- Patients with haematological malignancies are at increased risk of malnutrition, so it is important that all patients are nutritionally assessed and receive nutritional counselling at diagnosis and during the course of treatment.
- To prevent the negative impact on nutritional status of high-dose radio- and chemotherapy, artificial nutrition is frequently indicated in haematological malignancy.
- Mucositis of the gastrointestinal tract represents the main indication for artificial nutrition in haematological malignancy.
- Haematopoietic stem-cell transplantation (HSCT) may negatively affect oral food intake and nutrient absorption, and increase nutrient and energy needs. Nutritional and metabolic intervention should be considered an integral part of supportive care of HSCT patients.
- Parenteral nutrition still represents the main tool by which to provide nutritional support to patients undergoing HSCT. Enteral nutrition is also feasible, and should be attempted as soon as gastrointestinal impairment resolves.
15.1 Introduction
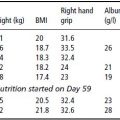
The impact of haematological malignancies on nutritional status is extremely variable and is essentially a function of disease- and treatment-related impairment in nutrient absorption, nutrient losses, and altered energy and protein metabolism. Until recently, however, little attention has been paid to the nutritional implications of haematological malignancies. Unlike solid tumours, which have a dramatic impact on a person’s metabolic homeostasis and nutritional status, haematological malignancies are, at least initially, rarely associated with a significant deterioration of nutritional status. The advent of aggressive antineoplastic regimens involving the use of high-dose combination chemotherapy, followed or not by haematopoietic stem-cell transplantation (HSCT) in order to achieve high disease remission rate and longer disease-free survival, has created a new scenario wherein nutritional and metabolic impairment occur as a consequence not of the underlying disease, but rather of the deleterious side effects of antineoplastic treatments. Therefore, patients who are initially well nourished (as most haematological patients are) may become acutely at risk of malnutrition or overtly malnourished, making nutritional intervention necessary (Table 15.1).
This chapter will mainly focus on the nutritional sequelae of the therapeutic regimens for haematological diseases, including HSCT.
15.2 Haematological malignancies
Haematological malignancies represent a heterogeneous group of diseases, including leukaemia, lymphoma, and other lympho-myeloproliferative disorders.
Table 15.1 Disease-dependent and treatment-dependent nutritional risks in haematological malignancies.
| Disease | Disease-dependent nutritional risks | Treatment-dependent nutritional risks |
| Myelodysplastic syndromes | × | |
| Acute myeloid leukaemia | × | |
| Chronic myeloid leukaemia | × | × |
| Acute lymphocytic leukaemia | × | |
| Chronic lymphocytic leukaemia | × | |
| Hodgkin’s lymphoma | × | × |
| Non-Hodgkin’s lymphoma | ×a | × |
aWeight loss is more frequent in high-grade lymphomas.
Myeloproliferative disorders
Myeloproliferative disorders are caused by acquired clonal abnormalities of the haematopoietic stem cells. They produce characteristic syndromes with a well-defined clinical and biological picture, which can show either a more indolent behaviour, like chronic myeloid leukaemia (CML), polycythemia vera, essential thrombocytemia, and myelofibrosis, or more aggressive features, like acute myeloid leukaemia (AML) and high-risk myelodysplastic syndrome (MDS). These conditions require an intensive treatment, but in a proportion of cases they fail to respond or relapse after an initial response to therapy.
Nutritional intervention is most frequently indicated for patients with MDS and AML.
Myelodysplastic syndrome
MDS is characterised clinically by a hyperproliferative bone marrow, reflective of ineffective haematopoiesis, and is accompanied by one or more peripheral blood cytopaenias. Bone-marrow failure results, leading to death from bleeding and infection in the majority, while transformation to acute leukaemia occurs in up to 40% of patients. Supportive therapy with transfusions and growth factors (erythropoietin, granulocyte colony-stimulating factor) and hormonal therapy (androgens, danazol) have a limited indication for the forms at low risk of trasformation in acute leukaemia. In high-risk MDS, long-term results with conventional chemotherapy are disappointing. In recent years, the introduction of demethylating and differentiating agents has seemed promising. In young patients with high-risk MDS, the use of high-dose chemotherapy followed by allogeneic bone-marrow or peripheral blood stem-cell (PBSC) infusion is also utilised as first-line therapy.
Acute myeloid leukaemia
AML is the most common variant of acute leukaemia occurring in adults, making up approximately 80–85% of cases of acute leukaemia diagnosed in individuals over 20 years of age. Currently, between 60 and 80% of young adults can achieve complete remission. The possibility of obtaining a durable complete remission decreases with age, and the chance of long-term survival in a patient more than 60 years old doesn’t exceed 30%. The French–American–British (FAB) morphological classification named the AML according to the normal marrow elements that it most closely resembled (M0–M7 and hybrid leukaemias), and was widely employed until 1998, when it was replaced by the World Health Organization (WHO) classification, which takes into account current knowledge about the diagnostic prognostic role of clonal cytogenetic and molecular aberrations.
Most patients with AML present with anaemia, thrombocytopaenia, and leukocytosis (median white blood cell count 10 000–20 000/µl). Patients with AML generally present initially with symptoms related to complications of pancytopaenia, including weakness, easy fatigability, infections of variable severity, and haemorrhagic findings such as gingival bleeding, ecchymoses, epistaxis, and menorrhagia. Combinations of these symptoms are common. Although increased resting energy expenditure has been described in paediatric and adult patients with AML, nutritional status is usually good upon diagnosis. Protein turnover is also increased.
Changes in plasma free amino acid concentration have been described in AML that only partially resemble those observed in solid tumours. In a study performed in 40 AML patients upon diagnosis, a significant increase in glutamic acid, ornithine, free tryptophan, and glycine plasma concentrations was reported, while serine, methionine, and taurine were significantly reduced with respect to control subjects. When patients were stratified according to their response to chemotherapy and their status at 18 months after chemotherapy, it was shown that taurine, its precursor serine, and methionine tended to be even lower in patients who had not responded to or had relapsed after high-dose chemotherapy. Thus, it would appear that taurine deficiency may have some relevance in the clinical outcome of AML, since it has been previously demonstrated that taurine is the most abundant intracellular free amino acid in AML, and that its plasma concentrations drop after chemotherapy, while its intracellular content correlates to the chemosensitivity of a leukaemia cell line.
Therapy for AML has traditionally been divided into stages: induction, post-remission therapy of varying intensity and duration, and post-relapse therapy.
- Induction therapy is designed to produce rapid clearing of leukaemic cells from the peripheral blood with subsequent marrow aplasia, and is achieved with combined therapy including an anthracycline in association with ara-C, causing severe mucosal damage.
- Post-remission therapy includes intensive consolidation with intermediate/high-dose cytarabine with or without anthracycline, followed in most cases by a stem-cell transplant; both allogeneic and autologous HSCT have been advocated for selected patients in first remission, depending upon the patients’ age, clinical and biological risk factors, and donor availability.
- Relapsed and refractory AML are usually treated with non-cross-resistant combining chemotherapy.
A transient reduction of energy expenditure may be induced by chemotherapy. However, fever, immunosuppression, and consequent opportunistic infections may again increase metabolic rate and protein wasting, particularly in the neutropaenic period.
Chronic myeloid leukaemia
CML is a clonal myeloproliferative disorder of a pluripotent stem cell with a specific cytogenetic abnormality, the Philadelphia (Ph) chromosome, which is responsible for the generation of a pathologic fusion protein (p210) with tyrosine-kinase activity. The proein induces a dysregulation in the control mechanisms of white blood cell proliferation and death. The first phase of the disease, the chronic phase, terminates in a second, more acute or abrupt course, called the blast phase. Symptoms and signs usually develop insidiously and include fatigue, anaemia, progressive splenomegaly, and leukocytosis. In the chronic phase, the myeloid cells in the peripheral blood show all stages of differentiation, but the myelocyte predominates. The therapeutic approach of CML has radically changed in the last 10 years. Until 2000, the best therapeutic options for young CML patients were recombinant interferon-gamma (rIFN-γ) and allogeneic stem-cell transplant; but since then the first treatment choice has become the use of tyrosine-kinase inhibitors (TKIs) (imatinib, dasatinib, nilotinib). These compounds, orally administered, target the pathologic fusion protein responsible for the proliferation and apoptosis impairment, and are capable of inducing cytogenetic remissions in a high proportion of patients. Currently the indication for stem-cell transplant in CML is limited to those patients not responding to TKI and to those in accelerated/blastic phase.
Lymphoproliferative disorders
Acute lymphocytic leukaemia
Acute lymphocytic leukaemia (ALL) makes up 80% of the acute leukaemias of childhood. The peak incidence is between 3 and 7 years of age. It also occurs in adults, causing approximately 20% of acute adult leukaemias. Adults with ALL are treated with combination chemotherapy, including daunorubicin, vincristine, prednisone, and asparaginase. This treatment produces complete remission in 80–90% of patients. After complete remission, central nervous system prophylaxis is performed.
Post-remission consolidation is achieved with variably myelosuppressive doses of cytarabine and other chemotherapeutic agents in varied combinations, while no standard approach has been devised for relapsed or refractory ALL.
High-dose chemotherapy plus bone-marrow transplantation represents a therapeutic option in selected categories of high-risk patients in first complete remission and in most patients after relapse.
Chronic lymphocytic leukaemia (CLL)
Chronic lymphocytic leukaemia (CLL) is characterised by a progressive accumulation of monoclonal B lymphocytes. During the initial asymptomatic phase, patients are able to maintain their usual lifestyle, but during the terminal phase, the performance status is poor, with recurring need for hospitalisation. The most frequent causes of death are severe systemic infections (especially pneumonia and septicaemia), bleeding, and malnutrition with cachexia.
Most cases of early CLL require no specific therapy. Standard treatment with chlorambucil is well tolerated and usually effective, and does not cause any nutritional impairment, but in young patients (<60 years) with biological features associated with a poor prognosis and a significant reduction of life expectancy with standard therapy, the indication to perform an allogeneic stem-cell transplant is increasing.
Malignant lymphoma
The malignant lymphomas are neoplastic transformations of cells that reside predominantly within lymphoid tissues. Although Hodgkin’s and non-Hodgkin’s lymphomas (NHLs) are among the most sensitive malignant neoplasms to radiation and cytotoxic therapy, their response rates are markedly different (nearly 75% for Hodgkin’s lymphomas and 35% for NHLs).
Hodgkin’s lymphoma
Hodgkin disease is a group of lymphoproliferative disorders characterised by the pathognomonic finding of Reed–Sternberg cells, with varying degrees of normal reactive and inflammatory cells and fibrosis within involved lymph nodes.
The disease has a bimodal age distribution, with one peak in the 20s and a second over age 50. Presenting symptoms include fever, weight loss, night sweats, generalised pruritus, and the occurrence of a painless mass, generally in the neck. Patients with stage I–II Hodgkin’s disease with favourable prognostic factors are candidates for radiotherapy alone or for modified radiotherapy and chemotherapy. Patients with unfavourable prognostic factors should receive chemotherapy (adriamycin, bleomycin, vincristin, and daunorubicin; ABVD) and radiotherapy as initial treatment. ABVD is also the treatment of choice in advanced disease. For patients who fail to achieve remission with primary chemotherapy, and for those who relapse after initial treatment, the best therapeutic option is autologous stem-cell transplantation. Allogeneic bone-marrow transplantation has been performed in patients with advanced Hodgkin’s disease, but results are controversial due to the high toxicity.
Non-Hodgkin’s lymphoma
NHLs are a heterogeneous group of neoplasms of lymphocytes. The pathogenesis of these disorders has been widely clarified with the aid of molecular biology. Although classification of the lymphoma is a controversial area in continuous evolution, lymphoma classification schemas are mainly based on lymph-node architecture, cytological classification of the neoplastic cells, and lymphoid cell immunophenotype (WHO classification of lymphoid neoplasms).
Unlike patients with Hodgkin’s disease, who present with weight loss, fever, or night sweats, patients with NHL generally do not present with systemic complaints, but mainly with painless peripheral lymphadenopathy.
The appropriate therapeutic regimen is strictly dependent upon the histology and extent of disease. The patient’s age and the presence of comorbid diseases also influence the treatment choice. Patients with early-stage NHL usually undergo involved field irradiation, while those with advanced-stage NHL are treated by systemic combination chemotherapy. In CD20-positive lymphomas, the use of the anti-CD20 monoclonal antibody (rituximab) in association with chemotherapy has become the standard therapeutic approach. High-dose therapy and autologous HSCT has a standard indication in patients after relapse, while during first-line treatment the indication is still controversial.
The treatment of high-grade lymphomas (such as lymphoblastic, Burkitt’s, and Burkitt’s-like lymphomas) involves the use of high-dose combined chemotherapy regimens. Disease relapse is treated by supralethal doses of chemotherapy, often in combination with radiation therapy, and syngeneic, allogeneic, or autologous stem-cell transplantation in order to circumvent myelosuppression.
Multiple myeloma
Multiple myeloma is a haematological malignancy defined by the proliferation of a single plasma-cell clone capable of producing a large amount of a specific immunoglobulin, known as ‘monoclonal component’. Main symptoms are renal impairment, anaemia, hypercalcaemia, and lytic bone lesions, which are often responsible for vertebral collapse and other bone fractures. Standard treatment for symptomatic myeloma includes antiangiogenetic agents (thalidomide) and proteasome inhibitors (bortezomib), followed, in patients younger than 65, by autologous stem-cell transplantation, which is currently the best therapeutic choice in patients responding to first-line treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree