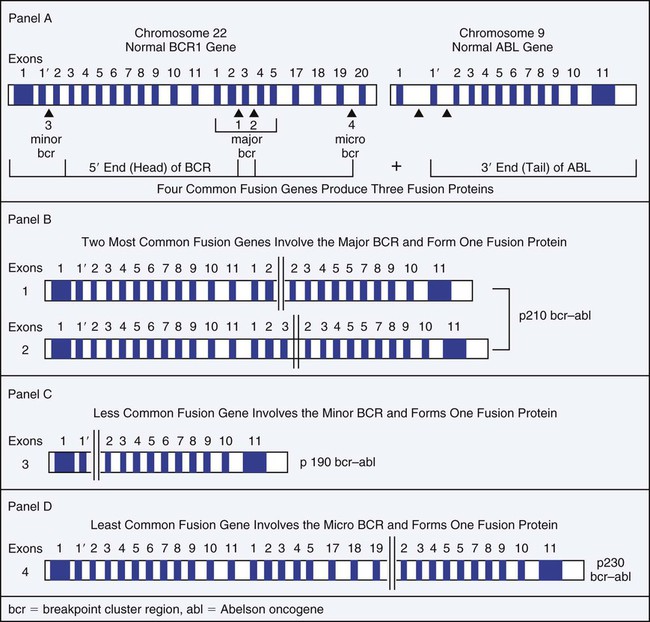
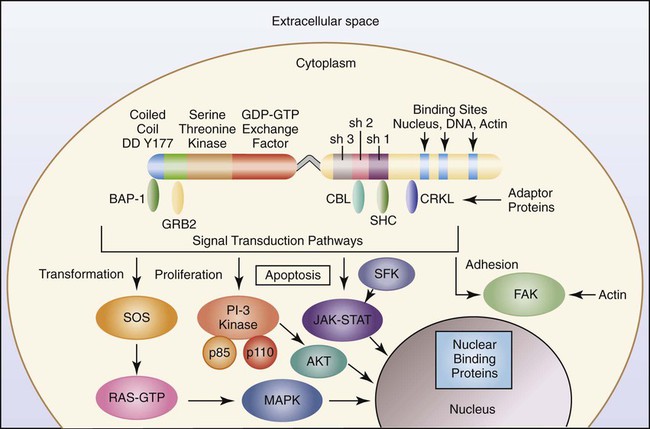
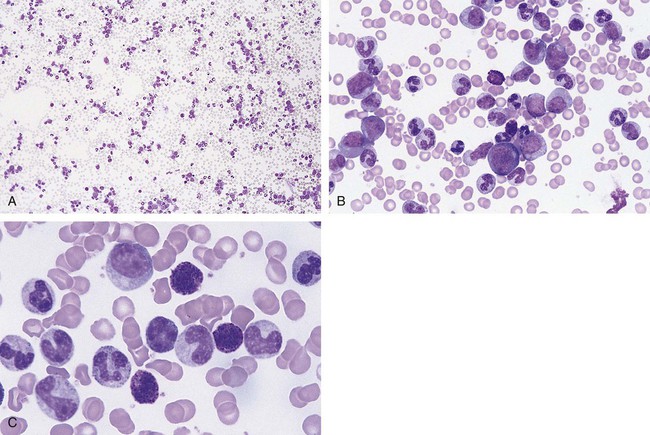
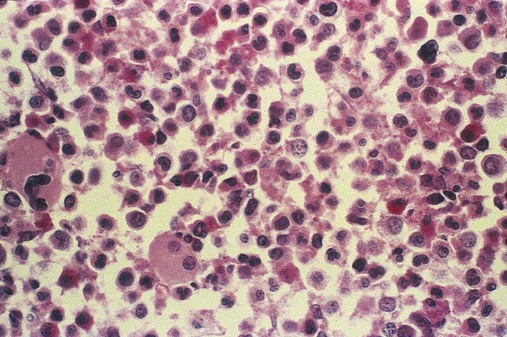
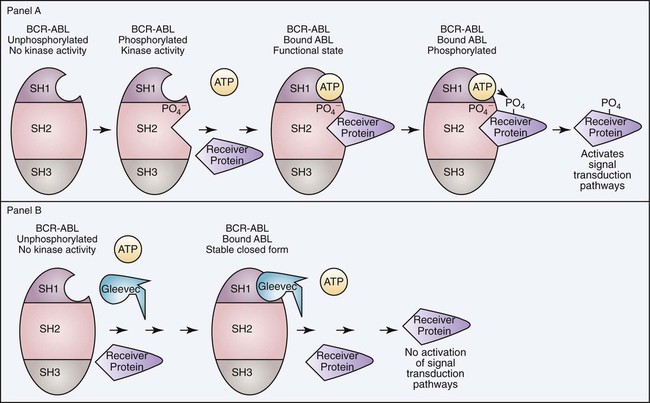
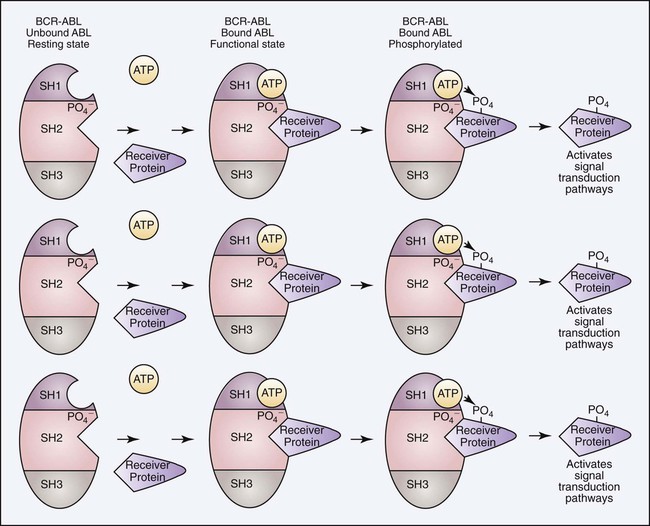
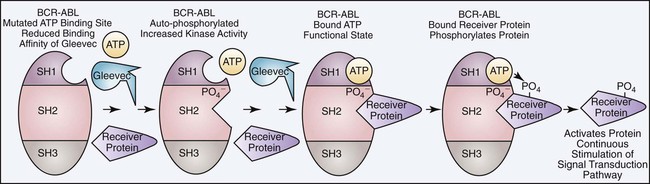
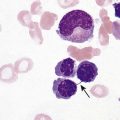
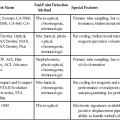
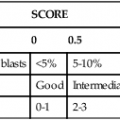
After completion of this chapter, the reader will be able to: 1. Define myeloproliferative neoplasms (MPNs). 2. List the most common diseases included in the classification of MPNs and recognize their abbreviations. 3. Define chronic myelogenous (chronic myelocytic) leukemia (CML), with emphasis on the affected cell lines. 4. Discuss the pathogenic mechanism in CML, including the cytogenetic and molecular biology. 5. Describe the peripheral blood and bone marrow findings in CML. 6. List the clinical phases of CML and describe the expected symptoms and laboratory test results in each phase. 7. Discuss the best approach to treatment and mechanisms of drug resistance. 8. Define polycythemia vera (PV), with emphasis on the affected cell lines. 9. Discuss the JAK2 mutation and the proposed pathogenic mechanism in PV. 10. Discuss clinical symptoms commonly observed in patients with PV. 11. Identify major morphologic changes in the bone marrow and peripheral blood in patients with PV. 12. List diagnostic criteria for PV. 13. Discuss the progression of PV and treatment modalities. 14. Define essential thrombocythemia (ET), with emphasis on the affected cell lines. 15. List the diagnostic criteria for ET. 16. Describe the morphologic changes in the peripheral blood in patients with ET. 17. Discuss two complications that may occur in patients with ET. 18. Define primary myelofibrosis (PMF), with emphasis on the affected cell lines and pathogenesis. 19. Describe the key pathologic features of PMF in bone marrow, peripheral blood, and tissues. 20. Describe the course of disease of PMF and current therapy. 21. Briefly describe the other myeloproliferative disorders. 22. Given complete blood count and cytogenetic, molecular, and other laboratory results, recognize the findings consistent with each major MPN. 23. Recommend follow-up testing for suspected MPN and interpret the results of testing. 24. Briefly describe the other MPNs outlined in this chapter. Leukocyte alkaline phosphatase (LAP) score—20 (reference range, 40 to 130) Lactate dehydrogenase—692 IU (reference range, 140 to 280 IU) Uric acid—8.1 mg/dL (reference range, 4 to 6 mg/dL) 1. What is the significance of the elevated WBC count and abnormal WBC differential? 2. How does the LAP score aid in the diagnosis? 3. Justify the use of cytogenetic studies in a patient with test results similar to those in this case study. 4. Predict the results of the cytogenetic studies. 5. Describe the molecular mutation resulting from the cytogenetic abnormality. 6. What is the usual treatment for this disorder? The myeloproliferative neoplasms (MPNs) are clonal hematopoietic disorders caused by genetic mutations in the hematopoietic stem cells that result in expansion, excessive production, and overaccumulation of erythrocytes, granulocytes, and platelets. Expansion occurs in varying combinations in the bone marrow, peripheral blood, and tissues.1–4 The MPNs have pathogenetic similarities as well as common clinical and laboratory features.5 The World Health Organization (WHO) has classified the MPNs as including four predominant disorders: chronic myelogenous leukemia (CML); polycythemia vera (PV) also known as polycythemia rubra vera; essential (primary) thrombocythemia (ET); and primary myelofibrosis (PMF), also known as agnogenic myelofibrosis with myeloid metaplasia and chronic idiopathic myelofibrosis. Several other less common MPN conditions have been described and are classified as chronic neutrophilic leukemia (CNL); chronic eosinophilic leukemia (CEL), not otherwise specified; mastocytosis; and myeloproliferative disorder, unclassified.6 CML and PV are defined by their overproduction of granulocytes and erythrocytes, respectively.2,7,8 PMF is a combination of overproduction of hematopoietic cells and stimulation of fibroblast production leading to ineffective hematopoiesis with resultant peripheral blood cytopenias.9 ET is characterized by increased megakaryocytopoiesis and peripheral blood thrombocytosis.10 Familial MPNs have been described in families in which two or more members are affected.11 Chronic myelogenous leukemia (CML) is an MPN arising from a single genetic translocation in a pluripotential hematopoietic stem cell producing a clonal overproduction of the myeloid cell line, which results in a preponderance of immature cells in the neutrophilic line. CML begins with a chronic clinical phase that progresses to an accelerated phase in 3 to 4 years and often terminates as an acute leukemia if left untreated. The clinical features are frequent infection, anemia, bleeding, and splenomegaly, all secondary to massive pathologic accumulations of myeloid progenitor cells in bone marrow, peripheral blood, and extramedullary tissues. Neutrophilia with all maturational stages present, basophilia, eosinophilia, and often thrombocytosis are noted in peripheral blood. The clonal origin of hematopoietic cells in CML has been verified in studies of females heterozygous for glucose-6-phosphate dehydrogenase. Only one isoenzyme is active in affected cells, whereas two isoenzymes are active in nonaffected cells.12 A unique chromosome, the Philadelphia chromosome, is present in proliferating hematopoietic stem cells and their progeny in CML and must be identified to confirm the diagnosis. Although the cause of Philadelphia chromosome formation is unknown, it appears more frequently in populations exposed to ionizing radiation.13,14 In most patients, a cause cannot be identified. Appearance of the Philadelphia chromosome in donor cells after allogeneic bone marrow transplantation indicates the possibility of a transmissible agent.15 The Philadelphia chromosome was first identified as a short chromosome 22 in 1960 by Nowell and Hungerford in Philadelphia.16 In 1973 Rowley, of the University of Illinois at Chicago, discovered that the Philadelphia chromosome is a reciprocal translocation between the long arms of chromosomes 9 and 22 (see Chapter 31).17 This acquired somatic mutation specifically reflects the translocation of an ABL proto-oncogene from band q34 of chromosome 9 to the breakpoint cluster region (BCR) of band q11 of chromosome 22, which results in a unique chimeric gene, BCR/ABL.18 This new gene produces a 210-kD BCR/ABL fusion protein (p210BCR/ABL) that expresses enhanced tyrosine kinase activity compared with its natural enzymatic counterpart. The t(9;22) translocation that produces the BCR/ABL1 chimeric gene has been observed in four primary molecular forms that produce three versions of the BCR/ABL chimeric protein: p190, p210, and p230 (Figure 34-1). The four genetic variations are based on the area of the BCR gene that houses the breakpoint on chromosome 22, because the breakpoint on chromosome 9 occurs in the same location. The wild-type (normal) ABL1 gene on chromosome 9 is a relatively large gene of approximately 230 kilobases (kb) containing 11 exons. The breakpoint consistently occurs 5′ of the second exon such that exons 2 to 11 are contributed to the BCR/ABL1 fusion gene. There are four BCR genes in the human genome: BCR1, BCR2, BCR3, and BCR4. It is the BCR1 gene that is involved in the Philadelphia translocation. Wild-type (normal) BCR1 gene is approximately 100 kb with 20 exons. In 1984 Groffen et al identified the BCR on chromosome 22 as a 5-exon region involving exons 12 to 16 that was the area of breakage in the traditional t(9;22) translocation.19 This area was later termed the major BCR. Two other areas of breakage were identified on chromosome 22, one nearer the 5′ (head) of the BCR1 gene, called the minor BCR, and one in the 3′ end (tail) of the BCR1 gene termed the micro BCR. Within the major BCR two specific breakpoints account for the t(9;22) translocation involved in the development of CML. Therefore, two areas of breakage in the major BCR combined with one in the minor BCR and one in the micro BCR produce the four versions of the BCR/ABL1 chimeric gene. Because the two breakpoints in the major BCR differ by only one exon, the chimeric protein product is essentially the same size and is designated as the p210 protein. Breakage in the BCR1 gene in the major BCR contributes exons 1 to 13 or 1 to 14, whereas the ABL1 gene contributes exons 2 to 11. Breakage in the minor BCR contributes only exon one from BCR, which joins with the same exons 2 to 11 of ABL1 to produce a p190 protein. The micro BCR breakpoint contributes exons 2 to 19 from BCR1, which fuse with ABL1 exons 2 to 11, producing the p230 protein. Therefore, the four possible BCR1 breakpoints produce four different chimeric genes, resulting in a total of three different protein products.20 To understand the aberrant function of the BCR/ABL fusion protein, it is first helpful to understand both the normal BCR and ABL proteins. The wild-type ABL protein, when in its usual location on chromosome 9, codes for p125, which exhibits normal tyrosine kinase activity. The BCR1 gene produces p160, expresses serine and threonine kinase activity, and is thought to function in the regulation of cell growth. Protein kinases are enzymes that catalyze the transfer of phosphate groups from adenosine triphosphate (ATP), guanosine triphosphate, and other phosphate donors to receiver proteins. A tyrosine kinase transfers the phosphate group to a tyrosine amino acid on the receiver protein. For the kinase activity of the ABL protein to occur, the ABL protein must first be phosphorylated. This is often accomplished through autophosphorylation. The ABL protein has three primary domains called SR1, SR2, and SR3 that together express and regulate the kinase activity. SR1 is the binding site for ATP; SR2 is the docking point for phosphate receiver proteins; and SR3 is the domain that controls the phosphorylation activity. When ATP binds to the ATP binding site, the phosphate is transferred to the SR2 region of the ABL protein, which initiates a conformational change that alters the tertiary structure of the protein and exposes the active site of the enzyme. When a second ATP binds the ATP binding site and a receiver protein docks in the SR2 domain, the phosphate group is transferred to the receiver protein. In most physiologically normal intracellular pathways, protein phosphorylation activates the receiver proteins (Figure 34-2). This phosphorylation initiates a cascade of phosphorylation events, each activating the next protein until a transcription factor becomes activated. These activation cascades, called signal transduction pathways, are designed to activate genes necessary to control cell proliferation, differentiation, and natural cell death, called apoptosis. There are several signal transduction pathways activated by the ABL tyrosine kinase that function in concert to activate these genes in a precise order and at the required level of activation to control these cellular events.20,21 In the case of CML, the BCR/ABL1 translocation occurs next to the SR3 domain of the ABL1 moiety, which is designed to control the rate and timing of phosphorylation. Therefore, the BCR/ABL tyrosine kinase has lost the ability to shut off kinase activity and is said to have constitutive tyrosine kinase activity. The BCR/ABL enzyme continuously adds phosphate groups to tyrosine residues on cytoplasmic proteins, activating several signal transduction pathways. These pathways stimulate gene expression keeping the myeloid cells proliferating, reducing differentiation, reducing adhesion of cells to bone marrow stroma, and virtually eliminating apoptosis. The result is increased clonal proliferation of myeloid cells secondary to a reduction in or loss of sensitivity to protein regulators.22 There is an increase in growth factor–independent cellular proliferation from activation of the RAS gene and a decrease in or resistance to apoptosis. New clones of stem cells vulnerable to additional genetic changes lead to the accelerated and blast phases of CML. In addition, the BCR/ABL protein localizes in the cytoplasm, rather than in the nucleus as does the normal ABL protein. The mutation affects maturation and differentiation of hematopoietic and lymphopoietic cells, whose progeny eventually dominate in the affected individual. Progeny cells that exhibit this chromosome include neutrophils, eosinophils, basophils, monocytes, nucleated erythrocytes, megakaryocytes, and B lymphocytes.7,23 In addition, the loss of genetic segments in the 5′ end of the ABL1 gene results in an altered protein-binding affinity for F-actin, which leads to a reduction in contact binding of hematopoietic CML cells to stromal cells and causing premature release of cells into the circulation.21 Abnormal adhesion between stem cells and stroma may dysregulate hematopoiesis. One action of interferon-α therapy is to reverse the loss of adhesion of CML progenitor cells, which reduces the premature release of these cells into the circulation.24 There are dramatic morphologic changes in the peripheral blood and bone marrow that reflect the expansion of the granulocyte pool, particularly in the later maturational stages. Table 34-1 lists the qualitative changes in the peripheral blood, bone marrow, and extramedullary tissues that are commonly observed at the time of diagnosis. A dramatic left shift is noted that extends down to the promyelocyte stage and occasionally even produces a few blasts in the peripheral blood. The platelet count is often elevated, reflecting the myeloproliferative nature of the disease. Extramedullary granulopoiesis may involve sinusoids and medullary cords in the spleen and sinusoids, portal tract zones, and solid areas of the liver. TABLE 34-1 Common Morphologic Changes in Chronic Myelogenous Leukemia Figure 34-3 illustrates a common pattern in the peripheral blood film of chronic phase CML at the time of diagnosis. Leukocytosis is readily apparent at scanning microscopic powers. Segmented neutrophils, bands, metamyelocytes, and myelocytes predominate, and immature and mature eosinophils and basophils are increased. Myeloblasts and promyelocytes are present at a rate of approximately 1% and 5%, respectively. Lymphocytes and monocytes are present and often show an absolute increase in number but a relative decrease in percentage. Nucleated red blood cells (NRBCs) are rare. Platelets are normal or increased, and some may exhibit abnormal morphology. Bone marrow changes are illustrated in Figure 34-4. An intense hypercellularity is present due to granulopoiesis, marked by broad zones of immature granulocytes, usually perivascular or periosteal, differentiating into more centrally placed mature granulocytes. Normoblasts appear reduced in number. Megakaryocytes are normal or increased in number and, when increased, may appear in clusters and exhibit dyspoietic cytologic changes. They often appear small with reduced nuclear size (by approximately 20%) and reduced nuclear lobulations. Reticulin fibers are increased in approximately 20% of patients. Increased megakaryocyte density is associated with an increase in myelofibrosis.25 The presence of pseudo-Gaucher cells (see Chapter 28) usually occurs. Hyperuricemia and uricosuria from increased cell turnover may be associated with secondary gout, urinary uric acid stones, and uric acid nephropathy.26 Approximately 15% of patients exhibit total white blood cell (WBC) counts greater than 300 × 109/L.27 Symptoms in these patients are secondary to vascular stasis and possible intravascular consumption of oxygen by the leukocytes. Symptoms are reversible with the lowering of the total WBC count.28 In the pre-imatinib era, most patients’ disease would eventually transform into acute leukemia.29 Before blastic transformation, some patients proceed through an intermediate metamorphosis or accelerated phase. Disease progression is accompanied by an increase in the frequency and number of clinical symptoms, adverse changes in laboratory values, and poorer response to therapy than in the chronic phase. Additional chromosome abnormalities may appear, associated with enhanced dyshematopoietic cell maturation patterns and increases in morphologic and functional abnormalities in blood cells. There is often an increasing degree of anemia and, in the peripheral blood, fewer mature leukocytes, more basophils, and fewer platelets, with a greater proportion of abnormal platelets, micromegakaryocytes, and megakaryocytic fragments. The circulating blast count increases to 10% to 19%. This total blast percentage, or a combination of 20% blasts and promyelocytes, has been proposed as a diagnostic criterion for the accelerated phase.30 Blast crisis involves the peripheral blood, bone marrow, and extramedullary tissues. By definition, blasts constitute more than 20% of total bone marrow cellularity; the peripheral blood exhibits increased blasts.29 Blast crisis leukemia usually is AML or ALL, but origins from other hematopoietic clonal cells are possible. Extramedullary growth may occur as lymphocytic or myelogenous cell proliferations; the latter are often referred to as granulocytic sarcoma. Extramedullary sarcoma is observed at many sites or locations in the body and may precede a marrow blast crisis. The clinical symptoms of blast crisis mimic those of acute leukemia, including severe anemia, leukopenia of all WBCs except blasts, and thrombocytopenia. Chromosome abnormalities such as additional Philadelphia chromosome(s), isochromosome 17, trisomy 8, loss of Y chromosome, and trisomy 19 accumulate with disease progression.31,32 These generally occurred in approximately 75% of patients in the pre-imatinib era. Several diseases exist that are clinically similar to CML but do not exhibit the Philadelphia chromosome and express only a few pseudo-Gaucher cells. Chronic neutrophilic leukemia is another MPN that manifests with peripheral blood, bone marrow, and extramedullary infiltrative patterns similar to those of CML, except that only neutrophilic granulocytes are present and fewer than 10% of peripheral blood neutrophils are immature.33 Similarly, chronic monocytic leukemia involves a comparable expansion of monocytes, including functional monocytes.34 Juvenile myelomonocytic leukemia and adult chronic myelomonocytic leukemia are classified by the WHO as myelodysplastic/myeloproliferative diseases because of the overlap in clinical, laboratory, or morphologic findings. Juvenile myelomonocytic leukemia is observed in children younger than 4 years of age and is accompanied by an expansion in the number of monocytes and granulocytes, including immature granulocytes, and manifestations of dyserythropoiesis.35 The peripheral blood of adults with chronic myelomonocytic leukemia may have characteristics similar to those seen in the refractory anemias, such as oval macrocytes and reticulocytopenia. The peripheral WBC concentration may reach 100 × 109/L. According to WHO criteria, absolute monocytosis (more than 1 × 109 monocytes/L) must be present to make the diagnosis. Clinical features include prominent splenomegaly, symptoms of anemia, fever, bleeding, and infection. Before presence of the Philadelphia chromosome was established as a requirement for the diagnosis of CML, some cases that were classified as Philadelphia chromosome–negative CML likely represented misdiagnoses of chronic myelomonocytic leukemia.36 Chronic myelomonocytic leukemia is discussed further with myelodysplastic syndromes in Chapter 35. A puzzling group of patients exhibit Philadelphia chromosome–positive acute leukemia. Studies reveal that 2% of patients with AML exhibit Philadelphia chromosome in a significant proportion of blasts. Further, 5% of patients with childhood-onset ALL and 20% of those with adult-onset ALL test positive for Philadelphia chromosome.37–40 The proper alignment of these cases within the spectrum of CML is speculative. It is understood that some of these cases likely represent undiagnosed CML that rapidly progressed to an acute leukemia prior to diagnosis. However, because rapidly dividing malignant cells are more prone to genetic mutation, the presence of the Philadelphia chromosome in acute leukemias may reflect a late-stage mutation that contributed little to acute leukemia leukemogenesis. Early treatment approaches for CML were unable to produce remission, so the goal of therapy became the reduction of tumor burden. The first forms of therapy for CML included alkylating agents such as nitrogen mustard,41 introduced in the late 1940s, and busulfan,42 which came into use in the early 1950s. Later, busulfan in combination with 6-thioguanine was used to achieve the goal of tumor burden reduction. Other drugs like hydroxyurea and 6-mercaptopurine were introduced later and found to improve patient survival. The discovery of interferon-α in 1983 dramatically improved outcomes of patients with CML by inducing the suppression of the Philadelphia chromosome, reducing the rate of cellular progression to blast cells, and increasing the frequency of long-term patient survival.43 Interferon-α stimulates a cell-mediated antitumor host response that reduces myeloid cell numbers, induces cytogenetic remissions, and increases survival.44 It improves the frequency and duration of hematologic remission and reduces the frequency of detection of the Philadelphia chromosome. In some patients, a complete cytogenetic remission is achieved for a time. In 1997 it was discovered that cytarabine given with interferon-α improved the frequency of hematologic remissions but did not eliminate the BCR/ABL gene, which was still detected by molecular and fluorescent methods.45 Also, in some patients the side effects of therapy became severe, drug resistance appeared, and relapse rates were not improved compared with other chemotherapies. Bone marrow and stem cell transplantation with either autologous or allogeneic hematopoietic stem cells have been reported as curative, especially in patients younger than age 55. Relapses occur, but long-term, disease-free survival is possible. Optimal survival occurs when the patient is treated during the chronic phase within 1 year of diagnosis and is younger than age 50. Treatment requires ablative chemotherapy followed by transplantation of mobilized normal progenitor cells that exhibit CD34+ surface markers. Allogeneic bone marrow transplants are more successful in patients up to age 55 when donors are matched for HLA antigens A, B, and DR. Donor-matched lymphocyte infusions after allogeneic transplantation of marrow from a sibling donor may assist in producing complete remissions.46 Modern therapies involve the use of synthetic proteins that bind the abnormal BCR/ABL protein, blocking the constitutive tyrosine kinase activity and reducing signal transduction activation. Imatinib mesylate is a synthetic tyrosine kinase inhibitor designed to selectively bind the ATP binding site and thus inhibit the tyrosine kinase activity of the BCR/ABL fusion protein. When imatinib binds the ATP binding site, ATP is unable to bind to provide the phosphate group necessary for kinase activity. Imatinib binds the BCR/ABL protein in the inactive conformation, which precedes the autophosphorylation necessary to generate the kinase active site (Figure 34-5).47 Goals of therapy include complete hematologic remission and cytogenetic remission induced in part by the reactivation of apoptotic pathways.48 The effectiveness of imatinib therapy and stem cell transplantation is best monitored using quantitative real-time reverse transcriptase polymerase chain reaction (RT-PCR). These monitoring tools are used to determine complete cytogenetic and molecular remission. The most sensitive measure of the effectiveness of imatinib therapy is the number of log reductions of BCR/ABL transcripts using real-time RT-PCR.49 Expected therapeutic response to imatinib is complete hematologic remission in 3 to 6 months, complete cytogenetic response in 6 months to 1 year, and a 2 to 3 log reduction in BCR/ABL transcripts. When real-time RT-PCR is used, the greatest log reduction possible is a more than 4 log reduction, which represents the maximum sensitivity of the assay. However, discontinuation of imatinib therapy in patients who achieve a more than 4 log reduction will result in relapse. Although imatinib has proven to be a successful form of therapy, a major limitation is the development of imatinib resistance resulting in relapse. Approximately 4% of patients with newly diagnosed CML will become imatinib resistant. There are two major categories of imatinib resistance, primary and secondary. Primary resistance is defined as the inability to reach the remission milestones. This form of resistance is rare and probably results from the presence of mutations other than the BCR/ABL mutation at the time of diagnosis. Secondary resistance involves the loss of a previous response and occurs at a rate of 16% at 42 months. The majority of cases of imatinib resistance result from two primary causes: acquisition of additional BCR/ABL mutations and expression of point mutations in the ATP binding site. Additional BCR/ABL mutations can occur through the usual translocation of the remaining unaffected chromosomes 9 and 22, which converts the hematopoietic stem cell from heterozygous to homozygous for the BCR/ABL mutation. A double dose of BCR/ABL can also be acquired from gene duplication during mitosis and accounts for 10% of secondary mutations. An additional BCR/ABL mutation will double the tyrosine kinase activity, making the imatinib dosage inadequate. In these cases higher dosages of imatinib will restore remission in most patients (Figure 34-6). The majority of patients who do not respond to higher dosages of imatinib express point mutations in the ATP binding site. Over 50 mutations have been identified in the ATP binding site, and these account for the remaining 50% to 90% of secondary mutations. Mutations in the ATP binding site reduce the binding affinity of imatinib, producing some level of resistance (Figure 34-7). Second- and third-generation tyrosine kinase inhibitors like dasatinib (Sprycel), nilotinib (Dasigna), and bosutinib (still in clinical trials at the time of publication) overcome the ATP binding site mutations except the T315I mutation. However, drugs designed to bind the A loop (receiver protein binding site) will inhibit tyrosine kinase activity and overcome the T315I mutation.50,51 Currently, studies are under way to evaluate modification of the dosage of imatinib used, to identify and develop other tyrosine kinase inhibitors, and to discover new classes of inhibitors that may be more effective than currently known tyrosine kinase inhibitors. The development of a care plan for treating a patient with newly diagnosed CML requires not only the formulation of alternative approaches to achieve complete cellular remission, but also the establishment of parameters to follow that confirm long-term success of therapy. Previous chemotherapies have provided cellular remission but usually do not suppress or delay clinical transitions to accelerated or blast phases. Bone marrow transplantation for patients who qualify is likely the preferred choice, but the long-term success (cure) rate remains at 50% to 70%. For a patient to qualify for transplantation, the patient must be younger than 50 years of age, must be in the first year of the disease, and must have CML that is still in the chronic phase, and a histocompatible donor must be available. Today, imatinib is considered first-line therapy for all patients with newly diagnosed CML. For the small subset of patients who qualify for hematopoietic stem cell transplantation, imatinib is used to induce hematologic remission prior to transplantation. For all other CML patients, imatinib is used as first-line therapy unless remission is not achieved (primary resistance) or until relapse occurs following remission (secondary resistance). Once the cause of relapse has been determined by cytogenetic and molecular testing, either a higher dosage of imatinib can be given (for an additional BCR/ABL mutation) or a second- or third-generation tyrosine kinase inhibitor (dasatinib, nilotinib, bosatinib) can be prescribed unless the mutation is the T315I mutation in the ATP binding site. If the T315I mutation is detected, the patient can be given an A-loop inhibitor (ONO12380) or other drugs like MK 0457 or BIRB-796 that inhibit the T315I mutation.51 Polycythemia vera (PV) is a neoplastic clonal myeloproliferative disorder that commonly manifests with panmyelosis in the bone marrow and increases in erythrocytes, granulocytes, and platelets in the peripheral blood.2 Splenomegaly is common. The disease arises in a hematopoietic stem cell. The hypothesis of a clonal origin for PV is supported by studies of X-linked restriction fragment length deoxyribonucleic acid (DNA) polymorphisms that demonstrate monoclonal X chromosome inactivation in all blood cells.52
Myeloproliferative Neoplasms
Case Study
Chronic Myelogenous Leukemia
Cytogenetics of the Philadelphia Chromosome
Molecular Genetics
Pathogenetic Mechanism
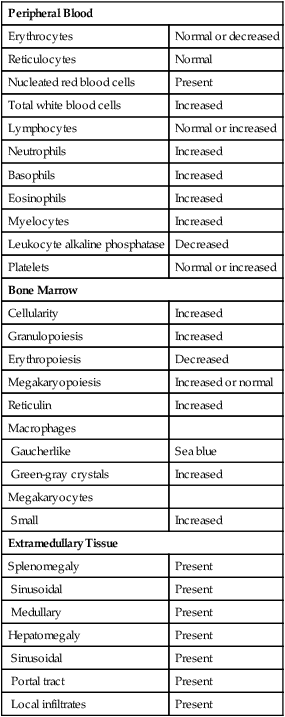
Peripheral Blood and Bone Marrow
Peripheral Blood
Erythrocytes
Normal or decreased
Reticulocytes
Normal
Nucleated red blood cells
Present
Total white blood cells
Increased
Lymphocytes
Normal or increased
Neutrophils
Increased
Basophils
Increased
Eosinophils
Increased
Myelocytes
Increased
Leukocyte alkaline phosphatase
Decreased
Platelets
Normal or increased
Bone Marrow
Cellularity
Increased
Granulopoiesis
Increased
Erythropoiesis
Decreased
Megakaryopoiesis
Increased or normal
Reticulin
Increased
Macrophages
Gaucherlike
Sea blue
Green-gray crystals
Increased
Megakaryocytes
Small
Increased
Extramedullary Tissue
Splenomegaly
Present
Sinusoidal
Present
Medullary
Present
Hepatomegaly
Present
Sinusoidal
Present
Portal tract
Present
Local infiltrates
Present
Other Laboratory Findings
Progression
Related Diseases
Treatment
Polycythemia Vera
Myeloproliferative Neoplasms