Introduction
- ■
Oral and esophageal mucosal injuries are inevitable postradiation changes, encountered with daily radiation therapy. Mucositis has remained a morbid side effect of radiation therapy since its first clinical use as an agent effective against cancer. Mucosal injury is generally the first change that is observed as the radiation beam enters human tissues. Alimentary mucositis (AM) is the recommended term to describe cancer therapy–associated mucosal injury of the alimentary tract (mouth to anus). This unifying term acknowledges the similarities along the entire gastrointestinal (GI) tract while allowing for regional differences that require discussion of oral and GI mucositis separately at times, based on pathophysiological responses, clinical characteristics, and management options. In almost all patients, AM is associated with considerable pain and thus can significantly impair quality of life and, in neutropenic patients, mucositis represents a clinically significant risk factor for sepsis. Furthermore, in some patients, AM becomes a dose‐limiting toxicity, slowing or preventing continuation of selected cancer therapies, including accelerated fractionation and hyperfractionation in radiotherapy and interventions that combine chemotherapy and radiotherapy.
- ■
The major determinants of mucosal injury are total dose of radiation, daily radiation dose, and concurrent chemotherapy, in addition to an individual’s inherent sensitivity to radiation. The incidence of AM is governed by these previously mentioned factors. Lower grade reactions are extremely common in nearly all patients receiving radiation with an incidence of almost 80% to 100%, with almost a third of these patients experiencing severe mucosal injury. ,
Description
- ■
Clinically, mucositis usually begins with mucosal congestion and erythema, which progresses through white, elevated, desquamative patches that are painful to contact pressure. Following this, the patches may coalesce and, eventually, there is development of painful, contiguous, pseudomembranous lesions ( Fig. 26.1 ) with associated dysphagia and decreased oral intake. The nonkeratinized mucosa in the oral cavity and GI tract is at the highest risk of being affected by the radiation-related reaction. Mucosal lesions usually heal within 2 to 3 weeks. The clinical course of AM may sometimes be complicated by local infection, particularly in immunosuppressed patients. Fungal infections such as candidiasis, and viral infections, such as herpes simplex virus (HSV) can sometimes be superimposed on oral mucositis, complicating its course by delaying healing.
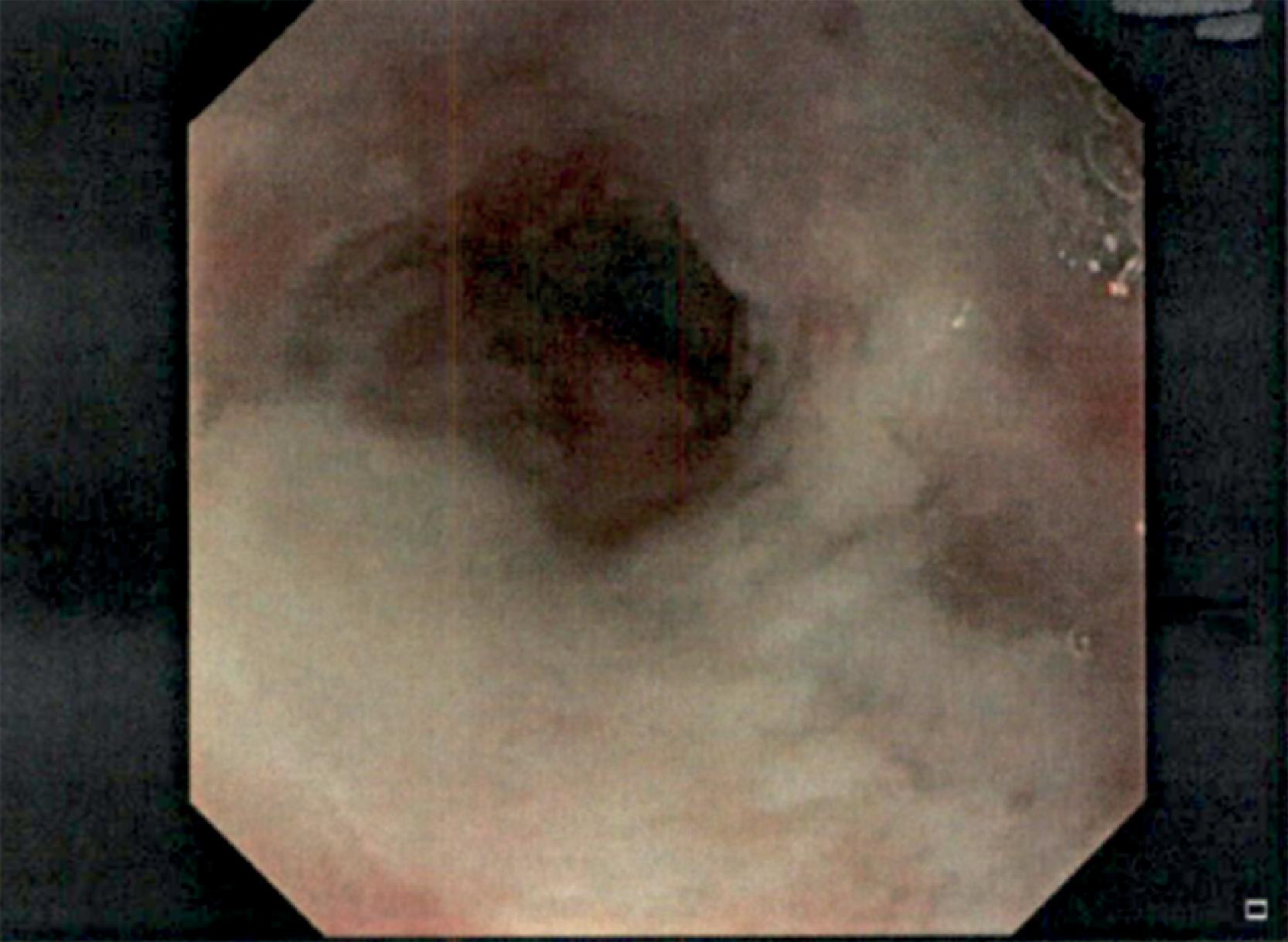
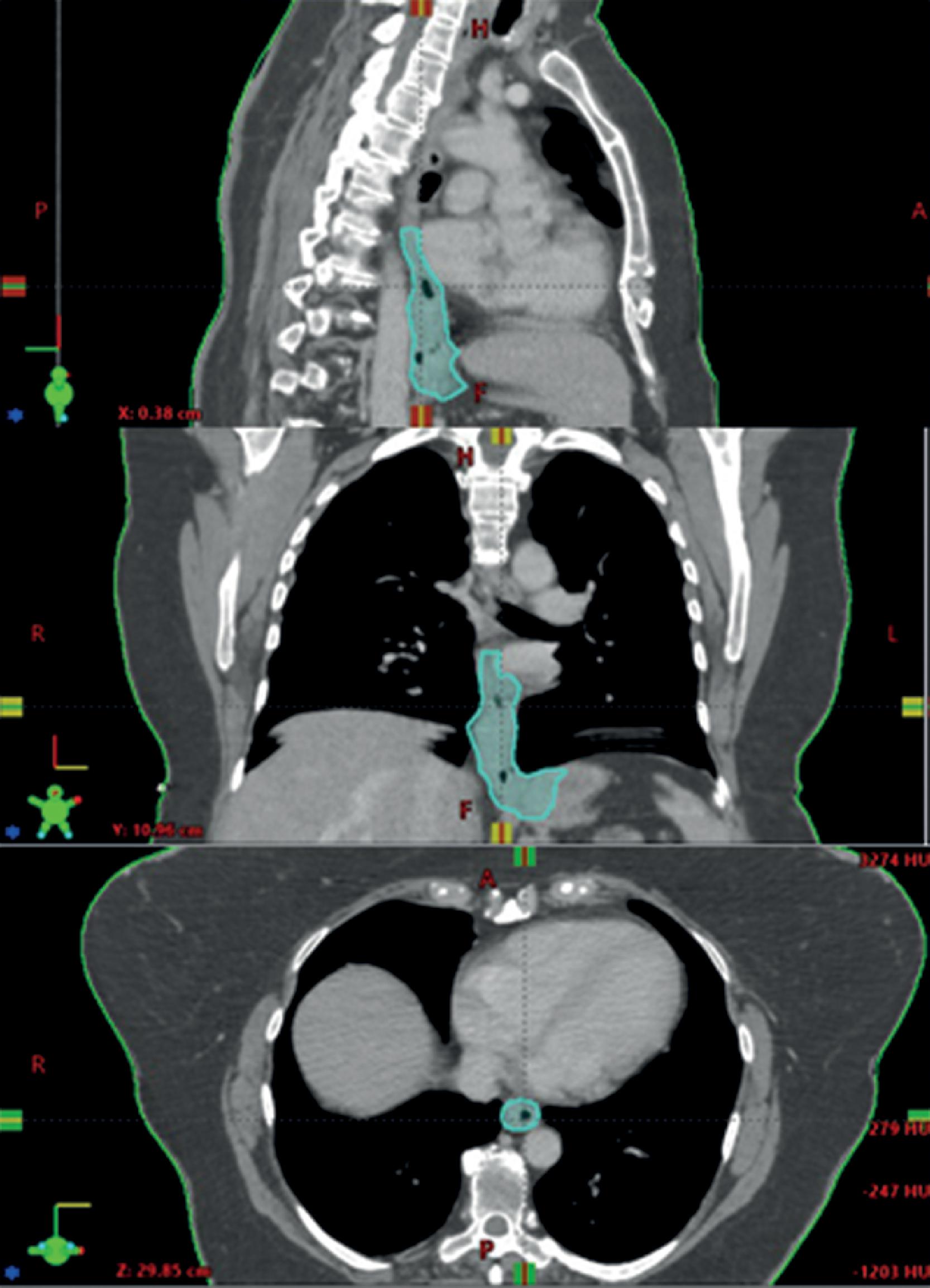
Fig. 26.1
Radiation esophagitis with confluent ulceration.
- ■
The sequence of events that occurs during radiation therapy for head and neck cancer reflects the different kinetics of the cell populations involved :
- ■
Week 1: The first week is characterized by slight focal hyperemia and edema caused by dilatation of capillaries in sensitive patients. Sensitivity may be associated with alcohol or tobacco use, chemotherapy, infection (oral candidiasis, HSV), or immunosuppression (such as HIV).
- ■
Week 2: The second week is characterized by increasing pain and loss of desire to eat. Sense of taste is altered; bitter and acid flavors are most changed, with less change with salty and sweet tastes. Erythema and edema increase, and early desquamative mucositis occurs. Basal cell division has been affected; this layer is being denuded, and vasculoconnective tissue damage becomes apparent. Mucositis is patchy during this time.
- ■
Week 3: The third week is characterized by mucositis and swelling with depletion of gland secretions leading to difficulty in swallowing. Mucositis plaques are confluent. Impairment of taste acuity occurs during the third week of a multifraction radiotherapy regime.
- ■
Week 4: The fourth week is characterized by further progression of signs previously seen signs. Confluent mucositis sloughs, resulting in denuded lamina propria. Mucosa becomes covered by fibrin and polymorphonuclear leukocytes.
- ■
Week 5: Maximal radiation damage becomes apparent by the fifth week. There is extreme sensitivity to touch, temperature, and grainy food. Recovery of epithelial layer may begin during therapy.
- ■
Posttherapy : After therapy concludes basal cells migrate into the area and proliferate. In 2 to 4 weeks, complete resolution is observed.
- ■
- ■
Defining the epidemiology of mucositis has been confounded historically by a number of variables, including underreporting, differences in terminology used to describe it, differences in assessment techniques and scales, and the correlation between mucositis and other clinically important sequelae. Multiple scoring systems for AM have been devised over the years with the goal of providing a uniform system which is objective, validated, and reproducible across all clinical situations and applications. The two most commonly used scoring systems in the field of radiation oncology include the ones formulated by the National Cancer Institute (Common Terminology Criteria for Adverse Events – CTCAE), and the Radiation Therapy Oncology Group (RTOG) scales for the purpose of uniform reporting throughout the globe. , Regardless of the scale used, increasing evidence confirms the importance of training and standardization for improving the accuracy and consistency of mucositis assessment.
- ■
The RTOG and NCI–CTCAE scoring systems for mucositis and esophagitis, are given in Tables 26.1 and 26.2 .
TABLE 26.1
RTOG and NCI–CTCAE Scoring System for Mucositis
Source
Grade 1
Grade 2
Grade 3
Grade 4
Grade 5
RTOG
May experience mild pain not requiring analgesic
Patchy mucositis may have a serosanguinous discharge. May experience pain requiring analgesics, <1.5 cm, noncontiguous
Confluent fibrinous mucositis/may include severe pain requiring narcotics, >1.5 cm, contiguous
Necrosis or deep ulceration, ± bleeding
Death
NCI–CTCAE
Painless ulcers, erythema or mild soreness
Painful erythema, edema or ulcers, but can eat
Painful erythema, edema or ulcers cannot eat
Requires parenteral or enteral support
Death
NCI–CTCAE, National Cancer Institute–Common Terminology Criteria for Adverse Events; RTOG, Radiation Therapy Oncology Group.
TABLE 26.2
RTOG and NCI–CTCAE Scoring System for Esophagitis
Source
Grade 1
Grade 2
Grade 3
Grade 4
Grade 5
RTOG
Mild dysphagia or odynophagia,topical anesthetics or NSAIDs, soft diet
Moderate dysphagia or odynophagia, narcotic analgesics, puree or liquid diet
Severe dysphagia or odynophagia, dehydration or weight loss >15%,
IV fluids, NGT, TPN
Complete obstruction, ulceration, perforation, fistula
Death
NCI–CTCAE
Asymptomatic
Symptomatic, altered eating/swallowing;
IV fluids <24 h
Symptomatic, inadequate oral caloric/fluid intake, need IV fluids >24 h, TPN
Life-threatening (obstruction, perforation)
Death
NCI–CTCAE, National Cancer Institute–Common Terminology Criteria for Adverse Events; NGT, nasogastric tube; NSAID, nonsteroidal antiinflammatory drug; RTOG, Radiation Therapy Oncology Group; TPN, total parenteral nutrition.
Risk Factors
- ■
As mentioned previously, there are certain risk factors directly associated with the incidence and severity of mucositis, which can be categorized as treatment- or patient-related. Treatment-related risk factors include the type of ionizing radiation, the volume of irradiated tissue, the dose per day, and cumulative dose. Lower energy radiation used for head and neck cancer results in higher surface dose compared with the higher energy radiation used for deeply situated tumors at other sites. The higher radiation doses needed for head and neck cancer, in the order of over 5000 cGy has been directly responsible for causing mucosal injury. , Any altered fractionation with dose fractions above 200 cGy or more than one fraction of radiation a day can also increase the risk of mucosal toxicity. It has been noted in a considerable number of clinical trials that the severity of acute normal tissue responses, particularly oral mucositis, is significantly increased when the overall treatment time is shortened. It is important to note that the incidence and severity of acute mucosal toxicity has not been significantly decreased by the introduction of newer techniques in radiation therapy. Using a different modality, such as proton therapy for head and neck radiation, has also not resulted in any significant mucosal sparing or decreased mucosal toxicity so far. Additional treatment in the form of concurrent chemotherapy is also a significant contributor to acute mucositis.
- ■
Patient-related factors play an equally important role when it comes to increased risk of mucosal injury. Any genetic changes that cause DNA repair deficiencies can inherently predispose the carrier to radiation sensitivity. There are reports of serious grade 5 toxicity with primarily homozygotes with DNA repair disorders, such as ataxia-telangiectasia (A-T), Nijmegen breakage syndrome (NBS), and Fanconi’s anemia (FA) being the most common ones. There is a high suspicion of a larger number of likely heterozygotes of these same disorders which have a higher risk of developing radiation-related toxicity due to their radiosensitivity. There appear to be additional risk factors (e.g., genetic polymorphisms) in some cohorts that account for the degree of clinical expression of mucosal injury. Further study of these more recently defined factors will likely strategically advance the pathobiological model in relation to clinical expression of the toxicity. Among other more common patient-related risk factors, comorbidities (e.g., malnutrition) can contribute important risk. Smoking is another important factor that can lead to both increasing the risk of mucosal toxicity and delaying its healing. In addition, patients who develop clinically significant salivary hypofunction/xerostomia due to head and neck radiation and/or antiemetic drugs may experience increased discomfort from oral mucositis.
Mechanism of Action
- ■
Mucositis has been known from the very beginning of the use of radiation in the treatment of cancer. However, the biological complexities underlying mucosal barrier injury have only recently been appreciated. Historically, mucositis was viewed solely as an epithelium‐mediated event due to radiation toxicity on dividing epithelial stem cells. The epithelial surface of the alimentary tract has a rapid turnover rate, predisposing it to be at a high risk of injury from ionizing radiation. It was previously believed that radiation resulted in direct damage to the basal epithelial cell layer leading to the loss of the reproductive capacity of the epithelium, further resulting in clonogenic cell death, atrophy, and consequent ulceration. However, there have been more recent findings confirming the involvement of submucosal cells and the extracellular matrix, which is not explained by the simpler previous theory of epithelial damage alone. Continued experimental evidence supports the involvement of virtually all of the cells and tissues of the oral mucosa, including the extracellular matrix, in barrier injury. There is evidence of microvascular endothelial and connective tissue damage which seems to precede epithelial changes. , There is also evidence of decreased incidence of mucosal toxicity with inhibition of platelet aggregation which supports the involvement of endothelial cells and platelets in radiation-induced mucositis. The sequence of cell and tissue changes further implies that nothing occurs within the mucosa as a biologically isolated event. Rather, it appears that interactions among the various mucosal components, including those influenced by the oral environment, collectively lead to mucositis. There is also evidence of increased proinflammatory cytokines with anticancer treatment leading to increased mucosal toxicity in animal and human studies. , There is evidence of similar pathogenesis for both oral mucositis and esophagitis, with direct damage to dividing cells, apart from decrease in the proliferative capacity of connective tissue cells within the lamina propria, leading to increased vascular permeability and an inflammatory infiltrate and causing tissue ischemia along with fibrosis.
- ■
From a radiobiology standpoint, the initiating event for radiation-induced mucosal injury is direct DNA damage to basal epithelial cells and cells in the underlying tissue. Radiation causes DNA-strand breaks as well as non–DNA injury initiated through a variety of mechanisms, most commonly with reactive oxygen species (ROS). Several injury-producing pathways involving multiple transcription factors are activated which leads to the upregulation of genes that modulate the damage response. Of the transcription factors that may be significant, nuclear factor‐κB (NF‐κB) has many of the characteristics that suggest that it may be a key element in the genesis of mucositis. NF‐κB is activated by either radiotherapy or chemotherapy, is detectable in stressed mucosa, and can respond differently to varying challenges. Once activated, NF‐κB leads to the upregulation of many genes, including those that result in the production of the proinflammatory cytokines tumor necrosis factor‐α (TNF‐α), interleukin (IL)‐1β, and IL‐6, with the potential to elicit a broad range of tissue responses, including apoptosis. Agents known to attenuate the expression of both these cytokines have demonstrated efficacy in the prevention of both experimental and clinical mucositis. These signaling molecules also participate in a positive-feedback loop that amplifies the original effects of radiation. There is synchronous direct and indirect damage to epithelial stem cells which result in a loss of renewal capacity. Acute mucositis results from the loss of squamous epithelial cells owing to the sterilization of mucosal stem cells and the inhibition of transit cell proliferation. This leads to a gradual linear decrease in epithelial cell numbers. Normally, oral mucosal cells have a rapid turnover rate of 1 to 2 weeks, which is reduced with radiation therapy, interfering with recovery of mucosal damage. Poor nutritional status further interferes with mucosal regeneration by decreasing cellular migration and renewal. As one advances in the course of radiation, the initial erythema/mucosal congestion transforms into patchy or confluent mucositis when the delicate balance between cell death and cell regeneration is altered, resulting in partial or complete denudation. As the mucositis becomes more severe, pseudomembranes and ulcerations develop.
- ■
There is a higher chance of developing secondary infections with damaged mucosal surfaces, which would otherwise form the primary barrier to protect any penetration by microorganisms. There is loss of “colonization resistance” which is a potent defense mechanism used by homeostatic microbial communities which prevents colonization by exogenous pathogens. When oral tissues are irradiated, the colonization resistance is practically abolished. Irradiation mucositis is caused by a combination of alteration of the normal oral microflora with concomitant changes in the tissues. However, healing eventually occurs when cells regenerate from the surviving mucosal stem cells.
- ■
To summarize, the following are the stages of pathogenesis of mucositis, based on evidence available date 20 :
- ■
Initiation of tissue injury: Radiation and chemotherapy induces cellular damage resulting in the death of the basal epithelial cells. The generation of ROS by radiation or chemotherapy is also believed to exert a role in the initiation of mucosal injury. These small highly reactive molecules are by-products of oxygen metabolism and can cause significant cellular damage. The consistent reports of ROS generation after exposure to stomatotoxic agents and the results of studies that demonstrate successful attenuation of mucosal injury by agents that effectively block or scavenge oxygen‐free radicals suggest a significant role for ROS in injury induction.
- ■
Upregulation of inflammation via generation of messenger signals: In addition to causing direct cell death, free radicals activate second messengers that transmit signals from receptors on the cellular surface to the inside of cell. ROS stimulates secondary mediators of injury, including transcription factors such as NF‐κB. This leads to upregulation of genes producing proinflammatory cytokines, including the genes for TNF‐α, IL‐1β, and IL‐6, leading to tissue injury and apoptosis of cells within the submucosa and primary injury of cells within the basal epithelium. Other genes also are upregulated, leading to the expression of adhesion molecules, cyclooxygenase‐2 (COX‐2), and subsequent angiogenesis. ROS and anticancer drugs can also activate enzymes (sphingomyelinase and ceramide synthase) that catalyze ceramide synthesis, complementing the ceramide pathway which appears to work in parallel, or sequentially, to induce primary apoptosis.
- ■
Signaling and amplification: During this phase, one of the consequences of upregulation of proinflammatory cytokines, such as TNF-α, is a series of positive feedback loops that serve to amplify and prolong tissue injury through their effects on transcription factors and on the ceramide and caspase pathways. Consequently, gene upregulation occurs with resultant increases in injurious cytokine production. Because the damaging events are focused in the submucosa and basal epithelium, the clinical appearance of the mucosal surface remains deceptively normal.
- ■
Ulceration and inflammation: The ulcerative phase is a result of cell injury and death of the basal epithelial stem cells after the prior phases. This phase is generally markedly symptomatic. The ulcers serve as a nidus for bacterial colonization, and secondary infection is common. The cell wall products from bacteria penetrate the submucosa and further exacerbate the condition by stimulating infiltrating macrophages to produce and release additional proinflammatory cytokines, further amplifying and accelerating local tissue damage. ,
- ■
Healing: This phase starts with a signal from the extracellular matrix and is characterized by epithelial proliferation, as well as cellular and tissue differentiation, restoring the integrity of the epithelium, and reestablishment of the local microbial flora. The mucosa regains its normal appearance with, however, significant alterations in the environment. There is residual angiogenesis, which puts patients at increased risk of future episodes of oral mucositis.
- ■
- ■
The pathobiology of mucositis shows that it is the culmination of a series of biologically complex and interactive events that occur in all tissues of the mucosa. Although the complete definition of mucositis as a biological process remains a work in progress, the current understanding of cellular and molecular events that lead to mucosal injury has provided a number of potential interventional targets. Consequently, for the first time, directed, biologically rational therapies are now in various stages of development. Furthermore, mechanistically based risk prediction and disease monitoring appear to be realistic goals for the future.
Pharmacological Approaches for Management and Treatment
The clinical management for oral mucositis and esophagitis can be categorized into agents for the therapeutic management of mucositis, pain control, control of infections, and dry mouth.
- ■
Therapeutic agents for oral mucositis and esophagitis: This class of medications include medications which may be used to decrease the chance of developing oral mucositis or to shorten the duration of oral mucositis in patients receiving chemotherapy and radiation therapy.
- ■
Anti-inflammatory/immunomodulatory agents:
- ■
Benzydamine hydrochloride 0.15%: Benzydamine hydrochloride is a nonsteroidal anti-inflammatory mouth rinse that is recommended for use to prevent and/or relieve the pain and inflammation associated with oral mucositis in patients who are receiving moderate doses of radiation therapy for head and neck cancer. It inhibits proinflammatory cytokines including TNF-α. In a phase III trial, benzydamine hydrochloride mouth rinse reduced the severity of mucositis in patients with head and neck cancer undergoing radiation therapy of cumulative doses of up to 50 Gy radiation therapy.
- ■
Indomethacin : Indomethacin is a nonsteroidal anti-inflammatory drug which inhibits prostaglandin synthesis and is noted to delay the onset of mucositis.
- ■
Prednisone : A short course of systemic prednisone (40 to 80 mg daily for up to 1 week) has been helpful in reducing inflammation and discomfort.
- ■
- ■
Cytoprotective agents
- ■
Amifostine: Amifostine is a cytoprotectant agent that may help to reduce the incidence and severity of chronic or acute xerostomia in patients who are receiving radiation therapy for head and neck cancer. It is a phosphorothioate (a radiation protection agent) and is thought to act as a scavenger for harmful ROS that are known to potentiate mucositis. However, because of insufficient evidence of benefit, various guidelines do not recommend the use of this agent in oral mucositis in chemotherapy or radiation therapy patients. The use of amifostine, however, has been recommended for the prevention of esophagitis in patients receiving chemoradiation for non–small-cell lung cancer.
- ■
Sucralfate: Sucralfate is a cytoprotective agent used for GI ulcerations. It is a basic aluminum salt of sucrose octasulfate and may be useful in reducing symptoms and discomfort and help healing by coating the esophagus. Studies have been negative in the radiation arena for oral mucositis, and a new randomized controlled trial of sucralfate in radiation treatment has confirmed this lack of benefit, showing no difference between micronized sucralfate and salt and soda mouth washes. However, some patients with severe esophagitis may derive symptomatic benefit.
- ■
- ■
Growth factors
- ■
Palifermin : Palifermin is a recombinant human keratinocyte growth factor-1, which can increase epithelial cell proliferation, and has been used for the management of oral mucositis. Recent evidence shows that intravenous recombinant palifermin significantly reduced incidence of World Health Organization (WHO) grade 3 and 4 oral mucositis in patients with hematological malignancies (e.g., lymphoma and multiple myeloma) receiving high-dose chemotherapy and total body irradiation before autologous hematopoietic stem cell transplantation. , Palifermin is also known to prevent oral mucositis in patients with head and neck cancer undergoing radiation and chemotherapy, according to two randomized trials. There is a theoretical concern that these growth factors may promote growth of tumor cells, which may have receptors for the respective growth factor. However, one recent study found no significant difference in survival between subjects with colorectal cancer receiving palifermin compared with placebo at a median follow-up duration of 14.5 months. , Further studies are ongoing to confirm the safety of epithelial growth factors in the solid tumor setting, including patients receiving radiation therapy for head and neck cancer.
- ■
- ■
- ■
Agents used for pain control: In general, topical analgesics provide rapid but temporary relief to a localized area. Oral opioids and opioid-containing combinations may be necessary for more moderate or persistent pain. Analgesics should be given at regular intervals for moderate and severe pain.
- ■
Topical analgesics/anesthetics:
- ■
Magic mouthwash: Magic mouthwash is the most commonly prescribed medication for oral mucositis and esophagitis. It is made up of lidocaine, diphenhydramine, and magnesium aluminum hydroxide, in equal amounts. Patients are asked to swish and gargle for 1 minute, and then swallow immediately before each meal. Similar preparations have been made with readily available ingredients for patients who have oral thrush. This is commonly known as the GI Cocktail (1 tbsp. [15 mL] Cherry Maalox [analgesia] + 1 tsp. [5 mL] Nystatin [antifungal] + 1/2 tsp. [2 mL] Hurricane Liquid [analgesia] original flavor).
- ■
Oxethazaine aluminum/magnesium hydroxide (Mucaine) analgesic/antacid Combination: This combination is useful for esophagitis and should be taken 10 to 15 minutes before meals and at bedtime.
- ■
Lidocaine HCl 2%: Oral lidocaine is usually swished in the mouth and spat out, up to 6 times daily. It may be swallowed slowly if there is also pharyngeal involvement; however, this can impair the swallowing reflex and may increase the risk of aspiration. Given this risk, it should be used carefully.
- ■
Benzocaine : Benzocaine is used as an adhesive paste as a topical anesthetic for local application to affected ulcerations.
- ■
- ■
Systemic analgesics:
- ■
Acetaminophen/codeine: Acetaminophen with codeine is an opioid-containing analgesic in tablet form, prescribed during early mucositis when patients can still swallow medication.
- ■
Liquid acetaminophen/codeine: The aforementioned combination is also available in a liquid formulation that is used for severe mucositis-induced odynophagia.
- ■
Morphine: Morphine is an opioid available in tablet, liquid, or IV formulations.
- ■
Hydromorphone HCl : Hydromorphone is a particularly potent opioid that is available in both enteral and parenteral formulations.
- ■
Transdermal fentanyl: Fentanyl patches are opioid analgesics used for stable and chronic pain as it is available as a skin patch to be replaced every 72 hours. Note that parenteral forms of fentanyl are also available; however, these are very short acting.
- ■
Patient-controlled analgesia: Some patients with very severe mucositis may require systemic opioids administered continuously via patient-controlled analgesia (PCA) pumps.
- ■
- ■
- ■
Oral infection management: Depending on the causative organism, an antifungal, antiviral, or antibacterial can be used and can be administered either topically or systemically. The systemic route is most useful for patients at risk of serious infections (e.g., patients with myelosuppression).
- ■
Antifungals: If symptoms of mucositis start earlier in the course of radiation therapy, get worse suddenly, or persist a long time after treatment completion, a candidal (monilial fungal) infection may be present, which can be effectively treated with multiple antifungal agents.
- ■
Nystatin oral suspension is one of the most commonly used agents to prevent and treat candidiasis in the mouth and esophagus. The usual instructions entail to swish in mouth for 5 minutes, then spit out or swallow. Patients should avoid eating for at least 30 minutes after use.
- ■
Fluconazole is a commonly used systemic treatment for fungal infections.
- ■
Other agents to treat oral candidiasis include ketoconazole, amphotericin, and itraconazole.
- ■
- ■
Antivirals:
- ■
Acyclovir ointment is used as a topical therapy for herpes labialis.
- ■
Acyclovir, famciclovir, and valacyclovir are used for systemic herpes treatment. Note that short courses of these agents can also be used for herpes labialis.
- ■
- ■
Antibacterials: Oral decontamination has historically been shown to reduce infection of the oral cavity by opportunistic pathogens. Furthermore, it can also reduce the risk of systemic sepsis from resident oral and/or opportunistic pathogens. In the past, some commonly used selective oral decontamination agents included chlorhexidine gluconate mouth rinse to suppress oral microflora and prevent dental plaque formation. Later, given some evidence suggesting lack of benefit of chlorhexidine, this agent fell out of favor. Antimicrobial lozenges in patients receiving radiation for cancers of head and neck were then assumed to provide effective mucositis prevention. Addition of ciprofloxacin or ampicillin with clotrimazole to sucralfate had shown reduction in mucositis. However, a few recent studies of oral lozenges that contained polymyxin, tobramycin, and amphotericin B or bacitracin, clotrimazole, and gentamicin showed no improvement in the incidence or severity of radiation‐induced mucositis. , Despite the often-postulated role of infection in the pathogenesis of mucositis, there is no conclusive evidence for the use of antibiotics in the prevention of radiation-induced mucositis. They might be still useful in cases of severe mucositis and would be recommended if suspicion for bacterial infection is high.
- ■
- ■
Agents for dry mouth: In cancer therapy, patients often develop transient or permanent xerostomia and hyposalivation. Hyposalivation can further aggravate inflamed tissues, increase risk for local infection, and make mastication difficult. Many patients also complain of a thickening of salivary secretions, because of a decrease in the serous component of saliva.
- ■
Products to moisturize dry mouth include prescription or over-the-counter mouth rinses, artificial saliva, or moisturizers to lubricate the mouth. Mouthwashes designed for dry mouth, especially ones with xylitol, can be effective, such as Biotene Dry Mouth Oral Rinse or Act Dry Mouth Mouthwash, which also offer protection against tooth decay. Saliva substitutes (e.g., Moi-Stir) are available as sprays or swabs to be used as needed. SalivaMAX is an artificial saliva that is used to relieve acute and chronic symptoms of xerostomia and mucositis. It is a supersaturated calcium phosphate powder that, when dissolved in water, creates a solution with a high concentration of electrolytes similar to that of natural saliva.
- ■
Cholinergic agents are prescribed as necessary. Commonly prescribed agents include pilocarpine (Salagen) or cevimeline (Evoxac) to stimulate saliva production.
- ■
Nonpharmacological Approaches for Management and Treatment
- ■
Nonpharmacological interventions for oral mucositis and esophagitis include general healing measures, nutritional support, oral hygiene, oral decontamination, and interventions for palliation of dry mouth.
- ■
Frequent use of a gentle mouthwash may help reduce discomfort or pain. A solution of baking soda and salt dissolved in warm water may be used instead of commercial mouthwashes, which may be irritating to the oral mucosa.
- ■
Nutritional support: All patients should be screened for nutritional risk and early enteral nutrition should be initiated in the event that swallowing difficulties develop. A soft diet or liquid diet is more easily tolerated than a normal diet when oral mucositis is present; gastrostomy tube placement may be beneficial, particularly when there is severe mucositis.
- ■
Oral hygiene: Proper oral care reduces some of the oral toxicity of radiation therapy. Multiple studies have demonstrated that maintenance of good oral hygiene can reduce the risk and severity of oral mucositis. Alcohol-containing mouthwashes should be avoided as these can cause further irritation. The importance of effective oral hygiene should be stressed with recommendations for use of a standardized oral care protocol, including brushing with a soft toothbrush, flossing, and the use of nonmedicated rinses (for example, saline or sodium bicarbonate rinses). ,
- ■
Oral decontamination: Oral decontamination is achieved by maintaining a good oral hygiene. Apart from pharmacological measures, some over-the-counter products like Cepacol Lozenges, Chloraseptic spray and lozenges, or the use of tea for swishing and gargling may help. Oral Balance is a dental gel that moistens the mouth while sores are healing and also has enzymes that help control oral bacteria. Saline mouthwashes are also preferred for their antiseptic properties.
- ■
Palliation of dry mouth: Sipping of water or ice chips throughout the day to moisten the mouth, in addition to drinking water during meals to aid chewing and swallowing, are beneficial techniques that should be relayed to patients.
- ■
Breathing through the nose rather than through the mouth is encouraged. Patients may even need to seek treatment for snoring if it causes them to breathe through their mouth during the night.
- ■
Chewing sugar-free gum or sucking on sugar-free hard candies may help stimulate salivary flow and improve symptoms of dry mouth.
- ■
Some over-the-counter saliva substitutes that contain xylitol (such as Mouth Kote or Oasis Moisturizing Mouth Spray), carboxymethylcellulose, or hydroxyethyl cellulose (such as Biotene OralBalance Moisturizing Gel) are recommended. Products that contain xylitol may also help prevent cavities.
- ■
Simple measures like adding moisture to the air at night with a room humidifier, or moisturizing lips to soothe dry or cracked areas, can be helpful.
- ■
Avoidance of products that can make xerostomia symptoms worse is also important. These include caffeine, tobacco, and alcohol, which can cause dryness and irritation. Over-the-counter antihistamines and decongestants can worsen dry mouth as well.
- ■
- ■
Newer developments in radiation therapy: With the use of newer modalities in radiation treatment, there are multiple ways to reduce the incidence of oral mucositis and esophagitis. Various steps can be taken to decrease toxicity in normal tissues, including precise treatment planning and irradiation techniques, selective decreased volume receiving higher doses dictated by estimated cell burden, and maneuvers to exclude sensitive organs (oral mucosa and esophagus) from the irradiated volume. With the emphasis on organ preservation, treatment planning is critical to achieve maximum tumor control probability (TCP) with the least side effects and satisfactory cosmetic results. Some recent changes in the field of radiation oncology, which have led to some reduction in the incidence and severity of oral mucositis and esophagitis, include:
- ■
The use of custom-made, intraoral prosthesis to exclude uninvolved tissues from the treatment portals or to provide shielding of tissues within the treatment area to aide with mucosal sparing.
- ■
Computed tomography (CT)-based simulation and target delineation ( Fig. 26.2 ) for accurate definition of the tumor and subclinical disease has led to better sparing of nontumor tissue with smaller target margins.
- ■