- To understand how to best meet the nutritional needs of an individual, the distinction between physiology in health and pathophysiology in disease needs to be carefully considered.
- For some groups of patients, the requirements are higher than those in health, while for other groups of patients they are lower. If recommendations for healthy individuals are applied to patients with certain types of disease, they may produce harm.
- In health, only the oral route is used to provide nutrients to the body. In clinical practice, other routes can be used. The use of the intravenous route for feeding raises a number of new issues.
- Alterations in nutritional therapy during the course of an acute disease may occur because the underlying disease has produced new complications or because it has resolved. Similarly, in more chronic conditions there is a need to review the diet at regular intervals.
1.1 Introduction
Clinical nutrition focuses on the nutritional management of individual patients or groups of patients with established disease, in contrast to public health nutrition, which focuses on health promotion and disease prevention in the general population. The two disciplines overlap, however, especially in older people, who are often affected by a range of disabilities or diseases. Working together, instead of independently, the two disciplines are more likely to facilitate successful implementation of local, national, and international policies on nutrition. To understand the overlap between them, it is necessary to consider not only some of the principles of nutrition that apply to health, but also special issues that apply to the field of clinical nutrition. These include altered nutritional requirements associated with disease, disease severity and malnutrition, and nonphysiological routes of feeding using unusual feeds and feeding schedules. This introductory chapter provides a short overview of these issues, partly because they delineate qualitative or quantitative differences between health and disease, and partly because they form a thread that links subsequent sections of this book, which is divided into discrete chapters addressing specific conditions.
It is now possible to feed all types of patients over extended periods of time, including those who are unconscious, unable to eat or swallow, or have little or no functional gastrointestinal tract. It is possible to target specific patient groups with special formulations, and even to change the formulation in the same patient as nutritional demands alter during the course of an illness. Since some of these formulations may be beneficial to some patient groups and detrimental to other groups or to healthy subjects, the distinction between physiology in health and pathophysiology in disease needs to be considered carefully. It is hoped that some of the principles outlined here will help to establish a conceptual framework for considering some of the apparently diverse conditions discussed in this textbook.
1.2 The spectrum of nutritional problems
Clinical nutrition aims to treat and prevent suffering from malnutrition. However, there is no universally accepted definition for ‘malnutrition’ (literally, ‘bad nutrition’). The following definition, which encompasses both under- and over-nutrition, is offered for the purposes of this chapter.
Malnutrition is a state of nutrition in which a deficiency or excess (or imbalance) of energy, protein, and other nutrients causes measurable adverse effects on tissue/body function (shape, size, and composition) and clinical outcome.
In this chapter and elsewhere, however, the term ‘malnutrition’ is mainly used to refer to under- rather than over-nutrition.
Both under- and over-nutrition have adverse physiological and clinical effects. Those relating to under-nutrition (Table 1.1) are diverse, which explains why malnourished patients may present to a wide range of medical disciplines. Several manifestations may occur simultaneously in the same individual, although some predominate. They may be caused by multiple deficiencies. Specific nutrient deficiencies may also have diverse effects, affecting multiple systems, but it is not entirely clear why the same deficiency can present in a certain way in one subject and a different way in another. For example, it is not clear why some patients with deficiency of vitamin B12 present to the haematologist with megaloblastic anaemia, others to the neurologist with neuropathy and other neurological manifestations (e.g. subacute combined degeneration of the cord), and still others to the geriatrician with cognitive impairment or dementia.
Table 1.1 Physical and psychosocial effects of under-nutrition.
| Adverse effect | Consequence | |
| Physical | ||
| Impaired immune responses | Predisposes to infection | |
| Reduced muscle strength and fatigue | Inactivity, inability to work effectively, and poor self-care. Abnormal muscle (or neuromuscular) function may also predispose to falls or other accidents | |
| Reduced respiratory muscle strength | Poor cough pressure, predisposing to and delaying recovery from chest infection | |
| Inactivity, especially in bed-bound patient | Predisposes to pressure, sores, and thromboembolism | |
| Impaired thermoregulation | Hypothermia, especially in the elderly | |
| Impaired wound-healing | Failure of fistulae to close, un-united fractures, increased risk of wound infection resulting in prolonged recovery from illness, increased length of hospital stay, and delayed return to work | |
| Foetal and infant programming | Predisposes to common chronic diseases, such as cardiovascular disease, stroke, and diabetes in adult life | |
| Growth failure | Stunting, delayed sexual development, and reduced muscle mass and strength | |
| Psychosocial | ||
| Impaired psychosocial function | Even when uncomplicated by disease, undernutrition causes apathy, depression, self-neglect, hypochondriasis, loss of libido, and deterioration in social interactions. It also affects personality and impairs mother–child bonding | |
The spectrum of presentations is more diverse than this would indicate because protein–energy malnutrition frequently coexists with various nutrient deficiencies. For example, patients with gastrointestinal problems are frequently underweight and at the same time exhibit magnesium, sodium, potassium, and zinc deficiencies, due to excessive losses of these nutrients in diarrhoea or other gastrointestinal effluents. There may also be problems with absorption; for example, patients with Crohn’s disease affecting the terminal ileum, where vitamin B12 is absorbed, are at increased risk of developing B12 deficiency. Patients who have had surgical removal of their terminal ileum or stomach, which produces the intrinsic factor necessary for B12 absorption, fail to absorb vitamin B12. Isolated nutrient deficiencies may also occur, for example iron deficiency due to heavy periods in otherwise healthy women.
Another complexity is the interaction between nutrients, which may occur at the level of absorption, metabolism within the body, or excretion. One nutrient may facilitate the absorption of another; for example, glucose enhances the absorption of sodium (on the glucose–sodium co-transporter). This is the main reason why oral rehydration solutions used to correct salt deficiency due to diarrhoea (or fluid losses due to other gastrointestinal diseases) contain both salt and glucose. In contrast, other nutrients compete with each other for absorption. For example, because of competition between zinc and copper for intestinal absorption, administration of copper may precipitate zinc deficiency, especially in those with borderline zinc status. Other nutrients interact with each other during tissue deposition. Accretion of lean tissue requires multiple nutrients, and lack of one of them, such as potassium or phosphate, can limit its deposition, even when adequate amounts of protein and energy are available (Figure 1.1). This emphasises the need to provide all necessary nutrients in appropriate amounts and proportions.
Figure 1.1 Effect of omitting potassium (K) and phosphate (P) from a parenteral nutrition regimen on the nitrogen (N) balance of depleted patients receiving hypercaloric feeding. Data from Rudman et al. (1975).

1.3 Nutritional requirements
Effect of disease and nutritional status
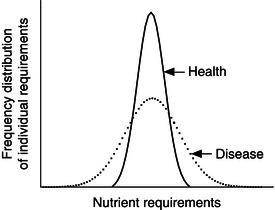
Fluid and electrolytes
The principles of nutrient requirements in healthy individuals are described in Introduction to Human Nutrition (Gibney et al., 2009), an earlier volume in this textbook series. The average nutrient intake refers to the average intake necessary to maintain nutrient balance. The reference nutrient intake (RNI) refers to the intake necessary to satisfy the requirements of 97.5% of the healthy population (+2 standard deviations from the average nutrient intake). In patients with a variety of diseases, the requirements are more variable (Figure 1.2): for some groups of patients, they are higher than for those in health, while for other groups they are lower. For example, in patients with gastrointestinal fluid losses, the requirement for sodium may be double the RNI, while in patients with severe renal or liver disease who retain salt and water, the requirements may be well below the average nutrient requirement for healthy subjects ingesting an oral diet. The requirements for potassium and phosphate may also be well below the RNI for patients with severe renal disease in whom there is failure of excretion. Therefore, if recommendations for healthy individuals are applied to patients with certain types of disease, they may produce harm. A general guide to the requirements for sodium and potassium in patients with gastrointestinal fluid loss (above those for maintenance) is provided in Table 1.2, which shows the electrolyte content of various fluids. A person with a loss of 1.5 litres of small-intestinal fluid may require ~150 mmol of sodium above maintenance (the RNI for sodium is 70 mmol/day according to UK reference standards), whereas loss of the same volume of nasogastrically aspirated fluid requires only ~90 mmol extra sodium. Note that the requirements for potassium in patients losing gastrointestinal fluids are generally much lower than those for sodium (Table 1.2).
Excessive salt and fluid administration can be just as detrimental as inadequate intake, causing fluid retention and heart failure in some individuals. Fluid retention is often detected clinically by noting pitting oedema at the ankles or over the sacrum, but oedema can also affect internal tissues and organs, causing a variety of problems. Some of these problems are shown in Table 1.3. A recent study has questioned the routine clinical practice of administering large amounts of fluid in the early postoperative period in an attempt to reduce the risk of hypotension. In a randomised controlled trial carried out in Denmark, routine fluid administration was compared with a fluid-restricted regimen that aimed to approximately maintain body weight. In those receiving routine fluid therapy, not only did body weight increase significantly more than in the fluid-restricted group, but it significantly increased a variety of complications, including tissue-healing and cardiopulmonary complications. It also increased mortality, but this did not reach statistical significance, possibly because only a small number of subjects died during the course of the study. Acute accidental and elective surgical trauma is associated with a tendency to retain salt and water, at least partly because of increased secretion of mineralocorticoids and antidiuretic hormone. Therefore, administration of excess salt and water as in protein–energy malnutrition may lead to fluid retention that would not occur in normal subjects.
Table 1.2 Electrolyte contents of some body secretions (mmol/l).
| Secretion/excretion | Na | K |
| Gastric | 60 | 10 |
| Pancreatic | 140 | 5 |
| Biliary | 140 | 5 |
| Small-intestinal | 100 | 10 |
| Diarrhoea | 60a | 20 |
| Faeces | 25 | 55 |
| Sweat | ||
| insensible | 10 | 10 |
| visible | 60 | 10 |
a Variable (30–140 mmol/l)
Protein
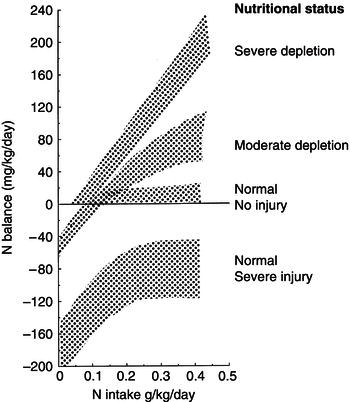
Another difference between nutritional requirements in health and disease concerns body composition and nutrient balance. In healthy adults, nutritional intake aims to maintain body composition (lean body mass and fat mass) within a desirable range, but this may not be the case in subjects with disease-related malnutrition in whom there is a need to replete tissues so that body function can improve. The response of the body to nutritional support also varies between health and disease with or without malnutrition. Consider the effect of increasing protein intake in normal, depleted, and catabolic subjects (severe acute disease), all of whom are close to energy balance (Figure 1.3). In healthy subjects, nitrogen (N) (1 g N = 6.25 g protein) balance is achieved with an intake of 0.105 g N/kg/day (the RNI necessary to achieve balance in 97.5% of the population is ~0.13 g N/kg/day according to World Health Organization (WHO) reference data). Increasing the N intake above this amount leads to little or no further net protein deposition. Depleted subjects continue to deposit protein (positive N balance) when intake is increased above 0.1 (and above 0.13) g N/kg/day, while catabolic patients show a negative N balance, with little improvement above an intake of ~0.25 g N/kg/day. With this in mind, protein requirements take into account the need to limit, but not necessarily abolish, N losses in catabolic patients, and the need to replete tissues in malnourished patients so that their function improves. These criteria differ from those in healthy, well-functioning adults, who have no need to change their body composition. In contrast, in healthy children it is necessary to cater for growth and development, which is associated with deposition of tissue and a positive N balance. Similar considerations apply to calculating the requirements of other nutrients and of energy, but metabolism in health and disease differs in a number of ways, which affects concepts about requirements.
Table 1.3 Some problems caused by oedema.
| Site of oedema | Consequence |
| Liver | Abnormal liver-function tests |
| Gastrointestinal tract | Impaired gastric motility with subsequent delay in the time taken to tolerate oral food and recover from abdominal surgery; impaired absorption |
| Brain | Impaired consciousness in those with a head injury associated with some preexisting cerebral oedema |
| Wounds | Delayed healing |
Figure 1.3 Effect of increasing protein (N) intake on N balance in depleted, healthy, and catabolic patients close to energy balance.