Abstract
Managing patients with bone metastases requires a multidisciplinary approach applying the expertise of orthopedic surgeons, radiation oncologists, medical oncologists, and radiologists. Small lesions can usually be successfully treated with radiation therapy alone, with subsequent surgical stabilization only for continued symptoms or fracture. Bones with diffuse, permeative destruction should be internally stabilized prophylactically if possible, followed by postoperative radiation therapy. Unless contraindicated, all patients with metastatic carcinoma of the breast with involvement of the bone should receive systemic osteoclast inhibitor therapy for the prevention of skeletal related events, irrespective of pain symptoms or extent of disease. Future treatment modalities will further decrease the substantial morbidity associated with the development and progression of bone metastases.
Keywords
breast cancer, bone metastases, bone pain, skeletal related events, pathologic fracture
Bone is the most common site of first recurrence in patients with breast cancer; affecting up to 70% of patients with metastatic disease. Patients with bone metastases are at high risk for developing clinically significant complications, often referred to as skeletal-related events (SREs), including radiation therapy or surgery to prevent or treat fracture and palliate pain, pathologic fracture (excluding major trauma), spinal cord compression, and hypercalcemia. If untreated, metastatic breast cancer patients experience an average of four complications per year related to bone metastases, with pathologic fractures and radiation therapy being the most commonly observed SREs. Cancer registry data suggest that patients with metastatic breast cancer who develop SREs live significantly shorter than similar metastatic patients who do not develop skeletal complications. Complications stemming from bone metastases can be life-threatening and are a major source of morbidity for patients, making their prevention and treatment a vital component of comprehensive oncologic care.
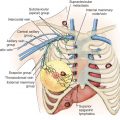
The development of bone metastases is common to all breast cancer subtypes but is especially prevalent in estrogen receptor–positive disease in which bone metastases are found in more than 80% of patients with distant relapse compared with 50% in patients with breast cancer negative for hormone receptor and HER2 expression (triple negative). Up to 30% of patients with metastatic breast cancer relapse exclusively in the bone without visceral involvement (bone-only disease). The most common skeletal sites affected, in decreasing order of frequency, are the spine, pelvis, skull, ribs, and femur. The lumbar spine is the single most commonly involved site, accounting for up to 20% of osseous metastases. In the appendicular skeleton, the proximal femurs are the most common site of metastases, followed by the humeri.
This chapter addresses the pathophysiology, clinical presentation, diagnosis, and treatment of bone metastases with surgery, radiotherapy (RT), and systemic osteoclast inhibitors. Chapters 69 and 70 discuss chemotherapy and endocrine therapy options for patients with bone metastases, and are not discussed here. However, poor systemic disease control remains the greatest risk factor for progression of bone metastases and for the development of SREs, rendering traditional cytotoxic and targeted antitumor therapies essential in the management of all patients with bone metastases.
Pathophysiology
During physiologic conditions, bone is in a state of constant remodeling, maintaining a dynamic balance between osteoclastic (resorptive) and osteoblastic (bone-forming) activity. Bone resorption is mediated by osteoclasts, multinucleated giant cells derived from granulocyte-macrophage precursors. Bone formation is carried out by osteoblasts, which are derived from mesenchymal fibroblast-like cells. The receptor activator of NF-κB ligand (RANKL)-RANK pathway mediates osteoclast activity is a key regulator of bone metabolism. RANKL is produced by osteoblasts, bone marrow stromal cells, and other cells under the control of various proresorptive growth factors, hormones, and cytokines including parathyroid hormone (PTH), parathyroid hormone–related peptide (PTHrP), progesterone, prostaglandins, and interleukins. By binding to the RANK receptor expressed on osteoclasts and preosteoclasts, RANKL controls the development, formation, activation, and survival of osteoclasts and plays a primary role in stimulating osteoclast-mediated bone resorption. As the only known ligand for the RANK receptor, RANKL is indispensable for normal osteoclast activity. Osteoblasts and stromal cells also produce osteoprotegerin, a soluble decoy receptor that binds to and inactivates RANKL preventing osteoclast activation. The RANKL/OPG ratio is the primary determinant of osteoclast activity in physiologic as well as several pathologic conditions, including cancer.
In patients with metastatic bone disease, bone formation and resorption are uncoupled, leading to both osteoblastic and osteolytic lesions. Bone resorption can occur through tumor-mediated osteolysis in which cancer cells directly resorb local bone or, more commonly, through the direct activation and stimulation of osteoclasts via the secretion of RANKL as well as other osteoclast-stimulating factors. The process of bone resorption leads to the release of growth factors from the bone matrix including type I collagen, osteocalcin, insulin-like growth factors, transforming growth factor (TGF)-β, as well as calcium, which may stimulate cancer cells directly, leading to the hypothesized vicious cycle of bone destruction and progressive tumor growth.
PTHrP is often the primary culprit responsible for RANKL release and bone destruction in breast cancer patients. This protein was originally identified as a hypercalcemic factor in several cancer types, including breast. PTHrP has 70% homology to the first 13 amino acids of PTH, the major hormone responsible for calcium homeostasis and binds to the common PTH/PTHrP receptors. The binding of PTHrP to receptors on osteoblasts and marrow stromal cells results in the production of RANKL, causing increased osteoclast differentiation and activation and the initiation of the vicious cycle. Approximately 80% of hypercalcemic patients with solid tumors have detectable plasma PTHrP concentrations.
The pathogenesis of osteoblastic metastases is less well understood than that of osteolytic lesions. As with osteolytic lesions, osteoblastic bone metastases are the result of dysregulated bone metabolism. Preclinical data suggest that in osteoblastic lesions, an initial phase of bone destruction may be followed by extensive bone formation, supported by the presence of elevated bone turnover markers in patients with prostate cancer metastatic to the bone. Endothelin-1, a vasoconstrictor peptide produced by prostate and breast cancer cells, is thought to be a stimulator of the osteoblast proliferation contributing to the development and progression of blastic metastases.
Clinical Presentation
Pain is the most common presenting symptom of bone metastases and is seen in up to 75% of patients. Bone pain is also the most common cause of cancer-related pain in metastatic patients, rendering pain control an essential goal of therapy. The mechanisms of pain production are varied and depend on the location of the metastatic foci as well as the type of lesion causing the pain. Nociceptive pain is caused by the local release of cytokines and chemical mediators by tumor cells, periosteal irritation, and stimulation of intraosseous nerves. Neuropathic pain is produced by the direct destruction of nerve tissue by tumors, whereas mechanical pain is caused by pressure or mass effect of the tumor within the bone, leading to loss of bone strength. The use of pharmacologic therapies including nonsteroidal antiinflammatory drugs, opioid analgesics, gamma-aminobutyric acid (GABA) analogs, and corticosteroids are often an important and necessary adjuvant to nonpharmacologic therapies for pain control.
Other common presenting signs and symptoms in untreated patients include pathologic fractures, spinal cord compression, and hypercalcemia. Because bone metastases from breast cancer most frequently include a lytic component, pathologic fracture is the most commonly observed SREs, occurring in up to 60% of patients with metastatic breast cancer to bone in historical series.
Spinal cord compression is also more common in breast cancer patients compared with other cancer types; however, it remains a relatively rare complication, occurring in only 3% to 5% of patients. Cord compression most commonly occurs by direct extension of a hematogenously derived vertebral body metastasis into the epidural space with resultant compression of the spinal cord. Symptoms of spinal cord compression include pain, weakness, and sensory changes, with bowel or bladder dysfunction a late finding (see Chapter 73 ). Sixty percent of patients with back pain and an abnormal two-dimensional projection radiograph (plain radiograph) of the spine, have epidural disease on magnetic resonance imaging (MRI).
Before effective treatment with bone-targeted and antitumor therapies, hypercalcemia was observed in up 20% of patients with metastatic breast cancer to bone. More recent studies suggest that hypercalcemia of malignancy is a rarer condition, affecting less than 5% of patients with breast cancer. Hypercalcemia of malignancy is thought to occur by several mechanisms, including direct skeletal destruction by tumor and via the release of humoral factors secreted by tumor cells, including PTHrP. Hypercalcemia can also rarely occur as a complication of hormonal therapies, especially tamoxifen, as part of the flare response (see Chapter 70 ). Hypercalcemia may result in a variety of gastrointestinal, renal, neurologic, and cardiovascular complications including constipation, nausea, fatigue, lethargy, and death. The marked decrease in the incidence of malignant hypercalcemia is thought to be in part a result of the increased use of systemic osteoclast inhibitors including bisphosphonates and denosumab in patients with metastatic breast cancer.
Diagnosis
The diagnosis of bone metastases is suggested by the presence of symptoms, abnormal laboratory values (alkaline phosphatase and calcium), and imaging studies. Imaging studies may include plain radiographs, 99m Tc bone scintigraphy (bone scan), MRI, computed tomography (CT), and positron emission tomography (PET) with or without CT or MRI. Plain radiographs are often the first test in the evaluation of bone pain because they are inexpensive and specific when abnormal albeit relatively insensitive (50%) for the detection of bone metastasis. Bone scans are more sensitive than plain radiographs, particularly for lesions with a blastic component as the radiolabeled diphosphonate preferentially accumulates in areas of osteoblastic activity. However, limitations in diagnostic specificity require confirmation of abnormal findings with plain radiographs, CT, MRI, or preferably biopsy. Bone scans are also less helpful for monitoring early responses because flare reactions can be observed for up to 8 months in responding lesions secondary to increased reparative osteoblastic activity. CT imaging provides additional information such as the presence of soft tissue masses and cortical integrity. MRI is superior for identifying spinal metastases, diagnosing radiologic spinal cord compression, and assessing bone marrow involvement.
Fluorodeoxyglucose ( 18 F-FDG) PET/CT has shown higher sensitivity and specificity than bone scans for detecting osteolytic bone metastases because FDG uptake occurs predominantly in cancer cells providing for a more specific tumor tracer. However, PET scans may not be as sensitive as bone scans for detecting osteoblastic metastases, and in particular lesions originating from invasive lobular breast cancers. Recent studies suggest 18 F-FDG PET has improved sensitivity over bone scans in detecting early bone lesions as FDG uptake in metastatic tumor cells in the bone marrow may predate the osteoblastic activity required for detection by bone scan. 18 F-FDG PET scans have limitations in certain parts of the body, such as the skull, where uptake from the brain may prevent visualization of skull metastases. PET offers an additional advantage for monitoring response to therapy as decreases in PET uptake (SUV max ) correlate with tumor responses and time to progression. 18 F-FDG PET/MRI has similar sensitivity as 18 F-FDG PET/CT but provides better anatomic delineation.
Fluorine-18–labeled sodium fluoride (F-fluoride) PET allows for the detection of bone metastases with high contrast and spatial resolution as 18 F-NaF is rapidly absorbed into areas of osteoblastic activity with subsequent incorporation into the bone mineral as a fluorapatite. F-fluoride PET has been shown to be more sensitive than bone scan as well as 18 F-FDG PET for detecting bone metastases; however, changes in SUV max have not been consistently reported to correspond to tumor responses. In addition, F-fluoride PET is useful only for the detection of bone metastases, whereas 18 F-FDG PET can be useful for detecting metastases in other organs and sites outside the bone.
Surgical Management
Surgery plays a vital role in the management of bone metastases, principally for lesions with a complete or impending pathologic fracture. It is also a consideration in patients presenting with spinal cord compression. The proximal femur is the most common metastatic location requiring surgical intervention in breast cancer. The combination of frequent involvement, high stress and torque forces placed on the bone, and the significant morbidity associated with femur fractures justify the rate of surgical intervention. Disease metastatic to the humerus is better tolerated than disease in the lower extremity, unless the patient needs crutches for ambulation.
For both the upper and lower extremities, two operative strategies are commonly considered: (1) endoprosthetic reconstruction or (2) internal fixation with either intramedullary nailing or plate/screw fixation devices. Factors that favor endoprosthetic reconstruction over intramedullary stabilization include large periarticular lesions, involvement of the femoral neck, substantial bone loss, severe fracture comminution, and an oncologic benefit to resection. Before surgically managing a completed or impending pathologic fracture, the entire bone in question should be imaged as other lesions in the vicinity may affect operative planning.
In a systematic review of 45 studies addressing the role of surgical management of bone metastases in multiple cancer types (including both prophylactic and after fracture), pain relief after surgical management was achieved in 91% to 93% of cases, and function was maintained or improved in 89% to 94%. The pooled complication and mortality rates were 17% and 4%, respectively. The most commonly encountered complications in cancer patients include superficial surgical site infection and deep venous thrombosis.
Spinal cord compression from metastatic disease is considered a medical emergency because prompt treatment is essential to reverse neurologic symptoms. Metastatic breast cancer accounts for 15% to 20% of all cases of metastatic epidural spinal cord compression with the thoracic spine being the most common site affected followed by the lumbosacral and cervical spines. Corticosteroids, RT, and decompressive surgery are the established therapies with pain control and maintenance of function the goals of care. Indications for surgery include the need for tissue diagnosis; bone impinging into the spinal canal producing thecal compression; spinal instability with unremitting mechanical pain; radiculopathy with progressive or uncontrolled symptoms; and tumor growth unresponsive to RT or neurologic progression after RT. Randomized clinical trials support the use of early decompressive surgery for maintaining ambulation; however, age has emerged as an important variable in predicting preservation of function, and in patients over 65 years of age, marginal benefit was observed with surgery compared with radiation alone.
Prophylactic Surgery
As a rule, if the patient undergoes surgery before fracture, the technical procedure is considerably simplified for the surgeon. In addition, patient morbidity and mortality are minimized because the patient does not suffer the intense pain associated with fracture or experience the complications inherent with the restrictions of immobilization associated with bed rest. The need for prophylactic surgery should be based on the estimated risk of fracture and the short-term prognosis of the patient.
Criteria historically used for selecting patients for prophylactic stabilization include lesions greater than 2.5 cm in greatest dimension involving the femur, lytic destruction of greater than 50% of the cortex of a long bone, avulsion of the lesser trochanter as seen on plain radiographs, and continued pain with weight bearing after radiation therapy. If the patient has underlying osteoporosis, any defect in the cortex may weaken the bone sufficiently that fracture may occur with normal activity. Such pathologic or spontaneous fractures can occur with minimal stress, such as torque of the skeleton (twisting) when getting out of bed.
Scoring systems provide an objective method for estimating fracture risk. The Mirels Scoring System consists of a 12-point scale incorporating factors known to influence the risk of fractures such as the location of the lesion, severity of pain, degree of cortical destruction, and radiographic appearance (i.e., lytic, blastic, or mixed). A score of 9 or higher defines an impending pathologic fracture for which prophylactic stabilization is recommended. This scale is widely used, has been validated in several studies, and in at least one series was found to be more sensitive than clinical judgment alone in assessing impending fracture risk.
Pathologic Fractures
The main goals of surgery for pathologic fractures are to relieve pain and permit ambulation of the patient in the immediate postoperative period, to provide sufficient stability and bone apposition for a union to be achieved, and to debulk the tumor. Commonly used criteria for performing surgery are life expectancy of at least 1 month for a fracture of a weight-bearing bone, life expectancy of at least 3 months for a fracture of a non–weight-bearing bone, the ability to tolerate surgery, sufficient integrity of the surrounding bone to support the surgical device, and whether surgery will allow mobilization or facilitate general care in the context of the patient’s overall performance status. A single, definitive surgery is preferable because many patients with metastatic cancer will be unable or unwilling to undergo subsequent procedures.
Early operative stabilization of the pathologic fracture permits patients to ambulate quickly and decreases the risk of complications related to immobilization and pain medications. The most common factors associated with reconstructive failure after intramedullary fixation include tumor progression, nonunion, and hardware failure. If osseous union is not achieved, internal fixation devices have a high risk of early failure. Resection of tumor, usually through intralesional curettement, is recommended to achieve local tumor control and allow surgical adjuvants, such as postoperative RT, to work more effectively. Removal of gross disease also permits the use of polymethylmethacrylate cement to fill the defect, leading to improved stability and faster time to weight bearing activity.
All patients should be evaluated for RT after operative stabilization to promote bone healing, reduce pain, and reduce the risk of subsequent fracture. A retrospective study from the University of Kansas by Townsend and colleagues found that postoperative RT was associated with improved function up to 12 months after surgery and decreased the need for further orthopedic procedures at the same site.
Radiotherapy
Radiotherapy Alone
RT plays a primary role in the relief of painful bony metastases. The exact mechanism for the analgesic effect is unknown, although radiation-induced death of host macrophages that release chemical mediators of pain (e.g., prostaglandin E2) and interference with bone resorption by osteoclasts are the main hypotheses.
Older series have reported complete pain relief in approximately 50% of patients and partial pain relief in 80% to 90% of patients. More recent studies using stricter criteria for pain response have reported complete response rates of 15% to 40% and partial pain relief in 60% to 80% of patients. The incidence of pathologic fractures after RT has ranged from 2% to 18% in randomized trials.
Multiple trials have examined various fractionation schedules for the treatment of painful bony metastases. In the Radiation Therapy Oncology Group (RTOG) 74-02 trial patients with bone metastasis were randomized to receive one of several radiation treatment plans with 15 to 40.5 Gy delivered in 5 to 15 fractions. All schedules were equally effective in relieving pain. However, this trial has been widely criticized for the use of physician rather than patient assessment of pain, the inclusion of a wide range of primary sites and histologic types of cancer, and the failure to take narcotic use and incidence of retreatment into consideration.
To address some of these concerns, RTOG conducted trial 97-14, a study limited to patients with breast or prostate cancer, for a more homogeneous patient population, and more sensitive tools were used to assess pain and quality of life. Patients were randomly allocated to receive either a single fraction of 8 or 30 Gy in 10 fractions over 2 weeks. At 3-month follow-up, a complete response as measured by pain control was achieved in 15% and 18% of patients in each arm, respectively ( p = .6), and a partial response in 50% and 48% of patients, respectively. At 3 months, 33% of patients in both arms no longer required narcotic analgesics. There was no difference in the rate of pathologic fractures within or adjacent to the treatment field (5% and 4%, respectively). A significant difference between the two arms was observed in the rate of retreatment with twice as many patients in the 8-Gy arm receiving retreatment (18%) compared with the 30-Gy arm (9%). This discrepancy in retreatment rates has been found in numerous other studies comparing single-fraction to multiple-fraction regimens and is believed to be related to physician willingness to retreat patients who initially receive lower doses of RT, rather than differences in efficacy between the two arms, which are generally otherwise identical.
Wu and associates at McMaster University performed a meta-analysis of dose-fractionation trials for the palliation of painful bone metastases. They divided the studies into three groups: two trials comparing 4 Gy with 8 Gy, each given in a single fraction; eight trials of single-fraction versus multiple-fraction regimens; and six trials comparing different multifraction regimens. Overall response rates were significantly lower with 4 Gy compared with 8 Gy, although complete response rates were not significantly different. For the next comparison, 8 Gy was the most common single-fraction dose, and 20 Gy in five fractions or 24 Gy in six fractions were the most common schedules for the multifraction arms. The pooled intention-to-treat complete response rates were 33.4% for single-fraction treatment versus 32.3% in patients receiving a multifractionation treatment schedule ( p = .04). Overall response rates, 62.1% versus 58.7%, also favored single-fraction treatment ( p = .04). No significant differences were found in response rates between the various multifraction regimens. The median duration of response and toxicity profile were also comparable between regimens.
Although there appears to be an equivalent pain response after single-fraction or multifraction RT, several studies suggest that other adverse events, including fracture rates and need for salvage surgery, may be more frequent with single-fraction RT schedules. The Dutch Bone Metastasis Study Group conducted a phase III randomized trial comparing single-fraction 8-Gy treatment to a multifraction regimen of 24 Gy in six fractions in 1171 patients with bone metastases. There was no significant difference between the two arms with respect to pain relief, analgesic use, or toxicity. However, more fractures occurred in the single fraction arm compared with the multifraction arm (23% vs. 7%, respectively), and the median time to fracture was delayed in the multifraction arm. Similarly, in a retrospective series of patients receiving RT for uncomplicated spine metastasis without spinal cord compression or prior radiation or surgery, the rate of spinal adverse events (symptomatic vertebral body fracture, hospitalization resulting from uncontrolled pain at the previously irradiated spine site, interventional procedures for pain control at the spine site, salvage spinal surgery, new or deterioration in neurologic symptoms, or cord or cauda equina compression) were 6.8% versus 3.5% at 30 days, 16.9% versus 6.4% at 90 days, and 23.6% versus 9.2% at 180 days for single fraction versus multifraction, respectively. Thus, although multifraction schedules are less convenient and more costly, they are appropriate for select patients, especially those with prolonged life expectancies.
Stereotactic body RT (SBRT) is an emerging method for the treatment of select patients with bone metastases. SBRT allows the delivery of a targeted ablative radiation dose in up to five fractions with subcentimeter precision. SBRT is useful for treating metastases to the spine, particularly in patients who have had prior radiation to the maximum allowable spinal cord dose, because it minimizes further irradiation of the spinal cord. In patients with metastatic breast cancer, SBRT often results in excellent pain control and local tumor control otherwise unavailable from simple (two-field) external beam radiation approaches. However, the use of spinal SBRT may be associated with an increased risk of vertebral compression fracture, with the greatest risk observed in those treated with a single fraction of 20 Gy or greater and those with a baseline fracture, lytic tumor, or spinal deformity. SBRT is being compared with traditional external beam radiation for the treatment of localized spinal metastases in the RTOG 0631 trial. SBRT is not suitable for patients with a limited life expectancy, extensive metastatic disease, or symptomatic spinal cord compression due to bone metastasis.
Postoperative Radiotherapy
When prophylactic surgery is necessary for stabilization, it should be performed before RT. Postoperative radiation should consider the nature and extent of the surgery when determining areas for treatment and at risk for recurrence. For example, the placement of an intramedullary fixation device or a long-stemmed cemented prosthesis exposes the entire intramedullary canal to tumor. In addition, tissue in the operative field can be contaminated with microscopic tumor. Thus radiation therapy for such a patient would be directed to all exposed regions and extend the full length of the involved bone. When RT is given without surgical stabilization, the risk of fracture in the short term may increase as a result of radiation-induced hyperemic response at the tumor periphery, which can weaken the adjacent bone. Therefore the bone should be mechanically protected until adequate healing has occurred. Crutch walking is recommended if the lesion is in the lower extremity and should continue until pain resolution and a favorable response is observed on radiograph.
Side Effects
External-beam RT is well tolerated with side effects most frequently related to the treatment field. Nausea and vomiting can occur if the stomach is in the radiation field and can be minimized with prophylactic antiemetics. A “flare” reaction, or temporary increase in pain at the site of metastases, occurs in up to 40% of patients after external-beam radiation. A phase III trial in patients with solid tumors undergoing single-fraction RT for painful bony metastasis randomized patients to 8 mg dexamethasone daily for 5 days starting 1 day before radiation therapy. Steroid treatment decreased the incidence of a painful flare reaction to 26% compared with 35% in the placebo group ( p = .05).
Other radiation-induced effects include skin reactions, which may require topical therapy, and edema when treating extremity lesions, which can be minimized by sparing a strip of soft tissue from the radiation portal. RT can also reduce osteoclast activity, causing brittle bones and potentially increasing the risk of fracture. However, differentiating a radiation-induced fracture from a pathologic fracture can be challenging in patients with metastatic bone disease.
Retreatment With Radiotherapy
For patients with recurrent pain stemming from bone metastases previously treated with RT, there are no standard guidelines regarding retreatment. Patients who responded to an initial course of RT are more likely to respond to reirradiation; however, a proportion of nonresponders may also respond. Several randomized trials comparing single-fraction RT to multifraction RT have shown higher retreatment rates in the single-fraction arms. However, many physicians are reluctant to retreat after multifraction RT due to concerns regarding excess toxicity—namely, fracture.
The National Cancer Institute of Canada Clinical Trials Group completed a prospective randomized study (NCIC CTG SC20) of reirradiation in patients with solid tumors metastatic to bone including prostate, breast, and lung cancer. Eight hundred and fifty patients were randomized to a single dose of 8 or 20 Gy in five daily fractions. The primary end point of the study was overall response rate at 2 months using the International Consensus schema, which combines the Brief Pain Inventory worst pain score (0–10 scale) with change in opioid analgesic use (using oral morphine equivalents). In the intent-to-treat analysis, the 2-month response rate was 28% with 8 Gy and 32% with 20 Gy ( p = .2). There was a nonsignificant increased rate of pathologic fractures in the group treated with 8 Gy compared with 20 Gy, with 30 (7%) versus 20 (5%) pathologic fractures and 7 (1.6%) versus 2 (0.5%) spinal cord compression events, respectively. No difference in quality of life, as measured by the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire C30 scale, was observed between the arms suggesting reirradiation is a safe and effective option for select breast cancer patients with recurrent painful metastases. SBRT is an appealing option in patients requiring retreatment as it minimizes reirradiation of normal tissue. However, large clinical trials to guide its use are lacking.
Radiopharmaceuticals
Radiopharmaceuticals are intravenously administered radioactive agents that localize preferentially to reactive bone sites leading to the delivery of therapeutic radiation doses to multiple sites of bony metastatic disease simultaneously. Strontium-89 (Sr 89 ) and samarium-153 (Sm 153 ) emit beta particles and are the two most studied agents. Most randomized trials evaluating Sr 89 studied patients with prostate cancer; however, one small trial compared Sr 89 to rhenium-186 in patients with metastatic breast cancer. The primary end point of the study was pain palliation as assessed by the Wisconsin pain test at 2 months. Thirty-two percent of patients in both arms achieved a complete response in pain. In a study of Sr 89 that included patients with various tumor types, the overall response rate for pain palliation in patients with breast cancer was 64%. Several randomized trials of Sm 153 in patients with bone metastases from a variety of tumor types, including breast cancer have similarly shown high response rates (50%–95%). The primary toxicity associated with radiopharmaceutical administration is hematologic with grade III/IV thrombocytopenia reported in up to 32% of patients, and grade III/IV leukopenia reported in up to 14% of patients receiving radiopharmaceuticals as single agents and in up to 45% of patients when combined with chemotherapy. Blood counts usually return to baseline levels 8 to 12 weeks after administration. In the United States, Sm 153 is approved for the relief of pain in patients with confirmed osteoblastic bone lesions that enhance on radionuclide bone scan, whereas Sr 89 is approved for the relief of bone pain in patients with painful skeletal metastases.
Radium-223 (R 223 ), the first in class alpha particle emitter, deposits high-energy radiation over an extremely short range (60–100 µm) to minimize toxicity to normal bone marrow while still providing therapeutic doses of radiation to the tumor cells. Radium-223 (R 223 ) has been approved by the US Food and Drug Administration for treatment of men with castration-resistant prostate cancer, symptomatic bone metastases, and no known visceral metastatic disease. There are limited case reports and small series regarding the use of R 223 in patients with hormone-refractory bone-dominant metastatic breast cancer showing improvements in pain, evidence of biological activity in bone metastases, and a favorable safety profile in this patient population.
Data on integrating radiopharmaceuticals with other treatments for bone metastases such as osteoclast inhibitors, chemotherapy, and external-beam RT are limited. Although radiopharmaceuticals appear to effectively palliate bone pain in breast cancer, the relative infrequency of bone-only metastatic disease in breast cancer compared with prostate cancer, the fear of potential marrow toxicity, and the plethora of other treatment options often limits this approach to breast cancer patients who refuse chemotherapy or with poor performance status and comorbidities that limit other treatment options.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree