Overview of Survivorship Issues
Ann H. Partridge
Larissa Nekhlyudov
OVERVIEW
Cancer survivorship has been defined as the period of time from diagnosis through the balance of a person’s life (1). However, most care and research in this area has focused on the post-early treatment phase, and broadly encompasses not only the physical, but the psychosocial and economic sequelae of the diagnosis and treatment of cancer for individuals, their families, and society. The vast majority of people diagnosed with breast cancer will become survivors in the short term and most also in the long term. Breast cancer survivors are the largest group of cancer survivors in the United States, comprising nearly a quarter of the recently reported 13 million cancer survivors; the number is expected to grow over the next decade (2). It is not surprising, therefore, that much of the survivorship research to date has focused on this population of women, resulting in a large and growing literature in this area. Yet, there remain significant limitations in our understanding of cancer survivorship care. This chapter presents the components of survivorship care for patients with a history of breast cancer, highlights evidence-based recommendations, and acknowledges areas of uncertainty.
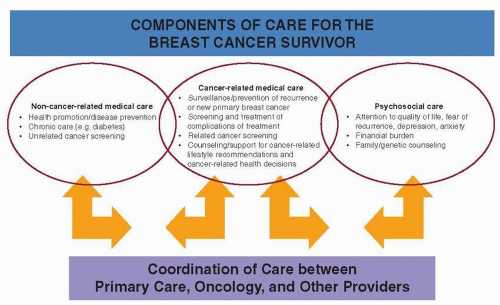
The general goals of follow-up care for patients with breast cancer are to: (i) detect recurrence or new primary disease and reduce the risk of future breast cancer events including encouraging adherence to surveillance and chronic adjuvant therapy; (ii) monitor, prevent, and/or treat longterm, late effects related to diagnosis or treatment, including medical and psychosocial risks; (iii) provide breast cancerrelated decision-making support (e.g., regarding duration of hormonal therapy, future fertility, or optimal contraception); (iv) educate and support patients to continue or adopt optimal health behaviors that may improve outcomes; and (v) assure that patients seek appropriate and timely noncancer related care, such as management and prevention of comorbid medical conditions (see Fig. 88-1).
DETECTION OF DISEASE AND RISK REDUCTION
Breast cancer survivors are at risk for locoregional or distant disease recurrence, as well as new primary breast cancer in remaining breast tissue or the contralateral breast. The risk of locoregional or distant recurrence for an individual patient is dependent on a number of disease, treatment and patient characteristics. (See Chapter 28, Clinical and Pathologic Prognostic and Predictive Factors.) In follow-up care, providers should promote and facilitate the continuation of chronic treatment (e.g., adjuvant endocrine therapy) and/or other strategies such as surveillance mammography that have been proven to lead to reduced rates of recurrence and breast-cancer mortality. For the average breast cancer survivor, the risk of developing a second primary tumor in the contralateral breast is low, approximately 0.5% to 1% per year for the first five years (3). Even though this is higher risk than for the general population, because of competing risks and the lack of clear evidence that contralateral mastectomy improves outcomes, removal of the contralateral breast is not routinely recommended. Women with genetic mutations, for example, BRCA1 or 2 mutation carriers are at dramatically increased risk of contralateral breast cancer; thus, screening for genetic risk is warranted where personal or family history suggests a potential mutation. In women who harbor a mutation or who have history suggestive of such, consideration of prophylactic efforts to reduce cancer risk in this high-risk population is standard. (see Chapter 17, Genetic Testing and Management of Patients with Hereditary Breast Cancer).
In order to detect recurrence or new primary disease, evidence-based guidelines recommend regular history and physical exam as well as mammography in follow-up but no additional screening for recurrence in the absence of prompting signs or symptoms (4). There is some controversy about the role of MRI in screening remaining breast tissue in survivors, particularly for women who are very young and/or have dense breast tissue. At the present time, while women who are at very high risk of developing new primary breast cancer (e.g., BRCA1 or 2 mutation carriers) are recommended to undergo additional breast surveillance with MRI, while this is not recommended for women at average risk (5). Given research to date suggesting lack of benefit, no additional imaging or laboratory testing (i.e., tumor markers) are recommended (see Chapter 67, Surveillance of Patients Following Primary Therapy).
MANAGEMENT AND PREVENTION OF LONG-TERM, LATE EFFECTS
Breast cancer survivors may face a number of long-term and late effects from treatment. Long-term effects are problems that become apparent during treatment and persist (e.g., taxane-related neuropathy), while late effects are those that manifest after treatment has ended (e.g., osteoporosis due to premature menopause from chemotherapy or treatmentrelated leukemia). Figure 88-2 presents common long-term/late effects from breast cancer treatments as they relate to local therapy with surgery and radiation, and systemic therapy, including chemotherapy, biologic therapy, and hormonal therapy. Most patients receive multimodality treatment and clear attribution of problems can be difficult for some symptoms such as fatigue. Further, problems may be pre-existing and may be exacerbated by the diagnosis and treatment of breast cancer (e.g., obesity, diabetes, hyperlipidemia, arthritis). Regular screening for long-term/late effects in survivors as part of a standard history and physical, and prevention and palliation where appropriate is warranted to improve symptoms, quality of life, and potentially future risks and outcomes (see Chapter 49, Implications of Obesity in Breast Cancer; Chapter 51, Management of Menopausal Symptoms in Breast Cancer Survivors; Chapter 52, Long Term and Late Effects of Primary Curative Intent Therapy: Neurocognitive, Cardiac, and Secondary Malignancies).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree