Key points
- •
Regional perfusion is a method of delivering high-dose chemotherapy to a region burdened with cancer.
- •
Isolated limb perfusion and hepatic perfusion are traditional open surgical methods of regional therapy in treating melanoma confined to an extremity or the liver.
- •
Newer hybrid methods employ percutaneous techniques by interventional radiologists to gain access to the afferent and efferent blood flow of the limb or liver.
Introduction
Regional perfusion is a unique approach to treating cancer confined to a region or organ of the body. This includes procedures that attempt to deliver effective levels of chemotherapy to an area of the body that bears a malignancy.
The afferent and efferent blood supply of a region or organ is placed on a heart-lung bypass circuit in regional perfusion. The blood flow to this organ or region is then independent of the systemic circulation, so that the blood flow within the region or organ is “isolated.” A high dose of chemotherapeutic agent is circulated through the isolated segment to treat the cancer while sparing the rest of the body from exposure to the agent. This increases the amount of chemotherapy delivered to the cancer cells, potentially to a range where the agent is more active while minimizing systemic toxicity from the treatment.
Two prototypic regional perfusion techniques are used to treat either cancers confined to the extremities or the liver. For each technique, the initially developed complex open operative procedure has evolved to a minimally invasive approach requiring the skills of multiple specialties. Classically, regional treatment of the extremities uses an open surgical procedure called an isolated limb perfusion (ILP). This procedure has evolved into a minimally invasive approach known as an isolated limb infusion. Similarly, regional treatment of hepatic cancers has evolved from an operation called an isolated hepatic perfusion to hepatic chemosaturation (formerly known as percutaneous hepatic perfusion or extracorporeal chemofiltration).
In each case, a complex open operative procedure has progressed into a hybrid procedure combining elements of image guidance done by interventional radiologists with intraoperative chemotherapy. This is best accomplished with a multidisciplinary approach combining the abilities of interventional radiologists, surgical oncologists, and anesthesiologists. For regional perfusion of the limb or liver, the hybrid procedure has not supplanted the open approach but rather provides an alternative to complex procedures with their own advantages and challenges.
Rationale for regional treatment
There are theoretic advantages of regional perfusion strategies that include the following:
- 1.
Minimizing systemic exposure and toxicity from the chemotherapeutic agent. By separating the blood flow to the organ or region of interest, chemotherapy can be intentionally delivered to the tumor-bearing area. Systemic exposure to the chemotherapeutic agent is limited to that amount that leaks into the systemic circulation. With no leak, the only toxicity is confined to the treated organ or region.
- 2.
Chemotherapeutic agents are delivered to the tumor-bearing area at a more effective dose. The therapeutic index is the dose that causes toxicity in 50% of recipient patients divided by the dose that causes regression of tumor in 50% of those treated. For many chemotherapeutic agents, the latter dose is higher than the former so that the therapeutic index is <1. The dose can be escalated if exposure is limited to an organ or region that does not experience significant toxicity from the agent. This brings the therapeutic index to a level significantly greater than 1, resulting in increased efficacy.
- 3.
The entire tumor-burdened organ or region is treated. This is in contrast to local resection, ablation, or selective embolization procedures. In some instances, a single lesion or oligometastatic disease may be effectively controlled with resection, ablation, or selective embolization. But regional perfusion can encompass a larger distribution and/or volume of tumor burden.
Candidate cancers for regional perfusion
Regional perfusions, theoretically, are most applicable for cancers in which the disease is isolated to an upper extremity, a lower extremity, or the liver. Eradication of the cancer in these cases may result in prolonged disease-free survival. This usually includes a very narrow spectrum of clinical scenarios. By definition, only disease that is in the region of interest is treated by high-dose chemotherapy. But cancers are rarely confined to a region. Most cancers are confined locally to the primary site, metastatic to the regional lymph nodes, or systemically disseminated through hematogenous spread.
There are examples, however, where a regional approach makes sense. In the limb, advanced primary tumors or tumors with lymphatic spread may be susceptible to this approach. In the liver, advanced primaries or metastatic disease isolated to the liver, but not amenable to resection, may be candidates for regional perfusion.
In practice, only melanoma (cutaneous for limb regional perfusion, ocular for hepatic regional perfusion) has been adequately clinically investigated for this approach using single agent melphalan or melphalan-based combination therapies. Regional therapy to the limb or liver for other types of cancer should be considered investigational and completed on a research protocol.
When considering the range of cancers that can be treated with a regional perfusion, it is important to recognize that regional perfusion is a method of chemotherapy delivery and therefore the range of response is similar to systemic chemotherapy. It is not equivalent to ablative therapies like alcohol injection, radiofrequency ablation, or high-frequency focused ultrasound. If systemic chemotherapy kills one type of cancer, it cannot be expected to be equally efficacious if used for a completely different type of cancer, whereas ablative therapies may be used interchangeably against differing histologies.
Responses are dependent on the specific tumor’s susceptibility to the chemotherapy used.
In-transit metastases from cutaneous melanoma
Melanoma often has its primary lesion in the upper or lower extremity and initially treated by wide excision and staging of the regional nodal basin. In a small subset of patients, melanoma will recur as metastases within the lymphatic channels of the limb, either in a dermal or subcutaneous location. These can occur with or without nodal involvement, and without evidence of hematogenous distant spread. This disease pattern is referred to as satellite or in-transit metastases depending on the distance from the primary site (satellite lesions occur within 5 cm of the excised primary). Metastatic lesions can occur between the primary and draining lymph node bed, or on the limb, distal to the primary lesion as so-called retrograde in-transit lesions.
In-transit disease is an infrequent yet clinically significant pattern of spread from a primary melanoma. Between 1991 and 2001, a total of 1395 patients at the M.D. Anderson Cancer Center had their primary lesion treated with wide local excision and sentinel lymph node biopsy to assess the regional lymph node basin. Ninety-one patients, or 6.9%, subsequently developed in-transit melanoma. Similar trials show an incidence of in-transit disease of 3.5%–8%. The development of in-transit metastases portends a poor survival. In-transit metastases without lymph node metastases assigns the patient to American Joint Committee on Cancer (AJCC) stage 3A with a median survival approximating 5.5 years, and with nodal disease places the patient in stage 3C with median survival approximating 2.0 years.
Although in-transit metastases can be excised, they often represent disseminated disease throughout the limb lymphatics. In rare instances, the limb can be surgically sterilized of disease through one or multiple operations leading to long-term cure. The most aggressive form of local control is amputation and can result in a 5- and 10-year survival rate of 40% and 20%, respectively. Because systemic therapy provides only a modest objective response rate, more effective strategies of delivering chemotherapy such as regional treatment of the upper or lower extremity are adopted in an attempt to render these patients free of disease without the need for amputation.
Ocular melanoma and cancers for percutaneous hepatic perfusion
Ocular melanoma represents an example of a cancer with a natural history favorable for regional treatment. Uveal melanomas develop in the vascular layer of the orbit, including the iris, ciliary body, and choroid. Although the primary lesion is in the eye, metastatic spread tends to be to the liver. In the collaborative ocular melanoma study, 361 of 1003 subjects with large uveal melanomas developed metastatic disease and of these 93% had hepatic metastasis. Many patients die of hepatic failure from hepatic replacement with metastasis, in the absence of other disease. Regional treatment, therefore, has the potential to halt the life-threatening component of the metastatic disease.
Cancers metastatic to the liver or advanced primary hepatic cancers are likely to be susceptible to isolated hepatic perfusion or chemosaturation; however, current studies for these cancers are inadequate for perfusion to be a standard approach.
Gastrointestinal cancers that spread through the portal system to the liver have a natural history that is unique compared to other metastases from hematogenous spread. Patients with limited colon cancer metastases in the liver exemplify this point. When the disease is isolated to the liver, with minimal and anatomically favorable location, resection is often used to eliminate the metastasis. In selected patients treated with resection, 41% remain alive at 5 years following resection. This suggests that colon cancer may spread hematogenously to the liver, but that hematogenous spread does not continue systemically in all cases.
Other cancers with portal spread may also be limited to hepatic metastases. Therefore liver-directed therapies are often used when metastatic disease exceeds the limits for resection. The role of regional perfusion therapy—either isolated hepatic perfusion or chemosaturation with percutaneous hepatic perfusion—for these histologies is yet to be defined and treatment of these cancers remains experimental.
Isolated limb perfusion
The procedure
ILP, an operative technique for regional therapy delivered to a specific limb ( Figure 3-1 ), is used to treat in-transit melanoma limited to either a lower extremity or an upper extremity. High-dose melphalan can be infused into the diseased limb with minimal systemic exposure to the chemotherapy, similar to other regional perfusions.
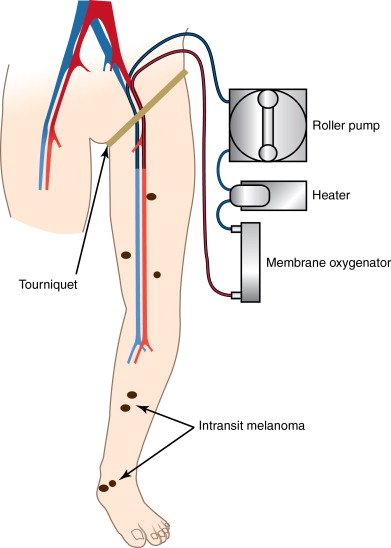
The regional artery and veins can be approached at several sites along the vessel depending on the distribution of disease in the limb. Vascular surgical principles for anticoagulation and vessel repair are applicable and must be followed as in any other vascular procedure.
In the lower extremity, cannulation can occur at the external iliac vessels, the superficial femoral vessels, or the popliteal artery and vein. The iliac approach is useful for disease that extends up to the groin crease, or when iliac nodes are involved. The external iliac vessels are approached through a retroperitoneal incision, and a deep dissection is completed at the time of cannulation. This allows for the dissection of any deep lymph nodes with metastatic involvement at the time of perfusion. For disease in the distal one-third of the thigh and below, or when inguinofemoral lymph nodes are involved, the superficial femoral vessels can be cannulated. A superficial lymph node dissection is completed first and then the vessels are cannulated entering at the level of the common femoral vessels. For the iliac and superficial femoral approaches, the cannula must be advanced below the tourniquet. The popliteal vessels can be used for disease that is limited to a level below the knee ( Figures 3-2 and 3-3 ). These are approached superiorly through the Hunter canal. The pneumatic cuff is inflated at a level above the incision ( Figure 3-4 ).



In the upper extremity, vascular access can occur at the subclavian vessels through an infraclavicular approach or at the axillary vessels through an axillary incision. The cannula must be advanced to a level below the tourniquet for each approach.
All collateral vessels are surgically ligated for procedures where cannulation is above the tourniquet. This is especially important for an iliac approach. This is to prevent any leak of perfusate out of the limb into the systemic circulation, and conversely to prevent leak of systemic circulation into the limb.
After cannulation and application of a tourniquet, the limb circulation is placed completely on a heart–lung bypass circuit. In this circuit, the blood is circulated using a roller pump, heated using an external bath, and blood gas is maintained using a membrane oxygenator. Hyperthermia is established both by heating the perfusate and external warming of the limb. Chemotherapeutics are added to the circuit and circulated through the limb for a period of 60 minutes.
Leak is minimal with a pneumatic cuff used on the thigh. But in many patients, the disease extends high on the thigh, mandating iliac cannulation and a manual tourniquet at the groin crease; leak may occur across this tourniquet, exposing the patient to potentially toxic levels of chemotherapy. In addition, the systemic circulation can leak into the limb, increasing the blood loss when the limb blood is discarded at the conclusion of the case. Leak can be managed by tightening the tourniquet, and adjusting the flow into the limb. The arterial pressure in the limb is constant, not pulsatile because of the use of roller pumps. Increasing the blood pressure to above the systemic mean can minimize leak into the limb. Further, decreasing the flow, and thereby the limb blood pressure to below the mean arterial blood pressure, leak from the limb into the systemic circulation can be decreased.
Monitoring leak is important when a manual tourniquet is used. Several methods have been used to monitor leak, but the use of radioactive labeled autologous blood is most widely accepted. Separate aliquots of blood are labeled with 99 technetium; one with a defined dose, usually approximating 3.0 mCi, and one with 1/10th the dose, usually 0.3 mCi. A gamma-counter is placed over the heart to measure the level of radioactivity in the systemic circulation. After the limb circuit is established and the tourniquet inflated, the 0.3 mCi aliquot of blood is given systemically. The resulting increase in gamma counts/min over baseline establishes the change associated with a 10% leak. Then the 3.0 mCi aliquot is given in the limb circuit. Any leak can be measured by the gamma counter using the 10% leak as a standard. For melphalan, the dose used in limb perfusion tends to be 10 times the dose that could be given systemically, so greater than 10% leak can be extremely toxic to the bone marrow.
Clinical results
The Sydney Melanoma Unit studied 101 patients with melanoma of the extremity who were treated with ILP using melphalan and dactinomycin. Of the 87 patients available for evaluation, there was a 90.8% overall response rate, with 58 patients exhibiting a complete response. The median local recurrence-free interval after complete response was 21 months, with 32 patients eventually developing distant disease. Long-term follow-up of 120 patients from Sydney who underwent ILP between 1984 and 1997 revealed that after an initial complete remission (CR) rate of 69.2%, there was a sustained CR rate of 33.7% (median follow-up of 199 months; 8–226 months). The response rate increased to 56.6% when patients who underwent minor resection of recurrent or residual disease were included. Several groups have confirmed a high response rate to melphalan-based ILP for regional melanoma ( Table 3-1 ).
| Group | N | Agents | Objective response | Survival | Toxicity |
|---|---|---|---|---|---|
| University of Erlangen 2006 | 101 | Melphalan Dactinomycin | 90.8% (CR = 66%) | Median PFS: 21 mos. | Grades IV and V: 5% |
| Netherlands Cancer Institute, 2002 | 202 | Melphalan | CR = 56.1% (>75 years old) CR = 58.2% (<75 years old) | 5-year survival: 37.0–40.6% | Grades III and IV 20.8%–23.7% |
| Tulane University, 1996 | 468 | Melphalan +/− Thiotepa +/− Dactinomycin | 5-year survival: 21% |
In an effort to improve response rates and disease-free duration, several groups combined tumor necrosis factor (TNF) with melphalan in ILP ( Table 3-2 ). In a single-arm trial, Leinard and associates in the Netherlands tested the combination of melphalan/TNF-α and interferon-γ delivered by ILP to patients with limb-restricted malignances including melanoma. Patients with melanoma showed a high response rate (overall response 100%, CR 90%) for in-transit disease. Similarly, the NCI conducted a dose escalation trial of melphalan, TNF-α, and interferon-γ in 38 patients with biopsy-proven in-transit or satellite melanoma. Response rates were high, with a CR rate of 76% for the low TNF-α group (4 mg) and 36% for the high TNF-α group (6 mg). In a subsequent multicenter phase II study run by the Dutch group, 64 patients with locally recurrent melanoma were randomized to receive melphalan/TNF-α with or without interferon. The objective response rate was 91%–100% for the two groups.
| Group | Agent(s) | N | Overall Response (%) | CR (%) |
|---|---|---|---|---|
| Lienard, 1992 | Melphalan/interferon-γ/TNF-α | 29 | 29 (100) | 26 (90) |
| Vaglini, 1994 | Melphalan/interferon-γ/TNF-α | 11 | 7 (64) | 7 (64) |
| National Cancer Institute, 1996 | Melphalan/interferon-γ/4 mg TNF-α Melphalan/interferon-γ/6 mg TNF-α | 26 11 | 24 (92) 11 (100) | 20 (76) 4 (36) |
| University of Pennsylvania 1999 | Melphalan Melphalan/interferon-γ/TNF-α | 51 52 | 49 (96) 47 (91) | 30 (58) 37 (72) |
| Lienard, 1999 | Melphalan/interferon-γ Melphalan/interferon-γ/TNF-α | 33 31 | 30 (91) 31 (100) | 23 (69) 24 (78) |
| ACOSOG, 2006 | Melphalan Melphalan/interferon-γ/TNF-α | 58 58 | 36 (62) 40 (69) | 14 (25) 15 (26) |
A small multiinstitutional trial enrolled 103 patients with measurable in-transit lesions randomized to ILP with melphalan or melphalan/TNF-α/ interferon-γ. There were more CRs in the group receiving TNF-α (72% vs. 58%) with no statistical differences in overall response (81% vs. 96% respectively) or survival (disease-free survival 12 vs. 14 months, respectively, and 3-year survival 58% for both groups).
The cumulative results of these studies led to cooperative group randomized multicenter trial comparing ILP with melphalan only or melphalan + TNF-α (ACSOG Z0020). One hundred twenty-four patients with locally advanced extremity melanoma were enrolled and underwent treatment. Accrual was halted early when investigators found no difference in response rates between the treatment groups. Analysis did show a slight improvement in the durability of the CR in the TNF-α group, though this was not a study end point. Many criticize this study for nonstandardization of the assessment of tumor response and the short duration of follow-up in the CR assessment. The response rates for this trial are dramatically lower than previous trials (see Table 3-4 ). In addition, the early cessation of this trial meant that a subgroup analysis on patients with bulky disease could not be completed. Many suggest that bulky disease appears to respond more rapidly and more frequently with the TNF-α combination.
Generally, overall objective response rates of 80%–90% with complete response rates of 50%–60% should be expected from melphalan-based ILP. These response rates, unfortunately, are rarely durable, with a median time to progression reported of 9–24 months. Long-term follow-up from the National Cancer Institute shows 5-year recurrence-free survival (in the field and out of the field) to be 18.0%. Similarly, investigators from Australia report that at a median follow-up of 177 months, 18.5% of 108 patients are alive without disease. Survival data are difficult to interpret though, because perfusion is applied to patients with various stages of disease and survival after perfusion stratifies by stage. , Series with a large proportion of early-stage disease will therefore show a prolonged survival for the study group that may not be reflective of survival in the whole population of patients typically treated with ILP.
Toxicity from melphalan-based ILP includes specific toxicity to the limb, as well as delayed effects from system exposure to melphalan. Limb toxicity is defined by the Wieberdink classification ( Table 3-3 ). Toxicity is dependent to some degree on the conditions of ILP. When hyperthermia is used, increased regional toxicity is measured at higher temperatures. Temperatures exceeding 42°C degrees results in high toxicity. Additionally, systemic complications are dependent on systemic exposure to the drug.