The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) causes a highly contagious disease called CO rona VI rus D isease 2019 (COVID-19). The virus was first reported in Wuhan city, Hubei Province of China in December 2019; in less than 3 months it spread globally and was declared a global pandemic by the World Health Organization (WHO) on March 11, 2020. By March 24, 2020, the novel SARS-CoV-2 had been observed in all seven continents and in 222 countries and territories, with 163,788,738 confirmed cases and a mortality rate of 2.1%.
Symptoms of SARS-CoV-2 infection include fever or chills, cough, shortness of breath, fatigue, muscle or body aches, headache, loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, and diarrhea. Severe cases often develop pneumonia, acute respiratory distress syndrome (ARDS), and multiple organ failure.
Less than 2 weeks after the Wuhan Municipal Health Commission announced the detection of the first cases of coronavirus-associated pneumonia, the WHO issued comprehensive technical guidance on how to detect, test, and manage potential cases based on available information. The first official confirmed novel coronavirus case outside of Wuhan was recorded in Thailand on January 13, 2020, and the United States reported its first case on January 21, 2020. Approximately 3 weeks later, on February 11, 2020, the WHO announced that the disease caused by the novel coronavirus would be named COVID-19. Within 5 days, significant transmission of SARS-CoV-2 and increasing cases of COVID-19 were reported in Iran, Italy, and Spain, and the first cases were reported on the African continent on February 25, 2020.
By March 7, 2020, the total number of confirmed COVID-19 cases worldwide had reached over 100,000. The WHO, alarmed at the rapidity of spread and severity of disease, issued a statement calling for “action to stop, contain, control, delay, and reduce the impact of the virus at every opportunity,” and on March 11, 2020, the WHO announced that COVID-19 was officially a “pandemic.” One month later, on April 4, 2020, infections had mushroomed 10-fold to over 1 million cases of COVID-19 worldwide.
The virus has spread in stages known as surges or waves because of their episodic increase in cases, peak, sometimes a plateau, and gradual decline. These waves of viral transmission can be isolated and studied to reveal the details of the spread during these specific periods and determine any precipitating events or related factors. A study conducted with COVID-19 patients before January 20, 2020 found that the average incubation period for the disease was 5.2 days (95% confidence interval [CI], 4.1–7.0) and the 95th percentile was 12.5 days; the number of individuals likely to be infected by each case (the R 0 ) was estimated to be 2.2. A later review found R 0 values ranging from 1.4 to 4.6, with a mean of 3.28. The epidemic doubling time was 7.4 days; however, doubling time will vary with the intensity of the mitigation efforts.
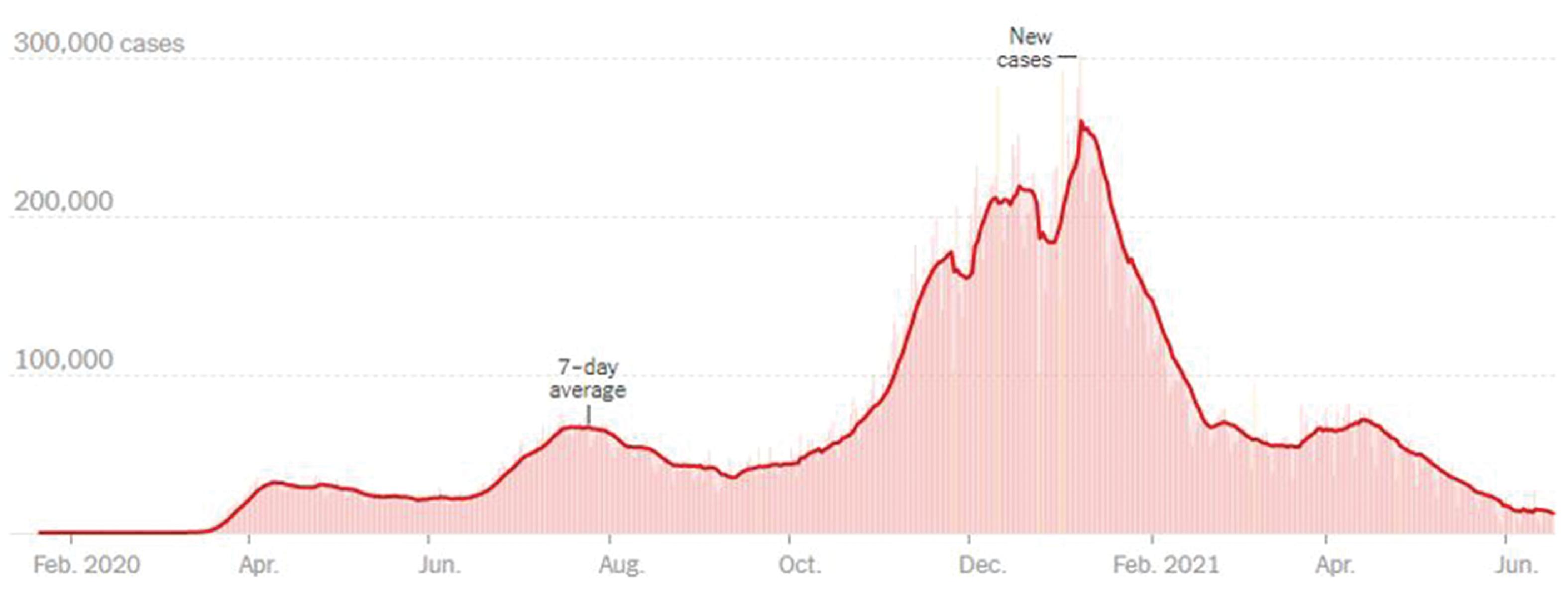
The COVID-19 pandemic has been characterized by several waves that differ in size and intensity across countries and continents. A wave is over when the number of new cases per day declines and then plateaus. “Flattening the curve” is a phrase that was commonly used in the early months of the pandemic, when efforts were focused on preventing transmission because health care facilities were in jeopardy of being unable to care for all cases. Flattening the curve means reducing transmission so that the number of daily new cases is reduced and maintained over a longer period. Locales that observed strict social distancing and other mitigation efforts typically observed flattening of their first wave of the pandemic ( Fig. 1.1 ).
In March 2020, Italy, Iran, and New York City were the hardest-hit regions, with daily cases peaking at 6557 new cases per day in Italy, 3186 cases day in Iran, and 21,000 new cases per day in New York City. In April 2020, COVID-19 cases started to spike in Brazil, and by mid-May COVID-19 cases were surging in India. At the same time, several countries, including Spain, Iran, Italy, Denmark, Israel, Germany, New Zealand, and Thailand, began to ease their lockdown restrictions because of reduction in cases. The total number of cases surpassed 5 million globally on May 21, 2020, a number that had doubled to 10 million by the end of June 2020. Globally, COVID-19 deaths had surpassed half a million people by June 28, 2020, according to the Reuters tally, but doubled to over 1 million on September 18, 2020, 191 days after the WHO declared the novel coronavirus outbreak a global pandemic.
In October 2020, the United States entered its third surge of coronavirus cases, the beginning of its deadliest phase yet. The United States accounted for the highest number of cases and deaths in the world at this point, and globally cases surpassed 50 million by early November 2020.
As of May 18, 2021, over 163 million people had tested positive for COVID-19 and over 3.3 million people had died from the disease across the globe. To date, the three countries most affected by COVID-19 infections are the United States (confirmed cases 32,356,034 and 1.8% mortality), India (confirmed cases 23,702,832 and 1.1% mortality), and Brazil (confirmed cases 15,209,990 and 2.8% mortality). Since March 2020, the overall case fatality rate (CFR) was reported to be around 2.1%; as of May 17, 2021, the CFR has decreased to 0.87% ( Fig. 1.2 ).

The most significant factor in controlling the pandemic has been the introduction of COVID-19 vaccines. The COVAX Facility, a system designed to equitably distribute COVID-19 vaccines worldwide, was developed as testing of COVID-19 vaccine candidates was ongoing. By July 15, 2020, the COVAX Facility had been accepted by over 150 countries, representing over 60% of the world’s population. Pfizer/BioNtech’s COVID-19 vaccine was authorized for use in the United Kingdom on December 2, 2020, and the US Food and Drug Administration (FDA) issued emergency use authorization (EUA) for the Pfizer/BioNtech vaccine on December 11, 2020, and EUA for Moderna’s COVID-19 vaccine on December 18, 2020. Immediately after approval for use, these vaccines were being administered to health care workers and other priority groups. At the end of February 2021, the one-dose Johnson & Johnson vaccine was given EUA by the FDA. As of this writing, individuals as young as 5 years old may receive a COVID-19 vaccine in the United States. Early reports find high vaccine effectiveness for the COVID-19 two-dose vaccines.
Because of the propensity of viruses to mutate, new coronavirus variants are already emerging. Currently six coronavirus variants that are causing significant numbers of symptomatic infections have been identified and are variants of interest or variants of concern. The B.1.1.7 variant was first detected in the United Kingdom but has since been reported in the United States (December 2020). The B.1.351 variant was initially detected in South Africa in December 2020 and was identified in the United States at the end of January 2021. The P.1 variant was first detected in travelers from Brazil at an airport in Japan in early January 2021 and found to be circulating in the United States later that month. The B.1.427 and B.1.429 variants were first identified in California in February 2021 and were classified as variants of concern in March 2021. The B.1.617 variants were first detected in December 2020 in the state of Maharashtra, India. They are currently listed as variants of interest. These variants are concerning because of evidence that they may be more contagious, more virulent, less susceptible to treatment, and/or capable of causing reinfections.
In the following sections, the epidemiology of COVID-19 is presented by continent, starting from its occurrence in Asia. Within each continent, selected countries are discussed as examples of different approaches to mitigation and control of the SARS-CoV-2, especially those with high morbidity and mortality rates. The second part of the chapter deals with risk factors for COVID-19.
Asia
China
The first cases of novel coronavirus (SARS-CoV-2)–infected pneumonia occurred in Wuhan, Hubei Province, China, in December 2019. Morbidity was low; 55% of the patients who developed symptoms before the end of December 2019 were related to exposure at Wuhan’s Huanan Wholesale Seafood Market. The first stage of epidemic transmission was primarily a local outbreak among people with a direct contact history at the seafood market. In the second phase, interpersonal and cluster transmission occurred in multiple communities and families in Wuhan in early January. This was the community dissemination stage of the epidemic. During the second half of January, in particular after the January 25, 2020 celebration of the Chinese New Year, there was a remarkable increase in the number of infected patients in affected cities outside Hubei Province. These cases were attributed to population movement in anticipation of the New Year.
An interim report by an independent panel commissioned by the WHO , found the initial Chinese response to the new disease to be inadequate. In response, China imposed a city-wide, strictly enforced lockdown of Wuhan that shocked the rest of the world. Nearly 11 million people were quarantined, and face masks and social distancing were mandatory. Hundreds of field hospitals were erected within days to deal with overwhelming cases of COVID-19. Despite the Wuhan lockdown, COVID-19 outbreaks occurred in other major Chinese cities such as Beijing and Shanghai. These were quickly controlled using the same immediate lockdowns and swift mass testing. Entry into China was managed by introducing new restrictions and quarantine control. Although considered to be harsh, these measures eventually proved effective in mitigating the spread of the virus. From January 3, 2020 to May 21, 2021, there have been 105,647 confirmed cases of COVID-19, with 4861 deaths reported to the WHO.
Japan
The first SARS-CoV-2 infection was confirmed in Japan on January 16, 2020, in a person who had returned from Wuhan, China. Multiple cases of COVID-19 were identified by the end of February 2020 throughout Japan. A second outbreak of infection occurred in Japan around mid-March 2020. However, the level of testing for SARS-CoV-2 conducted in Japan during the two initial outbreaks of COVID-19 was lower than in other countries. The total number of cases of COVID-19 reported in Japan is 97,074, with one of the lowest COVID-19 death rates per capita (1.356 deaths/100,000 population).
Vietnam
Between the first case being reported on January 23, 2020 and August 13, 2020, Vietnam had 911 confirmed cases with 21 fatalities (2% case fatality rate). In response, the Vietnamese government took draconian measures to curb the infection rate, including social distancing, locking down businesses, suspending entry of all foreigners from March 2020 until further notice, and closing the border between Vietnam and Cambodia. These measures were effective, and Vietnam reported 6314 confirmed cases and 46 deaths as of May 21, 2021. , However, from May 12, 2021 onward, community transmission cases have been reported from Bac Giang, Hung Yen, Hai Duong, Dien Bien, and Hanoi.
Vietnam reported its first case of the coronavirus variant from the United Kingdom on January 2, 2021 and has reinstituted closures of businesses such as movie theaters and sidewalk cafes, schools, and public transportation and banned inbound flights from the United Kingdom and South Africa.
Taiwan
Taiwan had been spared the worst of the pandemic by containing the spread of COVID-19 among its population of 24 million without a complete lockdown. The island recorded 1128 cases and 12 deaths by the end of April 2021. Most of these cases had been imported from travelers. Although Taiwan is currently experiencing a surge, reporting more than 6761 cases and 59 deaths as of May 27, 2021, these numbers are significantly smaller than those in most countries and territories worldwide.
The newest outbreak, causing over 200 daily cases in the week of May 17, 2021, is thought to have started because authorities had relaxed quarantine requirements for airline crew members in mid-April 2021. New social-distancing rules limiting social gatherings, closing some businesses, and tightening border restrictions have been implemented.
India
The first case of COVID-19 in India was reported on January 30, 2020 in an Indian student evacuated from Wuhan, and the first death was reported on March 12, 2020. , By August 2020, India had reported several million cases, with more cases among younger people than has been reported in higher-income countries. Deaths were concentrated in 50- to 64-year-olds.
India’s COVID-19 cases started to decline in September 2020, after peaking near 100,000 daily infections. After a plateau, cases began to rise again in March 2021, and the current peak is more than double the previous one, the severity of which has been described by comparison with the previous one, “the second wave has made the last one look like a ripple in a bathtub.” This surge has been attributed to a combination of factors, including the emergence of highly infectious SARS-CoV-2 variants (coronavirus variant B.1.617 was first detected in India in February 2021), a rise in unrestricted social interactions, and low vaccine coverage. In addition, inadequate resources and measures to combat the spread of COVID-19 have caused India to be considered the epicenter of the global COVID-19 pandemic. India now represents 50% of COVID-19 cases and 30% of deaths globally. From January 3, 2020 to May 21, 2021, there have been 26,031,991 confirmed cases of COVID-19 and 291,331 deaths in India.
Nepal
The surge in cases in India caused a critical upsurge in cases in Nepal, with which it shares a border. The cumulative cases in this country of 29 million are more than 513,000, with more than 6300 deaths as of May 23, 2021. The surging 9300 daily COVID-19 cases are overloading Nepal’s fragile health care system, and the country faces severe shortages of medical supplies and vaccines. Thus the pandemic easily crosses borders.
Russia
Russia is among the four countries with the highest number of confirmed COVID-19 cases as of May 11, 2020. The COVID-19 cases in Russia started later than in many neighboring European countries. Russia acted early to reduce importation of the virus by implementing quarantine for passengers arriving from China (January 23, 2020), closure of the land border with China (January 31, 2020), cancellation of most incoming flights from China (February 1, 2020), restrictions on the entrance of non-Russian citizens from China (February 4), and restrictions on access from Iran and South Korea in late February 2020. In the Russian Federation, from January 3, 2020 to May 21, 2021, there have been 4,983,845 confirmed cases of COVID-19, with 117,739 deaths, reported to the WHO.
Iran
Iran was among the first countries to experience large numbers of COVID-19 cases, but the rate of infection slowed after December 2020 32 as a result of containment measures such as movement restrictions and business closures across the country. After averaging 14,000 daily new cases, after December 1, 2020, the average daily new COVID-19 cases declined 50% to 6000 to 7000 and fatalities declined by approximately 50% and hospitalizations by 40%. Overall, the pandemic has caused 2,865,864 cases and claimed 79,219 lives in Iran.
Europe
France reported the first recognized case of COVID-19 in Europe on January 24, 2020, and within 6 weeks, all 27 countries of the European Union reported cases. Italy was the epicenter for cases early in the pandemic, reporting 62% of cases in Europe during the first week of March 2020. Italian cases and deaths were concentrated in the northern regions of Veneto and Lombardy during the latter part of February, likely as a result of environmental conditions there (see later section). On March 13, 2020, the WHO declared Europe the epicenter of the COVID-19 pandemic with more reported cases and deaths than the rest of the world combined. In a historic move, on March 17, 2020, the European Union closed all its external borders to prevent further spread of the virus. However, SARS-CoV-2 continued to spread quickly throughout the region, so that by the first week of April, Spain reported 21%, Italy 20%, Germany 15%, and France 11% of cases in Europe.
Differences across European countries can be attributed to a number of factors, including differences in population density, population size, the rapidity with which national governments imposed restrictions on movement of residents, availability of personal protective equipment (PPE) and sanitation supplies, and the restrictiveness of and adherence to stay-at-home and quarantine orders. Countries with fewer deaths locked down earlier, had shorter epidemics that peaked earlier, and had smaller populations.
Sweden, for example, stood out among European countries by not imposing restrictions on movement, masking requirements, or crowd sizes and instead relying on herd immunity to contain the epidemic. In addition, testing, contact tracing, source identification, and reporting were limited and considered inadequate. The effect was that Sweden’s cases and deaths (>1 million cases and >14,000 deaths) are higher than those of other Scandinavian countries (Norway 120,000 cases and 781 deaths; Finland 91,000 cases and 929 deaths ) as of May 21, 2021. The United Kingdom has experienced three waves of the pandemic and has reported 4.458 million cases and 127,710 deaths. The first nonclinical trial dose of the Pfizer/BioNTech COVID-19 vaccine was given December 8, 2020 in the United Kingdom, and vaccination began in earnest. Around the same time, a new variant of SARS-CoV-2, B.1.1.7, was beginning to spread, initiating the third surge of cases and the implementation of renewed travel and social distancing restrictions.
As of May 21, 2021, the European Union reported 51,599,270 cases and 1,093,462 deaths; the countries reporting the most deaths were France (5.568 million cases, 108,314 deaths), Italy (4.183 million cases, 125,028 deaths ), and Germany (3.64 million cases, 87,667 deaths ).
Americas
United States
The SARS-CoV-2 virus was introduced into the United States in January and February 2020 by travelers returning from China’s Hubei Province, where the virus was first recognized, and subsequently spread to their household contacts. No connection with international travel was found among cases by late February. Early in the pandemic, cases were concentrated on the East and West Coasts. Gatherings of persons from different locations, followed by return to their home communities, played a significant role in the early US spread of COVID-19. Over 3 weeks in late February to early March, the number of US COVID-19 cases increased more than 1000-fold. By mid-March, transmission had become widespread, and by April 21, a total of 793,669 confirmed COVID-19 cases had been reported in the United States, the majority resulting from widespread community transmission. Schuchat et al. report that four factors contributed to the speed with which the virus spread in the United States. Those factors include:
- 1.
Continued importation of the virus by travelers infected elsewhere (e.g., on cruise ships or in countries experiencing outbreaks). Restrictions on international travel did not occur until March 11, 2020, when the US President banned all travel from 26 European countries and declared a national emergency on March 13, 2020.
- 2.
Amplification of spread in local communities and across states occurred as a result of unrestricted attendance at professional and social events.
- 3.
Rapid spread occurred in facilities housing people in close proximity such as long-term care facilities and high-density urban areas, with the added importation to these areas by high levels of daily ingress and egress.
- 4.
Limited testing and contact tracing caused challenges in virus detection, concurrent circulation with influenza and influenza and pneumonia hospitalizations caused failure to recognize COVID-19 symptoms and infectivity, and cryptic transmission occurred from persons who were asymptomatic or presymptomatic.
During March 2020, national, state, and local governments, public health agencies, businesses, and schools began to implement mitigation strategies, issuing stay-at-home orders, virtual learning, organized case detection, contact tracing, and quarantine, but the response was uncoordinated and inconsistent. Thus different parts of the United States experienced varying levels of COVID-19 activity.
By June 9, 2020, New York State had the highest number of cases (>379,000) reported in the United States, with over half of these cases in New York City. At the same time, Washington state reported 24,354 cases and 1176 deaths and California was in a state of emergency, with 133,489 cases and 4697 deaths. By contrast, states in the Midwest reported lower cases and deaths at the same time: Kansas 10,972 cases and 238 deaths, Arkansas 10,327 cases and 172 deaths, and Wisconsin 21,308 cases and 661 deaths. Nationally, there were 1,933,560 reported cases with 110,220 deaths from COVID-19.
As the summer of 2020 began, PPE and sanitizing supplies became more widely available so that all people could access masks to prevent the spread of the virus. More information about how the virus spread was available, mass testing centers and testing protocols were in place, temporary intensive care units (ICUs) were opened in many hospitals, and more ventilators were becoming available. Despite promulgation through social media of ineffective and sometimes dangerous remedies for COVID-19, better treatments for COVID-19 cases were being developed and testing of vaccine candidates had begun. Although much of the United States had managed to flatten the curve, approximately 3 weeks after the Memorial Day holiday on May 30, 2020, cases began to surge again. This second wave of COVID-19 occurred in much of the United States because of lax adherence to social distancing protocols and family gatherings that included individuals from outside the household, the region, and state as the 7-day moving average doubled from 21,518 cases on June 1, 2020 to 43,767 cases on July 1, 2020.
After the summer wave, cases began to plateau through the fall when students stayed home from school and learned virtually, and most sports, entertainment, political gatherings, concerts, and other events that draw large groups of people continued to be curtailed. In addition, masking and social distancing had become commonplace and were being enforced in retail and other establishments.
In early winter, states that had seen little COVID-19 disease experienced surges. For example, Georgia on December 1, 2020 had 4261 new cases, which increased to 8371 new cases by December 31, 2020. During the second week of December (December 11) the Pfizer/BioNTech COVID-19 vaccine received EUA and was recommended by the Advisory Committee on Immunization Practices (ACIP) for individuals 16 years and older. A week later (December 18), the Moderna COVID-19 vaccines received EUA, and on December 19, 2020, the ACIP recommended its use in persons 18 years and older. Because of limited initial supplies, health care workers and residents of long-term care facilities were prioritized to receive the vaccine. Later, non–health care frontline essential workers and adults 75 years and older became eligible for vaccination; thereafter adults 65 years and older and younger adults ages 16 to 64 years with high-risk conditions became eligible. Initially, the rollout of vaccinations was slow and demand was high. At the end of February, a third vaccine (Janssen) became available and over the next several weeks, supplies and logistics for vaccinating large numbers of people were in place. Soon thereafter, children as young as 12 years of age were also given authorization by the regulatory agencies to be vaccinated. By May 20, 2021, 125,453,423 million Americans had received at least one dose of a COVID-19 vaccine. In response, COVID-19 cases began to decline, and restrictions on masking and social distancing were relaxed. Schools and businesses began to reopen, and capacity for indoor gatherings was increased in many places ( Fig. 1.3 ).
Canada
In Canada, the first few cases were reported on January 28, 2020, and the first death was reported on March 9, 2020. As of May 18, 2021, there have been roughly 1,338,141 reported cases and 25,018 deaths related to COVID-19 in Canada. The highest number of cases were seen in highly populated provinces, such as Ontario, with 513,102 confirmed cases and 8506 deaths, and Quebec, with 364,396 confirmed cases and 11,050 deaths. Ontario and Quebec reported the most cases (65.5%) and deaths (78.1%).
As observed in other developed countries, there was an increased risk of more severe outcomes for Canadians aged 65 and older with compromised immune systems or underlying medical conditions. However, Canada’s mitigation plan and considerable investment in research and development have led to dramatic successes in reducing the spread of COVID-19. These plans included significant cooperation among national and local governmental agencies with the preservation of local control over mitigation strategies to fit local circumstances and appropriate funding to support individuals, businesses, and local governments. Of the 13 jurisdictions reporting updates, no new deaths were reported in 6 provinces and territories in the previous 24 hours as of May 19, 2021, with 4.1% of the 33,754,111 tested identified as positive for COVID-19.
Mexico
The first case of COVID-19 detected in Mexico was on February 27, 2020. On April 30, 2020, 64 days after this first diagnosis, the number of patients had increased exponentially, reaching 19,224 confirmed cases and 1859 (9.67%) deaths. Cases of COVID-19 in Mexico were predominantly caused by community-based transmission, and the majority of cases of COVID-19 were located in Mexico City. Of 12,656 confirmed cases, most infected individuals were between the ages of 30 and 59 years (65.9%), with a mean age of 46 years. There was a higher incidence rate in men (58%) than in women (42%). Patients who died had one or more comorbidities, in particular, hypertension (46%), diabetes (39%), and obesity (30%). There have been 2,385,512 cases in Mexico and 220,746 deaths as of May 19, 2021.
Haiti
Among countries of the Western Hemisphere, Haiti has been spared the worst of the COVID-19 pandemic. With 13,906 cases and 288 deaths as of May 25, 2021, Haiti has one of the lowest death rates from COVID-19 in the world. This Caribbean nation often struggles with high rates of infectious diseases, yet has a COVID-19 death rate of 22 per million, compared with the United States at 1800 per million, and parts of Europe that are nearing 3000 per million.
Haiti’s success has not been attributed to innovative interventions or strict adherence to masking, social distancing, and quarantine. Rather, it is likely due to Haiti’s demographic distribution. Haiti is a young country, with an average age of 23 years. Although a significant number of people were infected by the virus in the summer of 2020, most showed no symptoms. In fact, Haiti closed its COVID-19 units in the fall of 2020 because of a lack of patients. According to Dr. Jacqueline Gautier, Director of the St. Damien Pediatric Hospital, “COVID-19 hasn’t become a daily concern for most Haitians.” A surge such as that seen in India may occur in Haiti given the capricious nature of the disease and the fact that Haiti has refused COVID-19 vaccines supplied through the COVAX program.
Latin America
Nearly 6 weeks after the first reported cases in the United States (March 10, 2020), Panama became the second country in Latin America and the first Central American country to have a confirmed coronavirus-related death, in an individual who had traveled to Spain and returned infected. On March 11, 2020, Honduras reported its first two cases of COVID-19 involving two women who had traveled to Europe.
According to the Pan American Health Organization, three factors accounted for most of the spread of COVID-19 into and within the Americas: importation, community transmission, and outbreaks in enclosed areas such as nursing homes. Brazil has had the highest number of confirmed cases (15,812,055) with 441,691 deaths as of May 21, 2021. , São Paulo is the largest city in South America and receives the greatest proportion of international flights in Brazil. Cities in Brazil are densely populated, with large numbers of poor people, indigenous people, and people living in close quarters. Cases and deaths were relatively low in Brazil until its first peak began in June 2020, with a second surge that began in January 2021. In an editorial published in May 2021, Hallal and Victoria argue that Brazil’s current devastating COVID-19 crisis in which Brazil accounts for 12% of all COVID-19 cases and more than a quarter of deaths, despite having 2.7% of the world’s population, is due to several factors. They include denial of science and consequent failure to implement social distancing, lockdowns, masking, and other mitigation strategies; denial of the value of vaccines and consequent failure to procure vaccines, especially those with the highest efficacy; and the practice of sending infected patients, particularly those infected with the new P.1 variant, to hospitals in other cities in because of overcrowded conditions in the area where patients live, contributing to the spread of more highly transmissible infections.
In the last few weeks of May 2021, Argentina had reported record-breaking numbers of daily cases (39,000/day up from 5000/day in March 2021) and deaths (744/day up from 112/day in March 2021). More than 3.5 million cases and more than 74,000 deaths were reported as of May 23, 2021. In response, the government of Argentina has implemented strict containment measures, including closing schools and nonessential businesses and banning social, religious, and sporting events until the end of May 2021. Argentina has the second highest COVID-19 burden, with 3,191,097 cases and 68,311 deaths; followed by Colombia with 3,031,726 cases and 78,771 deaths; Peru with 1,897,000 cases and 66,770 deaths; Panama with 368,368 cases and 6282 deaths; Honduras with 222,228 cases and 5789 deaths; and Costa Rica with 273,714 cases and 3456 deaths as of May 12, 2021. In total, there were more than 21,390,349 cases of COVID-19 reported in South America as of May 18, 2021.
Africa
The African continent was the last and least affected by the COVID-19 pandemic to date. The African continent confirmed its first case of COVID-19 in Egypt on February 14, 2020. In sub-Saharan Africa, the first case was reported in Nigeria on February 27, 2020. , Most of the initial cases of COVID-19 in Africa were imported from Europe and the United States rather than from the original COVID-19 epicenter, China. Africa’s first wave of the pandemic peaked in July 2020, when the mean daily number of new cases was 18,273.
Reporting for African countries in five regional groupings indicates Central (9 countries, 121.2 thousand cases, 2000 deaths); Western (15 countries, 444.3 thousand cases, 5600 deaths); Eastern (14 countries, 6.8 million tests, 468.5 thousand cases, 8500 deaths), Northern (7 countries, 1.2 million cases, 35,200 deaths); and Southern (10 countries, 1.9 million cases, 59,300 deaths). The most-affected countries are South Africa (1,538,961 cases, 3.4% mortality) and Egypt (52,251 cases, 7.2% mortality).
As of December 31, 2020, 40 African countries had experienced or were experiencing a more severe second wave of the pandemic, with the continent reporting a mean of 23,790 daily new cases. As of May 19, 2021, there were 2,763,421 COVID-19 cases and 65,602 deaths, accounting for 3.4% of worldwide cases and 3.6% of deaths and surpassing those figures from the early months of the global pandemic. This wave was in part due to new virus variants that emerged in South Africa. Since peaking in mid-January 2021, overall cases and deaths have trended downward; however, countries throughout the African region continue to report sustained transmission and increases in some areas, highlighting the importance of examining multiple epidemiological variables at the regional and country levels over time. As of May 2, 2021, the African region reported over 42,000 new cases, a 15% decrease, and 1000 new deaths, a 13% decrease compared with the previous week. The highest numbers of new cases were reported from South Africa (3% decrease), Ethiopia (34% decrease), and Cameroon (8% increase). The highest numbers of new deaths were reported from South Africa (32% decrease), Ethiopia (12% decrease), and Kenya (1% increase).
Several factors have significantly affected the epidemiology of COVID-19 in the African continent, , including (1) late arrival of the pandemic; (2) weak diagnostics, such as inadequate COVID-19 testing (as of December 31, 2020, 17 countries reported test-to-case ratios less than the recommended 10–30:1); (3) lack of essential medical supplies; and (4) a largely susceptible population (18 countries reported CFRs greater than the global CFR of 2.2%). The true epidemiology of COVID-19 in the African continent and the actual number of cases remain unknown because of inadequate testing capacity. Furthermore, 48 countries had five or more stringent public health and social measures in place by April 15, 2020; this number had decreased to 36 as of December 31, 2020, despite an increase in cases in the preceding month.
Cases and mortality in Africa are likely to be affected by the presence of other diseases. The Infectious Disease Vulnerability Index (IDVI, 2016) pointed out that of 25 countries most vulnerable to infectious diseases, 22 are in the African region. The WHO Africa estimates that 26 million people infected with human immunodeficiency virus (HIV), 2.5 million with tuberculosis, 71 million with hepatitis B or C, and 213 million with malaria live in Africa. Moreover, noncommunicable diseases, such as cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes, that affect the ability to fight infectious diseases increase the burden of COVID-19 in Africa. ,
Oceania
Australia
The first case of novel coronavirus in Australia (nCoV-19) was reported in Victoria on January 25, 2020, with an additional three cases confirmed in New South Wales later that day. A total of 12 cases of nCoV-19 infection were notified up until February 1, 2020. All 12 cases reported a travel history to China, especially to Wuhan, Hubei Province. On March 16, 2020, the Australian Ministry of Health declared a public health emergency.
Mitigation measures were imposed by the third week of March 2020 that included (1) a ban on nonessential indoor gatherings of 100 people or more, (2) considering only essential travel, (3) strict visitor rules for aged care facilities, (4) social distancing of 1.5 m, and (5) allowing student nurses to work in situations that assisted with pandemic response. By March 24, 2020, Tasmania, Northern Territory, South Australia, Western Australia, and Queensland announced closed borders and travel restrictions. In addition, by the end of March 2020, South Australia, Western Australia, New South Wales, Tasmania, Northern Territory, Australian Capital Territory, Victoria, and Queensland had all announced, cumulatively, billions of dollars’ worth of economic stimulus and support packages.
Australia continues to report low numbers of COVID-19 cases; in the 2 weeks reporting from April 26 to May 9, 2021, the daily average number of cases was 12. As of May 23, 2021, the total number of cases was 30,011, with 910 deaths reported. Reported cases have been higher among males than females in all age groups older than 30 years.
New Zealand
New Zealand’s rapid and immediate response to the COVID-19 pandemic has resulted in extremely low rates of infection and death. Working together with local public health officials, the New Zealand government invested a considerable amount of money in a “go hard, go early” strategy to combat the spread of the virus. Prevention policies were implemented by local infectious disease experts that were individually applied to each clinic or hospital department, with an emphasis on coordination and communication. The “hard-and-early” strategy was effective because New Zealand adopted a set of nonpharmaceutical interventions to stop the spread of COVID-19 and governments supplied resources such as personnel, PPE, laboratory supplies, etc. as they were requested. As other high-income countries have reported an increasing number of cases since August, 2020, New Zealand is one of the few countries globally with low COVID-19 cases and deaths, reporting 2313 confirmed cases with 29 deaths since March 2020.
Australia’s and New Zealand’s successes prove that a robust public health response focused on vigilant testing, well-functioning surveillance systems, and strict adherence to quarantine that are both enforced and supported by government, are the key to fighting a pandemic. ,
Risk Factors for COVID-19
As the pandemic swept across the world, the general public, public health officials, and governmental agencies watched in trepidation as SARS-CoV-2 arrived in each locality and cases began to surge. Tracking of cases was initiated to elucidate the population subgroups at greatest risk for infection, severe disease, and death. Many of the epidemiological studies were based on population-level factors and data. These studies were meant to inform systems to prepare for a surge in cases and allocate resources to the areas of greatest need. In the United States and elsewhere, PPE and sanitation supplies were in short supply and government officials were initially reluctant to impose sheltering in place orders and other restrictions on people’s movement. All of these factors contributed to unequal risk from a virus to which the entire population was naïve and should have been equally vulnerable.
In December, 2020, Woolf et al. published an editorial declaring COVID-19 as the leading cause of death in the United States, surpassing both heart disease and malignant neoplasms. This conclusion was based on COVID-19 deaths through October 2020, before the predicted 2020–2021 winter surge, which ultimately occurred, surpassing even the first spring 2020 surge. Provisional mortality data for 2020 named COVID-19 the third leading cause of death, with an overall 15.9% increase in age-adjusted mortality.
Early reports of risk factors for severe disease and death were older age, male sex, and presence of one or more chronic diseases, including diabetes, obesity, cardiovascular disease, and chronic lung disease. Other chapters are devoted to the relationships of COVID-19 and these chronic diseases.
Sex
Differences in COVID susceptibility and mortality between males and females have been noted. Early reports from China suggested higher rates of COVID-19 cases among males (1.27:1 male-to-female ratio), as well as COVID-19 deaths. Studies from Korea and the United States showed higher numbers of cases among females, whereas other studies showed no sex-based differences. Studies in the United States reported higher odds of severe outcomes and mortality associated with male sex. , These findings were later confirmed in which males were more frequently hospitalized, admitted to the ICU, intubated, and prescribed vasopressors. These varied findings may be due to differences in sample sizes, inclusion criteria, and methodology. Large studies, including data from multiple countries have confirmed that there are male and female differences in both COVID-19 cases and deaths. Importantly, sex-based differences in COVID-19 cases are age dependent, with confirmed cases higher among females in younger ages (10–50 years) and among males at ages younger than 10 and older than 50 years. On the other hand, case fatality rates for COVID-19 across 38 countries were significantly higher for males (7.3; 95% CI, 5.4–9.2) compared with females (4.4; 95% CI, 3.4–5.5; P < .001). Moreover, the risk for death for males increases with increasing age. Among nursing home patients, risk for mortality was significantly higher for males than females.
Many reasons, both biological and nonbiological, have been posited to explain these differences. For example, females have been shown to have stronger cell-mediated and humoral immune responses to viral and other microbial infections. , These differences are thought to be related to the sex hormone milieu―estrogen is immune enhancing and testosterone is immune suppressive. , Fig. 1.4 illustrates the potential role of hormonal and humoral factors proposed for the observed sex-based differences in susceptibility to SARS-CoV-2. Additionally, females have longer life expectancy and lower mortality from coronary heart disease and other chronic diseases, all of which are related to COVID-19 mortality. Some have attributed sex differences in COVID-19 mortality to social differences such as the higher frequency of male smokers, less health care–seeking behavior among males, and higher exposure to environmental toxins among males, because more females stay home to care for children (see Fig. 1.4 ).