Phyllodes Tumors
Kristine E. Calhoun
Kimberly H. Allison
Janice N. Kim
Habib Rahbar
Benjamin O. Anderson
PHYLLODES NOMENCLATURE
Phyllodes tumors are fibroepithelial breast tumors capable of a diverse range of biological behavior. Also termed “phylloides tumors” or “cystosarcoma phyllodes,” these lesions are similar to benign fibroadenomas in their least aggressive form, but with an increased propensity for local recurrence following excision. Although the original term, “cystosarcoma phylloides,” coined by Johannes Müller in 1838 was used to describe the tumor’s grossly fleshy physical appearance, it was not intended to indicate metastatic potential as is typically implied by the term “sarcoma” (1). Phyllodes tumors in their most aggressive form, however, can recur locally and distantly, typically degenerating into a sarcomatous lesion lacking an epithelial component (2). Fortunately, this malignant form of phyllodes is uncommon, with fewer than 5% of lesions ever developing distant metastases (3). Various histologic classification schemes have been used to subtype phyllodes based on histologic features that have been associated with clinical behavior. The World Health Organization (WHO) recommends classification of phyllodes into three subtypes as follows: benign phyllodes, borderline phyllodes (also known as “low grade malignant”) and malignant phyllodes (also known as “high grade malignant”) (4).
PATHOLOGIC CHARACTERISTICS
Macroscopic Appearance
Nonmalignant phyllodes tumors typically have a gross appearance similar to fibroadenomas, presenting as a circumscribed, round or oval mass that lacks a true histologic capsule but which generally can be easily shelled out from surrounding tissues. Malignant forms have less circumscription and often gross infiltration of surrounding breast tissue. In contrast to the classic stellate, depressed gross appearance of an invasive carcinoma of the breast, phyllodes tumors typically bulge from the surrounding tissue when cut and have a multi-nodular, fleshy appearance. Most phyllodes tumors are detected in the 1 to 2 cm range but there are reports in the literature of lesions ranging from less than 1 cm up to 40 cm (5).
Microscopic Appearance
Histologically, phyllodes tumors have a broad range of appearances, from those that resemble fibroadenomas to others that appear as outright sarcomatous lesions. Like fibroadenoma, phyllodes tumors are fibroepithelial lesions composed of both stromal and epithelial components, with both layers capable of manifesting a range of histopathologic
changes. The characteristic “leaf-like” architecture of phyllodes tumors is the result of a stromal proliferation with formation of elongated cleft-like spaces lined by epithelium that extend into cystic spaces (Fig. 62-1). This leaf-like, or intracanalicular, growth pattern may not be present in all tumors, particularly those toward the malignant end of the spectrum, where the epithelial component is typically minimal or absent (Fig. 62-2). The epithelium is generally single layered, but hyperplasia, atypical hyperplasia, in situ carcinoma, and/or epithelial metaplasia may be seen as well (6 and 7). It is the stromal characteristics rather than the epithelial features, however, which determine WHO subclassification and clinical behavior of phyllodes tumors.
changes. The characteristic “leaf-like” architecture of phyllodes tumors is the result of a stromal proliferation with formation of elongated cleft-like spaces lined by epithelium that extend into cystic spaces (Fig. 62-1). This leaf-like, or intracanalicular, growth pattern may not be present in all tumors, particularly those toward the malignant end of the spectrum, where the epithelial component is typically minimal or absent (Fig. 62-2). The epithelium is generally single layered, but hyperplasia, atypical hyperplasia, in situ carcinoma, and/or epithelial metaplasia may be seen as well (6 and 7). It is the stromal characteristics rather than the epithelial features, however, which determine WHO subclassification and clinical behavior of phyllodes tumors.
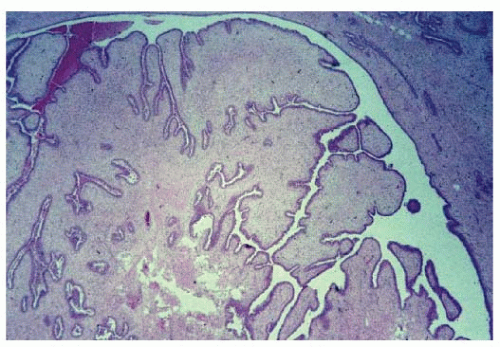 FIGURE 62-1 Phyllodes tumor illustrating characteristic “leaf-like” architecture. This histopathology image is from the borderline phyllodes tumor surgical case shown in Figure 62-5. |
Histologic Classification
Numerous studies have attempted to determine which histologic features of phyllodes tumors are useful in predicting clinical behavior (8, 9, 10, 11 and 12). The WHO classification of phyllodes tumors is based on characterization of multiple features of the stromal component of the lesion including degree of stromal cellular atypia, mitotic activity per 10 high-power fields (hpfs), presence or absence of stromal overgrowth, defined as a single 40X field of pure stroma devoid of epithelium, and infiltrative versus circumscribed tumor margins (Table 62-1). Benign phyllodes tumors (low-grade lesions) are characterized by increased stromal cellularity with no more than mild to moderate cellular atypia, circumscribed tumor margins, low mitotic rates (generally less than 4/10 hpf), and a lack of stromal overgrowth. Borderline phyllodes tumors are characterized by a greater degree of stromal cellularity and atypia, microscopically circumscribed or infiltrative borders, and mitotic rates in the 4-9/10 hpf range, but a lack of stromal overgrowth (Fig. 62-3). Malignant phyllodes tumors (high-grade lesions) are characterized by marked stromal cellularity and atypia, infiltrative borders, high mitotic rates (generally greater than 10/10 hpf), and areas of stromal overgrowth (Fig. 62-2). Over 50% of lesions are classified as benign in most large series. Alternatively, some authors continue to refer to tumors as low-, intermediate-, or high-grade lesions as advocated by Azzopardi and Salvadori (13, 14). Unfortunately, some tumors do not fit neatly into one of these three categories and tumors can have a range of behaviors within each category.
Immunohistochemistry
There has been interest in identifying immunohistochemical markers that can predict outcome. However, most of the markers identified to date are associated with grade of phyllodes lesions and have not proven to have clinical utility in predicting outcome. Increased MIB1 (Ki-67), p53, c-kit (CD117), and EGFR expression have all been associated with higher grade lesions (15, 16, 17, 18, 19, 20, 21 and 22). To date, no marker has been found to conclusively and reproducibly classify lesions or predict recurrence and metastasis.
Molecular Characteristics of Phyllodes Tumors
Due to their similarity to fibroadenomas, and the heterogeneity that can exist in any given phyllodes tumor, many theorize that phyllodes tumors arise from preexisting fibroadenomas. Studies have suggested phyllodes tumors can progress from fibroadenomas based on clonal analysis of the stroma and loss of heterozygosity analyses (23, 24). Whether all phyllodes tumors originate as fibroadenomas or conversely start de novo is still a matter of debate.
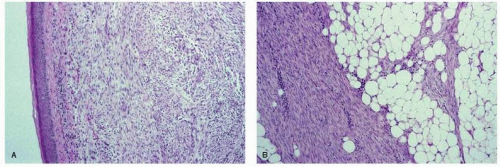 FIGURE 62-2 Recurrent malignant phyllodes tumor showing (A) dermal infiltration and (B) stromal overgrowth with infiltration of surrounding fatty breast tissue. Note the loss of epithelial elements from this recurrent tumor. These histopathology images are from the surgical case illustrated in Figure 62-8. |
TABLE 62-1 Histologic Features Used in the WHO Classification of Phyllodes Tumor Subtypes | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
More recent gene expression profiling data looking at the spectrum of phyllodes tumors supports the categorization of phyllodes tumors into benign, borderline, and malignant categories (25). Genes important in differentiating these categories are related to matrix production, cell adhesion, epidermis formation, and cell proliferation. Chromosomal changes associated with malignant phenotypes of phyllodes tumors have also been identified, with 1q gains being more common in the borderline and malignant categories and in general increasing numbers of chromosomal alterations with increasing malignancy. However, because these changes are often unique, characteristic genetic changes that could be useful in classification and prognosis have not yet been reproducibly identified.
Differential Diagnosis
The differential diagnosis for benign phyllodes tumors includes cellular fibroadenoma and juvenile fibroadenoma. Distinction of benign phyllodes tumors from fibroadenoma variants can be challenging. Cellular fibroadenomas have increased stromal cellularity, generally lack the prominent intracanalicular (leaf-like) growth pattern of phyllodes tumors and have a negligible mitotic rate (although some authors allow for rare mitotic figures up to 3/10 hpfs). Juvenile fibroadenomas are similar but are characterized by pronounced epithelial hyperplasia. Phyllodes tumors can also be quite heterogeneous, with areas indistinguishable from classic fibroadenoma and other areas of more clearly atypical stromal elements.
On the malignant end of the spectrum, the main differential diagnosis includes metaplastic carcinoma. This differential can be especially challenging when a malignant spindle cell lesion is present without identifiable epithelial elements. Usually, identification of a typical infiltrating ductal carcinoma or residual phyllodes tumor architecture can help distinguish between metaplastic carcinoma and phyllodes tumor. For cases in which only malignant stroma is present, a panel of immunostains including cytokeratins can also assist in this differential diagnosis.
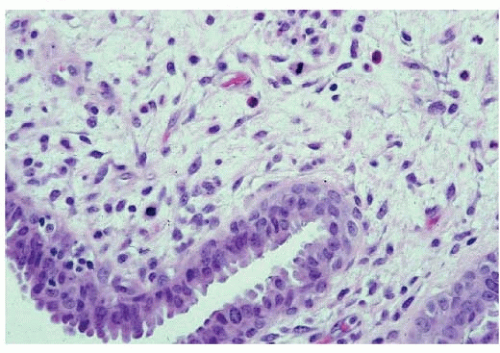 FIGURE 62-3 Borderline phyllodes tumor demonstrating intermediate level of mitotic activity and lacking stromal overgrowth. This histopathology image is from the surgical case illustrated in Figure 62-5. |
CLINICAL CHARACTERISTICS
Incidence
Phyllodes tumors are uncommon breast masses, accounting for 0.3% to 1% of breast tumors in females. In one review of 8,567 breast cancer cases treated between 1969 and 1993, only 32 cases of phyllodes tumors (0.37%) were identified among 31 patients (26). More recent series have reported numbers ranging from 33 to 821 patients (27, 28 and 29). A population-based study from California noted a higher risk in Latino than in white or Asian women (30), while another study found a propensity for higher grade tumors among Hispanic patients (31). Phyllodes tumors have been reported in males but are extremely rare, occurring in conjunction with gynecomastia and lobular development in male breast tissue (32).
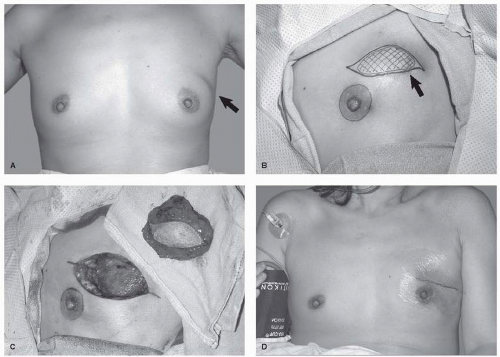
Most patients with phyllodes tumors tend to be in their 40s, a decade or so older than women diagnosed with palpable fibroadenomas. While those with benign phyllodes lesions are typically up to a decade younger than those with malignant tumors, these tumors have been reported in prepubertal females as well as elderly patients (Fig. 62-4).
Clinical Presentation
Typically, phyllodes tumors present as painless, palpable masses in the breast that demonstrate continuous growth, although some individuals may report rapid growth in a previously stable, long-standing nodule (3). Often, the history will be that of a breast mass with rapid clinical progression, growing to a relatively large size in a matter of a few months.
The mass may produce visible bulging when tumors expand quickly (Fig. 62-5A). Although tumors may grow quickly, rapid growth does not necessarily indicate malignancy. Shiny, stretched, and attenuated skin with varicose veins can overlie a phyllodes tumor as it pushes against the skin. In neglected cases, skin ulceration may develop from ischemia secondary to stretching and pressure. Such skin changes can occur with all types of lesions, so while ulceration associated with carcinoma is an indication of malignant behavior (T4 lesion), it is not necessarily an indication of a malignant phyllodes tumors. The nipple may be effaced, but invasion and/or retraction is unusual (3), as is bloody nipple discharge.
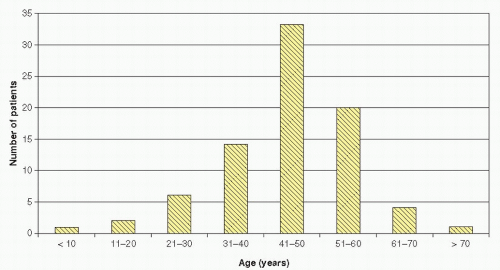 FIGURE 62-4 Age distribution of women diagnosed with phyllodes tumors. (Modified from Salvadori B, Cusumano F, Del Bo R, et al. Surgical treatment of phyllodes tumors of the breast. Cancer 1989;63(12):2532-2536.) |
Risk Factors
No clear risk factors for the development of phyllodes tumors have been identified in the general risk population. Patients with germline p53 mutations (Li-Fraumeni syndrome) are at increased risk for developing these lesions, but this represents only a small portion of diagnosed tumors (33).
Associated Tumors and Bilaterality
Bilateral phyllodes tumors (synchronous or metachronous) have been reported but are uncommon. An Memorial Sloan Kettering Cancer Center (MSKCC) series of 293 patients found only 10 individuals (3.4%) with bilateral lesions (34). Typically, concurrent tumors have similar histology, but in one documented case, a patient presented with a benign phyllodes tumor in one breast and a synchronous malignant phyllodes tumor in the other (35).
Patients can present with phyllodes tumors as well as separate noninvasive (36) or invasive breast carcinoma lesions (37). Occasionally, foci of intraductal and/or invasive carcinoma may also be found in association with a malignant phyllodes tumor (38). Because phyllodes tumors are so uncommon, it is unclear if there is any physiologic connection between these and other breast tumors when they occur in the same patient, such as a familial genetic abnormality predisposing to both lesions. Finally, pregnancy associated phyllodes tumors are rare, with fewer than 10 reported in the literature (39).
DIAGNOSIS
Clinical Features
Preoperative clinical suspicion of a phyllodes tumor is helpful but, because the lesions resemble fibroadenomas both on imaging and tissue sampling, this can be challenging. Short of being suspicious due to the large size of the mass or rapid growth of a pre-existing lesion, the majority of phyllodes tumors will be diagnosed postoperatively. In an individual series of 21 cases, only 6 (29%) were successfully identified before surgery on the basis of clinical features and/or preoperative diagnostic investigations (40). Most phyllodes tumors, therefore, are surgically “shelled out” (enucleated) at initial intervention, resulting in the inadequate surgical margins associated with an increased risk of local recurrence in the absence of additional surgery.
Imaging Features
On imaging, phyllodes tumors commonly resemble large fibroadenomas (Fig. 62-6A), and there are no distinct imaging characteristics that can reliably distinguish benign from malignant phyllodes tumors (41). Like fibroadenomas, phyllodes tend to present mammographically as round, oval, or lobular-shaped masses with circumscribed margins (Fig. 62-6B), and occasionally contain calcifications (41, 42). Sonographically, phyllodes tumors present as oval or round-shaped, hypoechoic, well-circumscribed, solid masses (Fig. 62-6C) that may contain scattered cystic regions (41, 42 and 43). Although large size (>3 cm) and presence of intramural cystic regions or clefts make the diagnosis of phyllodes tumor more likely, these features can also be present in fibroadenomas. Thus, any circumscribed mass presenting on imaging with large initial size or significant interval growth warrants excision to rule out phyllodes tumor.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree