients who had been hospitalized for COVID-19 met the criteria for PTSD. By 4 months after discharge, 17% of patients who had been hospitalized for COVID-19 had symptoms of PTSD. One study comparing patients who required hospitalization to those who did not followed patients between 1 and 6 months after COVID-19 diagnosis and found no significant difference in the prevalence of PTSD between these groups.
Longer-term symptoms also have been reported in a cross-sectional survey of 284 patients who were followed an average of 50 days after their COVID-19 diagnosis. In this survey, significant PTSD symptoms (assessed by the self-report questionnaire the Impact of Event Scale–Revised) were the most common psychiatric condition and moderate to severe PTSD was associated with an increase in suicidal thoughts. Risk factors for PTSD symptoms also included female sex, a history of traumatic events, how concerned the patient was that COVID-19 was a serious threat, and feeling stigmatized by contracting the virus.
Young adults (18–30 years old) reported particularly high rates of PTSD symptoms, with 31.8% of patients in the sample scoring 45 or greater on the PTSD Checklist-Civilian Version (>33 is considered clinically significant symptoms on this scale). In this cross-sectional online study of PTSD symptoms, the respondents also had high levels of depression and anxiety and psychiatric symptoms were associated with loneliness, COVID-19 concerns, and low distress tolerance. Social support after contracting the virus, particularly from the patient’s family, was shown to be protective.
Psychosis and Catatonia
The risk for psychosis has been documented in previous flu epidemics. Corticosteroids have been a significant contributor to psychosis and mania in previous viral pandemics.
Rare cases of brief psychotic disorder in the setting of acute COVID-19 infection are documented in a single-site retrospective study in Spain. Ten patients without previous episodes of psychosis, severe mental health history, or substance use history who had contracted COVID-19 were evaluated for new-onset psychosis. Within this study, delusions (particularly those of persecution, prejudice, and referential beliefs) were present in all of the psychotic patients. The majority (60%) of patients with psychosis had difficulties with orientation and attention, and many reported auditory (40%) or visual hallucinations (10%). The majority (80%) of patients did not develop psychosis for several weeks after physical symptoms of COVID-19 and had resolution of psychosis with low doses of antipsychotics within 2 weeks. Disorientation and inattention resolved faster than delusions. In this study, iatrogenic factors could not be ruled out, because most patients had received corticosteroids and hydroxychloroquine, which have been associated with psychosis. There has been a case of brief psychotic disorder in a patient with COVID-19 who had not been exposed to any medications known to precipitate psychosis.
A surveillance study of over 150 patients with COVID-19 in the United Kingdom revealed that 43% of patients who developed neuropsychiatric symptoms with acute SARS-CoV-2 infection had new-onset psychosis, which was a considerably higher incidence compared with the development of mood disorders in this patient population.
Catatonia has been observed in patients with acute COVID-19. , Catatonia is a psychomotor condition that in itself may be life threatening. It can manifest from a medical condition such as COVID-19 but also may be a symptom of an underlying psychiatric state. Patients classically may be mute and rigid, stop eating and drinking, and have autonomic instability. In a review of 10 cases of catatonia in patients with COVID-19, all patients exhibited akinetic mutism. Patients with catatonia associated with COVID-19 have reportedly responded to benzodiazepine treatment, the standard of care.
Psychiatric Symptoms Directly Linked to Viral Infection
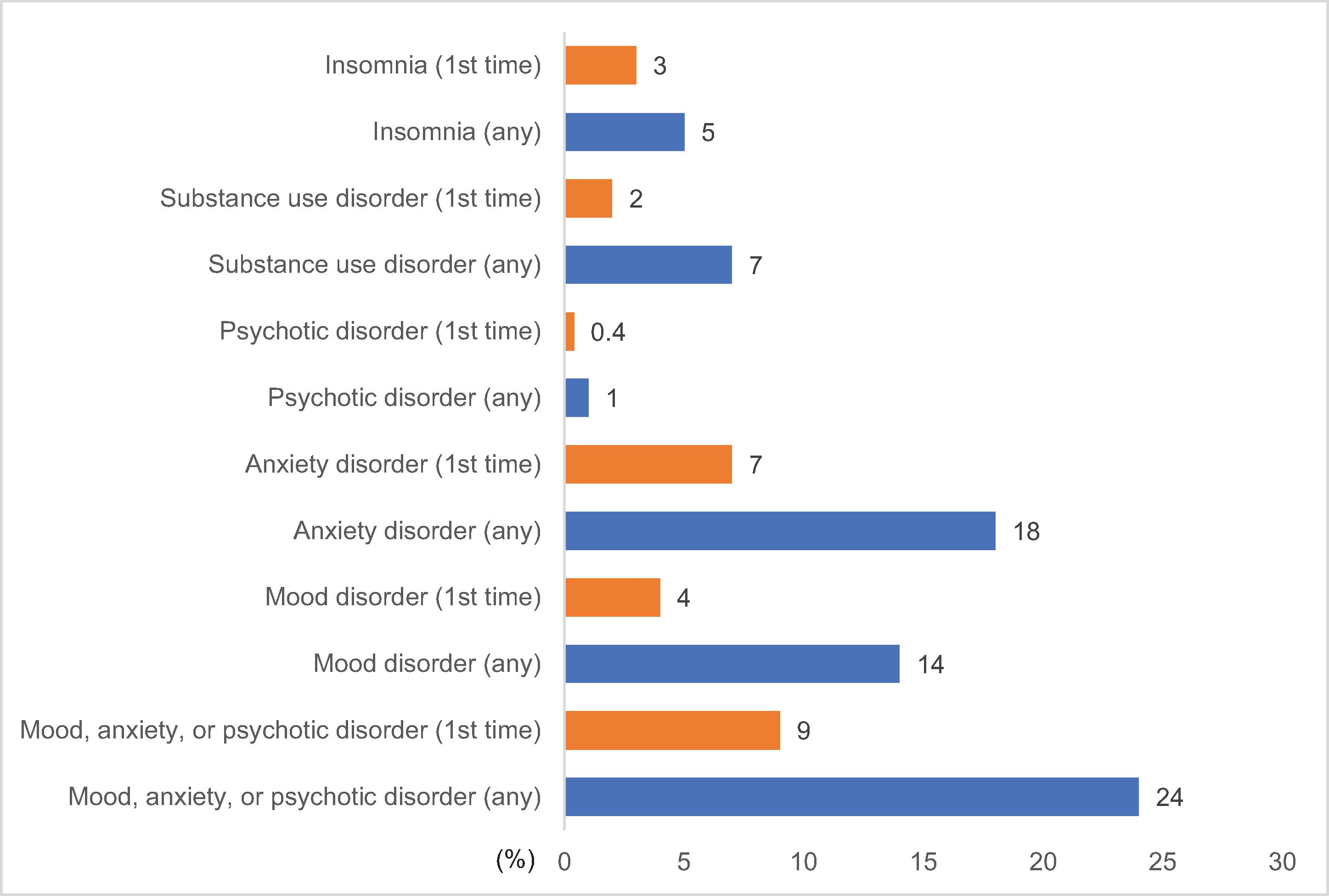
Not surprisingly, the pandemic in and of itself has created a “second wave” of psychiatric morbidity in all populations as a result of the stress of social isolation, persistent feelings of uncertainty or loss of control, sense of powerlessness, and secondary traumatization. Therefore it can be difficult to decipher how much of the psychiatric sequelae in patients with COVID-19 is related to the stress of the pandemic compared with direct effects from the virus. Several studies have provided evidence that suggests the viral infection plays a significant role in the relatively high incidence of psychiatric symptoms.
Hospitalized patients with COVID-19 have been compared with age- and sex-matched patients hospitalized during the pandemic for other respiratory illnesses. Patients with COVID-19 had significantly higher rates of mood, anxiety, or psychotic disorders compared with controls.
Higher levels of the inflammatory marker C-reactive protein were detected in COVID-19 survivors who developed severe depression compared with normal controls, suggesting that the inflammatory response from the virus may be inducing neuropsychiatric symptoms. In this study, duration of hospitalization did not have an impact on risk for depression, suggesting that the hospital experience and possibly severity of COVID-19 (if duration is a proxy for disease severity) may not be contributing to development of depression.
Conclusion
Significant psychiatric comorbidities are relatively common in patients with COVID-19 and can lead to significant disability, which can persist for months to years in vulnerable populations. There are no established somatic treatments, although using selective serotonin reuptake inhibitors and evidenced-based psychotherapies such as cognitive-behavioral therapy and prolonged exposure therapy are reasonable approaches. However, data to support their efficacy in COVID-19 are limited.
There are also public health approaches that have been shown to be effective in limiting the psychiatric comorbidities of COVID-19. Decreasing social isolation (e.g., providing Meals on Wheels, telepsychiatry groups, visits by family members), increasing knowledge about the pandemic in regular and reliable public service announcements, and decreasing stigma associated with contracting the virus should all be addressed by broader public health measures. Disseminating reliable information on the pandemic with the proliferation of social media has been challenging and should be addressed. The public should be confident in the information they are receiving and referred to the Centers for Disease Control and Prevention and other public health agencies that are current and reliable. This may be difficult but should be immediately addressed.
Stigmatization for contracting the virus will be particularly difficult to address in patients who declined to get vaccinated and contracted the disease. This may be a problem not only for the general public but also health care workers and is reminiscent of the issues surrounding other “self-induced” illnesses such as cirrhosis in an alcoholic patient or lung cancer in a chronic smoker. Perhaps public service announcements or other information outlining why people declined the vaccination would be helpful in personalizing an individual’s decision.
There are also specific patient groups that should be targeted as at high risk for developing psychiatric symptoms, including those patients with previous psychiatric diagnoses or presently in psychiatric treatment. Female sex was a significant risk factor for psychiatric symptoms and could lead to some targeted strategies such as asking gynecologists to screen COVID-19–positive patients carefully for psychiatric symptoms.
Clearly, physicians managing patients with acute COVID-19 should be alert to the potential for the emergence of psychiatric symptoms both in the acute phase and over time. These patients are at significant risk for disabling psychiatric syndromes. Decreasing the psychiatric comorbidities should include public health measures (e.g., decreasing social isolation, increasing accurate information on the pandemic) and monitoring patients for symptoms, particularly those in high-risk populations (e.g., premorbid psychiatric conditions, low socioeconomic status). Treatment with antidepressant medications and psychotherapy should be considered in symptomatic patients.
REFERENCES
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree