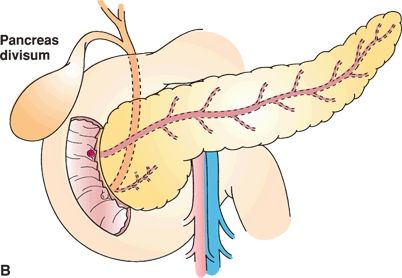
FIGURE 1.1 A. Normal pancreatic ductal anatomy. B. Failure of the ventral and dorsal buds to fuse results in pancreas divisum, in which case the majority of the pancreas drains through the duct of Santorini into the minor papilla. In these patients, the inferior portion of the head and the uncinate process continue to drain separately through the duct of Wirsung into the major papilla. (From Mulholland MW, Lillemoe KD, Doherty GM, et al. Greenfield’s surgery: scientific principles and practice, 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2005:1939.)
Annular pancreas (AP) is an uncommon variant characterized by a thin band of normal pancreatic tissue surrounding the second portion of the duodenum. Annular pancreas occurs due to incomplete rotation of the ventral pancreatic bud, so that it remains on the right side of the duodenum. The incidence of AP is approximately 1 out of 20,000 individuals. More than 60% of patients with this anomaly present during the neonatal period with features of gastric outlet obstruction. Many children with annular pancreas have other congenital abnormalities such as Down syndrome and esophageal or duodenal atresias. Children with AP typically present with duodenal obstruction (often diagnosed by prenatal ultrasound). This obstruction is treated by duodenostomy, as dividing the pancreatic annulus may lead to pancreatic fistula from dividing a main pancreatic duct. In contrast to children, adults presenting with AP often have different and more challenging pancreatobiliary disease such as pancreatitis or biliary obstruction.
ARTERIAL BLOOD SUPPLY
The pancreas has a rich blood supply derived from both the celiac trunk and the SMA (Fig. 1.2). The celiac trunk gives rise to the splenic artery, the left gastric artery, and the common hepatic artery. The common hepatic artery gives rise to the gastroduodenal artery before continuing as the proper hepatic artery. The gastroduodenal artery gives off the right gastric artery superior to the duodenum, travels inferiorly, anterior to the pancreatic neck and posterior to the duodenum, and gives rise to the right gastroepiploic artery at the inferior border of the duodenum, and then continues as the superior pancreaticoduodenal artery. This branches into the anterior and posterior superior pancreaticoduodenal arteries. The SMA gives rise to the inferior pancreaticoduodenal artery, which also divides into anterior and posterior branches. The pancreaticoduodenal arcades are always present and form an extensive network of blood vessels that supply both the pancreatic head and the second and third portions of the duodenum. This shared blood supply renders duodenal-preserving pancreatectomy a complex feat. A rim of pancreatic tissue containing the arcade must be left intact.
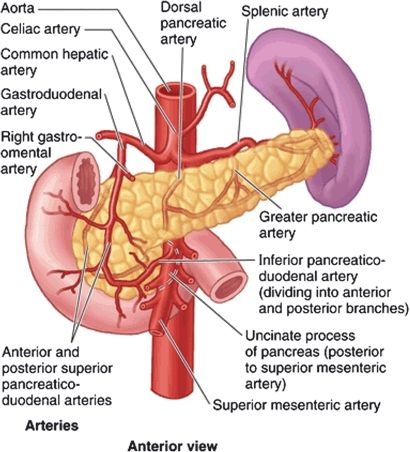
FIGURE 1.2 Arterial anatomy of the pancreas. (From Moore KL, Agur AM, Dalley AF. Clinically oriented anatomy, 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2013:266.)
Patients with celiac stenosis may derive all hepatic arterial blood flow retrograde from the SMA via collateral pancreaticoduodenal arcades. Therefore, it is prudent to temporarily occlude the gastroduodenal artery prior to dividing this vessel during pancreatic head resection. This maneuver ensures adequate antegrade hepatic arterial flow is present from the celiac artery.
The neck, body, and tail of the pancreas are supplied by many branches from the splenic artery and the SMA. The inferior pancreatic artery usually arises from the SMA and runs to the left along the inferior border of the body and tail of the pancreas, parallel to the splenic artery. Three vessels run perpendicular to the long axis of the pancreatic body and tail and connect the splenic artery and inferior pancreatic artery. They are, from medial to lateral, the dorsal, great, and caudal pancreatic arteries. At the pancreatic neck, the dorsal pancreatic artery arises from the splenic artery and gives off both right and left branches. The right branch supplies the head of the pancreas and usually joins the posterior arcade. The left branch passes through the body and tail of the pancreas, often making connections with branches of the splenic artery or left gastroepiploic artery. These arteries form arcades within the body and tail of the pancreas, and account for the rich blood supply of the organ. Detailed knowledge of the blood supply to the neck, body, and tail of the pancreas is important when performing a distal pancreatectomy with splenic preservation or a central pancreatectomy. Equally important is recognizing the broad arterial variability present.
Preoperative planning for patients with pancreatic cancer includes high-quality computed tomography imaging to evaluate the primary tumor or any sites of distant metastases, assess the patency of nearby vessels, and delineate their relationship to the primary lesion. Tumors can then be classified as resectable, locally advanced, or metastatic. A subset of tumors blurs the distinction between resectable and locally advanced. These tumors of borderline resectability include those that abut the SMA, celiac axis, or hepatic artery (<180 degrees) or display short-segment occlusion of the SMV, portal vein, or confluence of the two vessels with suitable remaining vessels for reconstruction. Locally advanced, surgically unresectable tumors include those that encase the celiac axis, hepatic artery, or SMA (>180 degrees), or that occlude the SMV, portal vein, or its confluence leaving no technical options for reconstruction. Encasement is defined as involvement of greater than 50% of the circumference of the vessel whereas abutment refers to less than 50% involvement.
Preoperative imaging also delineates aberrant vascular anatomy. The most common arterial variant is a replaced right hepatic artery that arises from the SMA instead of the proper hepatic artery. This variant is found in 10% to 15% of patients and usually courses posteriorly and superiorly from the SMA around the posterior side of the portal vein and then up to the porta hepatis on the right side. The artery may be involved by pancreatic head tumors. It must also be differentiated from the inferior pancreaticoduodenal arteries, which also arise from the SMA and take a similar course to the replaced right hepatic. Inadvertent injury or resection of a replaced right hepatic artery can lead to hepatic ischemia or compromise of the biliary enteric anastomosis. A replaced left hepatic artery, present in 10% of the population, typically arises from the left gastric artery and travels along the superior border of the lesser omentum. A replaced left hepatic artery is usually distant from pancreatic head masses but may be involved with tumors of the pancreatic body. Less common arterial variants include accessory left and right hepatic arteries, which are similar to the replaced hepatic arteries but are found in addition to the typical hepatic arterial anatomy.
VENOUS BLOOD SUPPLY
The venous drainage of the pancreas follows the arterial supply. The veins are generally located anterior to the arteries, and both veins and arteries lie posterior to the pancreatic ducts. All pancreatic veins ultimately drain into the portal vein, splenic vein, SMV, or inferior mesenteric vein. Just as an arterial arcade supplies the pancreatic head, a venous arcade of pancreaticoduodenal vessels drains this region as well. The anterior superior pancreaticoduodenal vein joins the right gastroepiploic vein, which also receives the middle colic vein, and drains directly into the SMV. Anterior traction on the transverse colon during colectomy or pancreatectomy can avulse these veins, which then retract behind the pancreas and can be difficult to control.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree