- ♦
Minimally invasive parathyroidectomy (MIP), or focused parathyroidectomy, was developed to facilitate surgical management of single-gland parathyroid disease with a smaller incision and less tissue dissection than the traditional four-gland exploration.
- ♦
MIP does not include extrathyroid approaches (e.g., axillary or chest wall), which require an extensive dissection to avoid a cervical incision, nor does it include focused unilateral parathyroid exploration via a standard full-length cervicotomy. Smaller incisions and less tissue dissection with MIP translate into better cosmesis, less pain, and shorter hospital stays.
- ♦
This technique has been conclusively demonstrated to be as safe as open four-gland exploration. MIP is now accepted as the first-line treatment for surgical management of primary hyperparathyroidism due to a single adenoma, with success rates exceeding 96%.
- ♦
The application of MIP requires careful patient selection and attention to the embryologic development of the parathyroids and variations in gland location. We summarize the lessons learned by predecessors in this operation from first assessment through operation and discharge.
Step 1. Surgical Anatomy
- ♦
The minimally invasive or focused approach to parathyroid surgery requires a thorough understanding of the anatomic relationships of the parathyroid glands to adjacent landmark structures, including the recurrent laryngeal nerve and the inferior thyroid artery.
- ♦
The inferior and superior parathyroid glands are derived from the third and fourth pharyngeal pouches, respectively. This embryologic derivation and the subsequent migration of these pouches accounts for the final location of these glands in the neck.
- ♦
The superior parathyroids are typically found within 1 cm of the intersection of the inferior thyroid artery and the recurrent laryngeal nerve, commonly cephalad or on the surface of the tubercle of Zuckerkandl of the thyroid.
- ▴
Abnormal superior parathyroid glands generally descend along the tracheoesophageal groove into the mediastinum in a plane posterior to the recurrent laryngeal nerve.
- ▴
- ♦
The inferior parathyroid glands, derived from the third pharyngeal pouch, descend with the developing thymus and are typically found on the anterior or inferior aspect of the thyroid gland or within the thyrothymic ligament.
- ▴
Ectopic inferior parathyroid glands may be intrathyroid or may descend into the anterior mediastinum within the thymus.
- ▴
Undescended inferior parathyroid glands can be located in the carotid sheath.
- ▴
- ♦
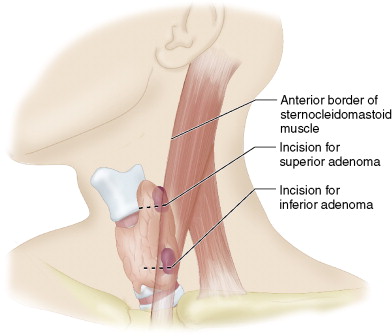
Demarking the prevertebral fascia, carotid artery, tubercle of Zuckerkandl, and tracheoesophageal groove will allow the surgeon to identify a region in the neck that contains at least 90% of the superior and inferior parathyroid glands found in either predicted or ectopic locations ( Fig. 8-1 ).
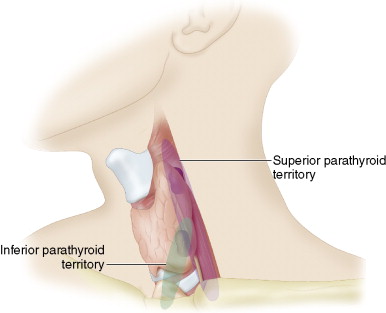
Figure 8-1
Step 2. Preoperative Considerations
- ♦
MIP is designed for single-gland disease, namely parathyroid adenomas. A confident diagnosis and accurate localization of the diseased gland are thus fundamental to the success of this technique; a great deal of literature describes the application of different biochemical tests and imaging modalities to identify the hyperfunctioning gland.
- ▴
First the diagnosis must be confirmed with an elevated serum calcium and an elevated or inappropriately suppressed parathyroid hormone (PTH) level.
- ▴
It is important to note that there is also a small subgroup of patients with symptomatic bone disease who have normocalcemic hyperparathyroidism; these patients may also benefit from MIP.
- ▴
- ♦
A 24-hour urine collection for measurement of urine calcium concentration must also be done to exclude familial hypocalciuric hypercalcemia.
- ♦
After diagnosis, risk factors for multiglandular disease should be identified, including personal or family history of multiple endocrine neoplasia or familial hyperparathyroidism, previous radiation exposure, or chronic renal failure. The presence of these factors will significantly increase the risk of a failed MIP because of multiple abnormal parathyroid glands; they are considered exclusion criteria.
- ♦
The most common and tested modalities for preoperative localization are Tc 99m sestamibi scan and high-resolution ultrasonography. Our practice is to perform an initial Tc 99m sestamibi scan followed up by a focused ultrasound to define the anatomic features and precise localization of the parathyroid adenoma as well as to assist with incision placement.
- ♦
Kebebew and colleagues developed a scoring model for predictors of single-gland disease, with the following five criteria: single site on sestamibi scan, single site on ultrasound, concordant localization, serum calcium >1 mg/dL above the upper normal limit, and PTH twice upper limit of normal. Scores of 3 or more were reported to have a positive predictive value of 100%.
- ♦
There are cases in which repeat studies can clarify discordant results, especially with sestamibi scans. Concordant imaging is associated with a greater than 98% cure on removal of the enlarged parathyroid gland.
- ♦
Localization can be complicated by anatomy, such as obesity, multinodular goiter, or previous neck surgery. In these cases the MIP may be contraindicated.
- ♦
Even under ideal circumstances patients are quoted a 5% possibility of requiring conversion to open exploration.
Step 3. Operative Steps
- ♦
MIP can be performed under local or general anesthesia within an ambulatory setting. Our unit commenced MIP using a video-assisted technique, then progressed to a central mini-incision technique before utilizing the lateral technique, which significantly facilitates anatomic exposure of the parathyroid glands, especially those in a superior or posterior location.
Positioning
- ♦
The patient is positioned supine with the neck held in extension with slight rotation to the contralateral side. An operating headlight is used by the surgeon to provide illumination of the narrow operative field. The suprasternal notch, cricoid cartilage, and medial border of the sternocleidomastoid muscle are all marked to provide orientation and aid in operative planning.
Incision
- ♦
Incision placement depends on the localization to either the superior or inferior gland ( Fig. 8-2 ). This is guided by the preoperative ultrasound, which is most useful when the location of the adenoma has been described using constant landmarks such as the cricoid cartilage as reference points.