Abstract
Partial breast irradiation encompasses a variety of techniques including accelerated partial breast irradiation (APBI) and intraoperative radiation therapy (IORT). APBI includes multicatheter brachytherapy, applicator based brachytherapy, and external-beam techniques. With the publication of five randomized trials demonstrating no difference in local recurrence with APBI compared with whole breast irradiation, APBI is increasingly being used and considered a standard treatment option for appropriately selected women after breast conserving surgery. IORT, although promising in its ability to complete treatment at the time of surgery, has been shown in two randomized trials, using different techniques, to have higher rates of local recurrence compared with whole breast irradiation. At this time, IORT remains investigational with further studies required in light of the findings of the randomized studies to date, a lack of mature data, and an inability to provide clinicians with evidence based consensus guidelines on patient selection.
Keywords
breast cancer, partial breast irradiation, accelerated partial breast irradiation, brachytherapy, intraoperative radiation therapy
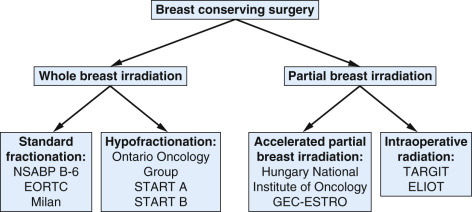
With more than 20 years of follow-up, multiple randomized studies have demonstrated equivalent outcomes between mastectomy and breast conserving therapy. Furthermore, multiple studies have demonstrated an increase in local recurrence with the omission of radiation therapy after breast conserving surgery (BCS), and a meta-analysis has demonstrated an improvement in breast cancer mortality with the addition of radiation therapy to BCS. As part of the randomized trials, radiation therapy primarily consisted of whole breast irradiation (WBI) using two-dimensional techniques. Over the past several decades, WBI has evolved and with modern radiation delivered using three-dimensional (3D) techniques that allow for improved target coverage and sparing of the heart and other organs at risk. The duration of WBI is typically 3 to ![]() weeks, often including a tumor bed boost, which can make compliance difficult for some patients. Multiple studies have documented that up to 15% to 20% of patients forgo adjuvant radiation therapy, and another subset of patients forgo breast conservation altogether due to an inability to receive adjuvant radiation therapy. Although recent studies have documented the clinical efficacy and toxicity profile of hypofractionated WBI, reducing the treatment duration to 3 weeks, many patients continue to seek alternatives that shorten the duration of radiation therapy. Partial breast irradiation represents a variety of techniques that allows for adjuvant radiation therapy to be delivered in 1 week or less ( Fig. 51.1 ).
weeks, often including a tumor bed boost, which can make compliance difficult for some patients. Multiple studies have documented that up to 15% to 20% of patients forgo adjuvant radiation therapy, and another subset of patients forgo breast conservation altogether due to an inability to receive adjuvant radiation therapy. Although recent studies have documented the clinical efficacy and toxicity profile of hypofractionated WBI, reducing the treatment duration to 3 weeks, many patients continue to seek alternatives that shorten the duration of radiation therapy. Partial breast irradiation represents a variety of techniques that allows for adjuvant radiation therapy to be delivered in 1 week or less ( Fig. 51.1 ).
The rationale for WBI is the assumption of the potential for microscopic disease beyond the lumpectomy cavity. However, patterns of failure for patients undergoing breast conservation do not validate this hypothesis because the majority of ipsilateral breast tumor recurrences (IBTRs) occur within close proximity to the lumpectomy cavity, “true recurrences,” with lower rates of failures elsewhere in the breast. Furthermore, multiple studies have confirmed that the incidence of metachronous new primaries is not altered by the delivery of WBI. Finally, pathologic specimen evaluation has documented that in patients undergoing BCS with negative margins that residual disease is most likely located within 1 to 2 cm of the surgical cavity. Taken together, these data support the concept of partial breast irradiation, treating the breast tissue in the periphery of the lumpectomy cavity rather than the whole breast in selected patients. This chapter focuses on partial breast irradiation techniques, including accelerated partial breast irradiation (APBI) and intraoperative radiation therapy (IORT).
Accelerated Partial Breast Irradiation
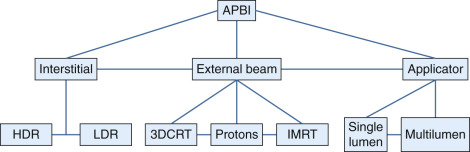
APBI can be delivered using several techniques and fractionation schemes with the most common techniques being interstitial brachytherapy, applicator-based brachytherapy, and external-beam techniques ( Fig. 51.2 ). Interstitial brachytherapy represents the original APBI technique with the longest follow-up to date, followed by development of single lumen applicators and subsequently multilumen applicators and external-beam techniques.
Interstitial Accelerated Partial Breast Irradiation
The interstitial brachytherapy technique had traditionally been used for boost after WBI before the introduction of electron beams on linear accelerators and thus was the first technique used for APBI as monotherapy. A prospective Hungarian trial (1996–1998) with 12-year follow-up used the high-dose-rate (HDR) interstitial multicatheter technique as monotherapy for APBI and demonstrated a 9.3% rate of IBTR in a series of 45 patients with early-stage disease (tumor <2 cm, negative margins, negative nodes [N1mi allowed], low-grade). Toxicity rates were low with a 2% rate of grade 3 fibrosis and a 2% rate of fat necrosis, with 78% of patients having excellent/good cosmesis. This prompted a randomized trial comparing partial breast irradiation (PBI) and WBI in women with early-stage breast cancer (T1N0-1mi, grade 1–2, nonlobular histology, negative margins). Radiation on the partial breast arm was delivered with interstitial brachytherapy (HDR: 7 × 5.2 Gy) or electrons (50 Gy/25 fractions). At 10 years, no difference in the rate of local recurrence was noted (5.9% PBI vs. 5.1% WBI) with no difference in disease-free, cancer-specific, or overall survival noted as well. PBI was associated with improved cosmetic outcomes (81% vs. 63% excellent/good cosmesis). Similarly, a matched pair analysis (matched for age, size, nodal status, estrogen receptor status, hormonal therapy) from William Beaumont Hospital comparing 199 patients receiving interstitial APBI with 199 patients receiving WBI found no difference in 12-year outcomes including local recurrence (3.8% WBI vs. 5.0% APBI), which was confirmed by a second matched pair analysis from Washington University (3.8% WBI vs. 3.0% APBI). These outcomes were recently validated by the Groupe Européen de Curiethérapie-European Society for Therapeutic Radiology and Oncology trial; this multiinstitutional phase III noninferiority trial randomized 1184 patients to interstitial APBI with HDR/pulsed-dose-rate (PDR) implants or WBI with a boost after BCS. Five-year outcomes demonstrated no difference in local recurrence with interstitial brachytherapy (0.9% WBI vs. 1.4% APBI), along with no difference in survival. With respect to toxicity, APBI was associated with a reduction in breast pain and a trend for reduced late grade 2 to 3 skin toxicity (5.7% APBI vs. 3.2% WBI).
Radiation Therapy Oncology Group (RTOG) 9517 was a Phase II trial evaluating interstitial brachytherapy with both low-dose-rate (LDR; n = 33, 45 Gy in 3.5–5 days) and HDR (n = 66, 34 Gy in 10 fractions twice daily) multicatheter implants. Five-year local recurrence rates of 3% and 6% were noted for the HDR and LDR cohorts respectively. With regard to toxicity, 13% developed grade 3 skin toxicity with 66% to 68% rates of excellent/good cosmesis. These findings have been confirmed by other single-institution prospective studies as well as retrospective studies that have documented low rates of recurrence and toxicity with high rates of excellent/good cosmetic outcomes that remained stable over time. With respect to dose and fractionation, the majority of studies have used 34 Gy/10 fractions twice daily or 32 Gy/8 fractions twice daily, whereas the Hungarian randomized study used 36.4 Gy/7 fractions twice daily. In cases in which LDR is used, 45 to 50 Gy over 3 to 5 days has commonly been administered. A summary of selected multicatheter interstitial APBI studies are presented in Table 51.1 .
| Trial/Institution | Patients (n) | Study Type | Median Follow-Up (months) | Technique | Outcomes |
|---|---|---|---|---|---|
| GEC-ESTRO | 1184 | Randomized | 78 | HDR/PDR | No difference in 5-year local recurrence (0.9% vs. 1.4%); APBI reduced breast pain |
| National Institute of Oncology Hungary | 128 PBI (88 HDR) | Randomized | 124 | HDR/ electrons | No difference in 10-year local recurrence (5.9% vs. 5.1%); excellent/good cosmesis |
| William Beaumont Hospital | 199 | Matched Pair | 127 | HDR | No difference in 12-year local recurrences (3.8% vs. 5.0%) |
| Washington University | 202 | Matched Pair | 60 | HDR | No difference in 5-year local control (97% vs. 96.2%); excellent/good cosmesis 95%, 10.1% rate of symptomatic fat necrosis |
| National Institute of Oncology Hungary | 45 | Prospective | 133 | HDR | 12-year local recurrence 9.3%; excellent/good cosmesis 78%, 2.2% grade 3 fibrosis, 2.2% fat necrosis requiring surgery |
| RTOG 9517 | 99 | Prospective | 73 | HDR (66)/ LDR (33) | 5-year local recurrence 3% HDR/6% LDR; excellent/good cosmesis 66%, 13% grade 3 toxicity |
| Harvard University | 50 | Prospective | 134 | LDR | 12-year local recurrence 15%; excellent/good cosmesis 67%, 9%/13% grade 3/4 toxicity, 54% moderate/severe fibrosis, 35% fat necrosis |
| Multi-Institutional (Germany/Austria) | 274 | Prospective | 63 | PDR (175)/ HDR (99) | 5-year local recurrence 2%; excellent/good cosmesis 90%, 0.4%/2.2% grade 3 + fibrosis/telangiectasia |
| Ochsner Clinic | 50 | Prospective | 75 | LDR/HDR | Local recurrence 2%; 8% grade 3 or 4 toxicity; comparable outcomes, toxicity, cosmesis compared with WBI cohort |
| Tufts/Brown University | 75 | Retrospective | 73 | HDR | Excellent/good cosmesis 91% |
| University of Wisconsin | 247 | Retrospective | 48.5 | HDR | Local recurrence 2%; Excellent/good cosmesis 93%, |
| Virginia Commonwealth University; | 44 | Retrospective | 42 | LDR (11)/HDR (31) | Local recurrence 0%; excellent/good cosmesis 80% LDR/90% HDR |
| Orebro University | 50 | Retrospective | 86 | PDR | 7-year local recurrence 4%; excellent/good cosmesis 56%, 12% fat necrosis |
Applicator Accelerated Partial Breast Irradiation
Interstitial brachytherapy represented a technique that allowed for the delivery of APBI with excellent clinical outcomes. However, due to the technical complexity associated with inserting the catheters, it has been limited to a small number of centers. However, with the introduction of single-entry applicators whose insertion is less technically demanding, brachytherapy-based APBI became more widely available for patients and is used at a growing number of centers. The initial clinical studies, after US Food and Drug Administration approval in 2002, were performed using the single-lumen MammoSite (Hologic, Bedford, MA) applicator. Benitez and colleagues published results from the initial study of 43 patients with no local recurrences at 5 years and 83% excellent/good cosmesis. Toxicity rates were low including a 9.3% rate of infection and 12% symptomatic seroma rate. Importantly, a skin spacing target of 7 mm was identified to reduce skin toxicity, such as telangiectasias, and improve cosmetic outcomes. The success of this study led to the prospective American Society of Breast Surgeons (ASBS) MammoSite Registry, which enrolled 1449 patients from 2002 to 2004. With a median follow-up of 63 months, the 5-year IBTR rate was 3.8% and excellent/good cosmesis was seen in more than 90% of cases. Toxicity outcomes showed a 9.6% rate of infection, 2.5% rate of fat necrosis, and 13% rate of symptomatic seromas. Similar results have been seen by multiple prospective, multiinstitutional, and single-institution studies.
Although the initial applicator studies used a single lumen device, advances in design allowed for the development of multilumen applicators providing for more dosimetric degrees of freedom. Multiple dosimetric studies have been performed demonstrating improvements in target coverage as well as reduction in dose to the chest wall, normal breast tissue, and skin, even in cases with limited skin distance. Mature data beyond 5 years are limited with this technique, but initial studies have demonstrated low rates of toxicity and excellent clinical outcomes. A multiinstitutional series with 3-year outcomes found the local recurrence rate to be 2.2% in a series of 342 patients, with a 4.4% rate of persistent seromas and 8.5% rate of infection. Excellent/good cosmesis was noted in 88% of patients with these findings substantiated by additional studies. Table 51.2 presents a summary of selected applicator APBI studies.
| Trial/Institution | Patients (n) | Study Type | Follow-Up (months) | Technique | Outcomes |
|---|---|---|---|---|---|
| MammoSite Initial Study | 43 | Prospective | 65 | Single Lumen | 5-year local recurrence 0%; excellent/good cosmesis 83%, 12% symptomatic seromas, 9% infections |
| ASBS MammoSite Registry | 1449 | Prospective registry | 63 | Single Lumen | 5-year local recurrence 3.8%; excellent/good cosmesis 91%, 13% symptomatic seroma, 2.5% fat necrosis, 10% infections |
| Contura Phase 4 | 342 | Prospective registry | 36 | Multi-Lumen | 3-year local recurrence 2.2%; excellent/good cosmesis 88%, 4.4% symptomatic seroma, 8.5% infection |
| Multi-Institutional (Germany) | 23 | Prospective | 20 | Single Lumen | 39% serious seroma, 26% telangiectasia, 56% hyperpigmentation |
| Multi-Institutional (United States) | 483 | Retrospective | 24 | Single Lumen | 2-year local recurrence 1.2%; excellent/good cosmesis 91%, 9% infections, reduced infection with closed-cavity technique |
| William Beaumont Hospital | 80 | Retrospective | 22 | Single Lumen | 3-year local recurrence 2.9%; excellent/good cosmesis 88%, at 3 years, 10% symptomatic seromas, 11% infections, 9% fat necrosis, 88% excellent/good cosmesis |
| Rush University Medical Center | 70 | Retrospective | 26.1 | Single Lumen | Local recurrence 5.7% |
| Medical University of South Carolina | 111 | Retrospective | 46 | Single Lumen | 4-year IBTR 5%; excellent/good cosmesis 90% |
| The Breast Center, Georgia | 46 | Retrospective | 36 | Multi Lumen | Local recurrence 2%; excellent/good cosmesis 97%, 4.3% persistent seroma, 2.2% telangiectasia |
| University of California–San Diego | 100 | Retrospective | 21 | Strut Applicator | Recurrence rate 1%; 1.9% symptomatic seroma, 1.9% fat necrosis |
Two observational studies evaluated brachytherapy based APBI compared with WBI and found higher rates of mastectomy as well as higher rates of toxicity (infectious and noninfectious). The limitations of these studies include the design of the study (observational), missing data in the databases used especially regarding use of radiation, short follow-up, failure to control for relevant patient and disease characteristics as well as lack of information for evaluating the reason for the difference in mastectomy rates, and use of billing codes rather than medical records, all of which makes their findings hypothesis generating in light of mature phase III data failing to corroborate their findings. With the continued evolution of brachytherapy APBI to include multilumen applicators, it is expected that toxicity rates will continue to decline. The most common dose and fractionation scheme is 34 Gy/10 fractions twice daily; however, shorter courses (e.g., 28 Gy/4 fractions twice daily) are being investigated.
External-Beam Accelerated Partial Breast Irradiation
APBI delivered with external-beam techniques is an appealing option for many patients because it eliminates the need for another procedure after surgery. Although older series have evaluated this technique, with the advent of computed tomography simulation, 3D planning, and image guidance, external-beam APBI can be delivered in multiple techniques with greater accuracy of target volume delineation and treatment delivery. Several institutional studies have suggested increased toxicity or poorer cosmesis with 3D conformal radiation therapy (CRT) APBI external-beam techniques, potentially related to larger volumes of normal breast irradiated or specific techniques utilized. However, publication of two randomized trials evaluating external-beam APBI has provided level I data regarding the technique and support the continued study and utilization of the technique.
The 3D-CRT technique was developed at William Beaumont Hospital with initial dosimetric studies and outcomes demonstrating its feasibility. A 5-year update (205 patients) from the institution demonstrated no recurrences and reasonable rates of chronic toxicity with a 7.5%/7.6% rates of fibrosis/telangiectasias and 81% of patients having excellent/good cosmesis. Similar results were noted in several studies including a subset analysis of National Surgical Adjuvant Breast and Bowel Project (NSABP) B-39, which demonstrated low rates of fibrosis (grade 2 < 12%, grade 3 < 3%, grade 4/5 0%), and an analysis of 100 patients treated with external-beam radiation therapy APBI at New York University using the prone technique, which demonstrated an 89% rate of excellent/good cosmesis at 5 years. Also, a small randomized trial from Spain demonstrated no recurrences at 5 years with improved acute toxicity with 3D-CRT APBI. However, other single-institution studies raised concerns regarding toxicity (fibrosis) and poor cosmetic outcomes. Findings from the University of Michigan (which used intensity modulated radiation therapy [IMRT] and active breathing control) and Tufts series were confirmed in part by long-term follow-up of RTOG 0319, a phase II trial that demonstrated deterioration of cosmetic outcomes from 82% excellent/good cosmesis at 1 year to 64% at 5 years with a 5.8% rate of grade 3 toxicity. The RAPID trial randomized women after BCS to external-beam APBI (3D-CRT) or WBI (standard/hypofractionated). The trial accrued more than 2100 women, and with median follow-up of 3 years, APBI was found to have higher rates of grade 1 and 2 toxicity (telangiectasias, induration, breast pain, fat necrosis) with no difference in the rates of grade 3 toxicity (1.4% vs. 0%). Cosmetic outcomes were inferior with 3D-CRT APBI. An alternative to 3D-CRT APBI is to use IMRT; initial outcomes from this technique were promising with a phase II study of 136 patients from Lei and colleagues demonstrating a 4-year IBTR rate of 0.7% with 88% to 91% excellent/good cosmesis and low rates of toxicity noted. A randomized study from Florence compared IMRT APBI with WBI delivered with IMRT (standard fractionation); at 5 years, no difference in rates of local recurrence were noted and acute toxicity was improved with APBI (0% vs. 6.5%), as was excellent/good cosmesis (95.1% vs. 89.6%). The dose and fractionation most commonly used is 38.5 Gy/10 fractions BID; however, recent data have demonstrated excellent clinical and toxicity outcomes with 30 Gy/5 fractions every other day. Similarly, an abstract of the IMPORT-LOW trial demonstrated that with 5.8 years of follow-up that once daily fractionation (40 Gy/15 fractions) to the partial breast was noninferior to WBI or WBI with a simultaneous integrated boost (0.5% vs. 1.1% vs. 0.2%) with respect to recurrences as well as toxicity. Table 51.3 provides a summary of selected external-beam APBI series.
| Trial/Institution | Patients (n) | Study Type | Follow-Up (months) | Technique | Outcomes |
|---|---|---|---|---|---|
| RAPID | 2135 | Randomized | 36 | 3D-CRT | Increased adverse cosmesis with APBI (26% vs. 18%, per patients), increase grade 1–2 toxicity with 3D-CRT |
| University of Florence | 520 | Randomized | 60 | APBI | No difference in local recurrence or survival; improved cosmesis with IMRT APBI (95.1% vs. 89.6%) and reduced rates of acute toxicity |
| IMPORT LOW | 2018 | Randomized | 68 | 3D-CRT | No difference in local recurrence: 1.1% WBI vs. 0.2% (WBI with simultaneous boost to cavity) vs. 0.5% PBI |
| Hospital de la Esperanza | 102 | Randomized | 60 | 3D-CRT | No local recurrences, APBI lower acute toxicity, no difference chronic toxicity |
| NSABP B-39/RTOG 0413 | 1367 | Randomized | 41 | 3D-CRT | Grade 2 fibrosis 12%, grade 3 3% |
| RTOG 0319 | 52 | Prospective | 63 | 3D-CRT | Local recurrence 6%; excellent/good cosmesis 82% year 1/64% year 3, 5.8% grade 3 toxicity |
| University of Michigan | 34 | Prospective | 60 | IMRT | Local recurrence 3%; excellent/good cosmesis 73%, 3.3% grade 2 fibrosis, |
| New York University | 100 | Prospective | 64 | 3D-CRT-prone | Local recurrence 1%; excellent/good cosmesis 89%, grade 3 toxicity 2% |
| Rocky Mountain | 136 | Prospective | 53.1 | IMRT | Ipsilateral failure 0.7%; excellent/good cosmesis 88%, 3.6% telangiectasia, 1.4% rib fracture |
| Canadian Multi-Institutional Trial | 104/87 with 3-year + follow-up | Prospective | 36 (minimum) | 3D-CRT | One local recurrence; excellent/good cosmesis 82%, 1 grade 3 toxicity |
| Tufts University | 80 | Retrospective | 32 | 3D-CRT | Excellent/good cosmesis 81%, 7.5% grade 3/4 fibrosis, 11% fat necrosis |
| William Beaumont Hospital | 192 | Retrospective | 56 | 3D-CRT | Local recurrence 0%; excellent/good cosmesis 81%, 7.5% grade 3 fibrosis, 7.6% telangiectasias |
Proton therapy represents an alternative external-beam technique compared with 3D-CRT and IMRT ( Table 51.4 ). This technique has undergone continued refinement because of initial concerns regarding toxicity; a study from Massachusetts General Hospital demonstrated 79% of patients having moderate to severe skin color changes at 3 to 4 weeks after treatment and 22% moderate to severe moist desquamation at 6 to 8 weeks. A subsequent update from MGH compared outcomes of 19 patients treated with protons (32 Gy/8 fractions BID) with 79 treated with photons or mixed photons/electrons. With 7-year follow-up, proton therapy was associated with worse cosmesis (62% vs. 94% excellent/good, p = .03) as well as higher rates of skin toxicity including telangiectasias, pigmentation changes but no difference in the rates of breast pain, edema, fibrosis, fat necrosis, rib fracture, or skin desquamation. Also, although not statistically significant there was a higher rate of local recurrence noted (11% vs. 4%). An update of the Loma Linda proton experience (40 Gy/10 fractions daily) was recently published with 5-year outcomes; 100 patients were enrolled with a 3% IBTR and no grade 3 or higher acute skin toxicity. Patient and physician assessed cosmesis was 90% excellent/good cosmesis with no change noted over time. Chang and colleagues reported outcomes of a phase II trial including 30 patients treated with protons (30 CGE/6 fractions daily). With a median follow-up of 59 months, no recurrences had been identified with 69% excellent/good cosmesis at 3 years. Breast retraction was noted to increase during follow-up across all patients.
| Institution | Patients (n) | Follow-Up (months) | Outcomes |
|---|---|---|---|
| Massachusetts General Hospital | 19 | 82.5 | 7-year local recurrence 11%; 62% excellent/good cosmesis, increased late skin toxicity compared with photons |
| Loma Linda University Medical Center | 100 | 60 | 5-year local recurrence 3%; 90% excellent/good cosmesis |
| Seoul National University | 30 | 59 | 5-year local recurrence 0%; 69% excellent/good cosmesis |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








