Introduction
The long-term complications of diabetes are generally classified as:
- Macrovascular disease: cardiovascular disease, cerebrovascular disease, and peripheral vascular disease. These are common in Type 2 diabetes and are often present at diagnosis. Type 2 diabetes is often preceded by the metabolic syndrome, which confers a high level of cardiovascular risk. Significantly, myocardial infarction is often ‘silent’ and sudden.
- Microvascular disease: nephropathy and retinopathy. These are a major concern in Type 1 diabetes but the rate macrovascular disease risk is also increased.
- Neuropathy: peripheral, which predominantly affects the feet and legs and autonomic, which can lead to gastroparesis, erectile dysfunction (ED), and hypoglycae-mic unawareness.
These conditions are inter-related and often occur concomitantly. For example, ED has vascular and nerve components. In the long term in the presence of persistent hyperglycaemia, diabetes can affect almost all body systems and is associated with a number of other disease processes, especially Type 2 diabetes where there is an association between obesity, some cancers, and sleep apnoea. Diabetes is also associated with a range of musculoskeletal diseases, osteoporosis, depression, and dementia although the causal links are not clear in all cases. The presence of other concomitant and age-related diseases such as arthritis contribute to reduced quality of life and depression and inhibit self-care.
Thus, a multifactorial approach to managing diabetes complication risk is needed and encompasses regular systematic, individualised risk assessment processes, effective self-care, optimising physical and mental health and diabetes education to prevent the morbidity and mortality and reduce the health costs associated with diabetes.
Pathophysiology of diabetes complications
It is becoming evident that the pathophysiology of diabetes complications is complex and that glycaemic control is the most important determinant of optimal mitochondrial function and therefore, long-term diabetic complications (Brownlee 2000). Changes in mitochondrial function result in oxidative stress and play a key role in the development and progression of both micro and macrovascular complications associated with diabetes. Thus, maintaining normoglycaemia to preserve normal oxidative mitochondrial function is needed to delay or prevent the progression of complications (Forbes & Cooper 2007).
Increases in HbA1c from normal to 9.5% confer a 10-fold increased risk of micro-vascular disease. The relationship between macrovascular disease and hyperglycaemia is not as clear; for example, only a twofold increase in macrovascular disease risk at the same HbA1c was noted in the UKPDS (UKPDS 1998). This finding might be partly explained by the fact that free fatty acids can also be utilised as fuel for oxidative processes in the mitochrondria.
Hyperglycaemia initiates a cascade of pathological changes that underlie diabetes complications. Glucose is the major source of fuel for energy production by oxidative phosphorylation. Hyperglycaemia has significant effects on metabolic pathways concerned with generating cellular energy especially in the mitochondria. Most cells have the capacity to reduce glucose transport across the plasma membrane into the cytosol to maintain glucose homeostasis in the presence of hyperglycaemia. However, some cells are not able to adapt and reduce glucose transport sufficiently to prevent intercellular changes in glucose concentration. The cells are at particular risk include capillary endothelial cells in the retina, mesangial cells in renal glomeruli, neuronal and Schwann cells in peripheral nerves (Forbes & Cooper 2007).
An increasing body of research suggests reactive oxygen species (ROS) initiate the development of diabetic complications (Nishikawa et al. 2000). ROS are generated by damaged or dysfunctional mitochondria. The antioxidant chain is a complex pathway involving the metabolism of oxygen and the transfer of electrons from glucose and other fuels through the respiratory chain via a complex series of reactions. When excess fuel enters the respiratory chain, the mitochondrial membrane potential is overwhelmed and leaks electrons to oxygen to form superoxide (Nishikawa et al. 2000). However, despite the increasing evidence that ROS plays a role in the pathogenesis of diabetes complications the exact mechanisms are still being determined. Maintaining optimal mitochondrial function appears to be important to reduce the progression of diabetes complications.
Hyperglycaemia contributes to cell death, thickened basement membranes in blood vessels, stiffened vessels and reduces the functionality and structure of resistance vessels (proximal vessels before the blood flows into the capillaries). Calcium-regulated potassium channels are disrupted, which affects smooth muscle cell contraction, which contributes to hypertension. As a result, both under perfusion and over perfusion occur. The myogenic response is lost, so the resistance vessels no longer have the capacity to cope with the increased blood flow. Increased basement membrane dysfunction and reduced nerve fibre density is apparent in impaired glucose tolerance. Micro and macrovascular and endothelial cell damage and reduced lumenal size also occur.
Brownlee (2000) suggested that no ‘unifying hypothesis’ links the four main hypotheses proposed to explain the pathogenesis of diabetic complications shown below, but suggested either redox changes in the polyol pathway, or hyperglycaemia-induced formation of ROS, may account for all the underlying biochemical changes.
CARDIOVASCULAR DISEASE AND DIABETES
- Cardiovascular disease is a leading cause of death in people with diabetes.
- People with diabetes need to be treated as if they have heart disease, especially Type 2 diabetes.
- Chest pain may be atypical in people with diabetes.
- Watch for weakness, fatigue, increased blood glucose, congestive cardiac failure (CCF).
- Counsel about how to reduce cardiac risk factors.
- Smoking increases micro-and macrovascular damage. Smoking cessation is imperative.
- Depression is common.
- Transient ischaemic attacks (TIA) may indicate impending stroke.
Rationale
Diabetes is a significant risk factor for cardiovascular disease, for example, coronary heart disease, cardiomyopathy, peripheral vascular disease and stroke (Australian Institute of Health and Welfare (AIHW) 2007). Cardiovascular disease is a major cause of hospital admissions and mortality in people with diabetes. It is often associated with other vascular disease and depression. Complex metabolic abnormalities are present and the need for surgical intervention is high. Autonomic neuropathy can give rise to atypical presentations of cardiovascular disease and heart attack and lead to delayed treatment.
The major clinical manifestations of cardiovascular disease involve:
- The heart and coronary circulation
- The brain and cerebral circulation
- The lower limbs – peripheral vascular disease.
Cardiac disease is a common complication of diabetes, and carries a higher mortality rate than for people without diabetes. The World Health Organisation (WHO) (2003) estimated ~16.7 million people die from cardiovascular disease each year. Myocardial infarction may be a diabetes risk equivalent in non-diabetics. Diabetes often occurs within 3.5 years of an infarct particularly in older people, those with a high BMI, hypertension and smokers. Risk is lower in people consuming a Mediterranean diet and those on lipid-lowering medicines (Mozaffarian et al. 2007).
There is an association among increasing age, duration of diabetes, the presence of other complications and mortality. Cardiac disease is associated with diffuse atherosclerosis, coexisting cardiomyopathy, autonomic neuropathy, hyperglycaemia and hyperlipidaemia, the metabolic consequences being hypercoaguability, elevated catecholamines and insulin resistance. Atherosclerosis is more frequent and more severe in people with diabetes. It occurs at a younger age than in people without diabetes and is more prevalent in women.
Cardiac disease accounts for >50% of deaths in Type 2 diabetes (Standl & Schnell 2000; Huang et al. 2001) and half of these people die before they reach hospital. The mortality rate has not been reduced despite new therapeutic measures and preventative health programmes.
A number of clinical trials demonstrate the importance of reducing lipids, blood pressure, and blood glucose to reduce the risk of cardiovascular disease (Hansson et al. 1998; UKPDS 1998). Hypertension leads to thicker, less elastic blood vessel walls and increases the strain on the heart. There is a linear relationship between the diastolic blood pressure and the eventual outcome of Type 2 diabetes. Reducing the blood pressure below 90 mmHg significantly improves the outcome (UKPDS 1998).
Subtle changes occur in the heart as a result of ischaemia-induced remodelling and the effects of hyperglycaemia on the endothelium of large blood vessels that predispose the individual to heart failure (Standl & Schnell 2000). Heart muscle metabolism is critically dependent on glucose during ischaemia, and heart muscle performance is improved in the presence of insulin, which stimulates glucose uptake, which support the use of IV insulin in acute myocardial infarction (Malmberg et al. 1995). However, impaired heart performance is multifactorial and blood pressure, lipids, and prothrombin imbalance all play a part.Table 8.1 outlines some of the diabetic-specific abnormalities linked to the development of cardiovascular disease.
Table 8.1 Diabetes-specific cardiovascular abnormalities that predispose an individual to heart disease.
| Abnormality | Relevance to cardiovascular disease |
| Microvascular disease | Often occurs concomitantly with macrovascular disease Affects nutrient and oxygen exchange Nephropathy, frequently in association with retinopathy |
| Autonomic neuropathy | Postural hypotension Abnormal cardiovascular reflexes Loss of sinus rhythm Resting sinus tachycardia Painless myocardial ischaemia and infarction ‘silent MI’ Delayed recognition and treatment Increased anaesthetic risk Increased risk in critical care situations Sudden death |
| Endothelial damage in basement membrane or outer lining of vessels large blood | Weak vessel walls, stiffened vessels contributing to hypertension Impaired blood flow Reduced tissue oxygenation and nourishment |
| Hypertension | Thickening of blood vessel walls Increased strain on the heart Risk of stroke and MI |
Myocardial infarction is ‘silent’ in 32% of people with diabetes, which leads to delay in seeking medical attention and may be a factor in the increased mortality rate. ‘Silent’ infarct means that the classic pain across the chest, down the arm and into the jaw is absent. Only mild discomfort, often mistaken for heartburn, may be present. The atypical nature of the chest pain may make it difficult for people to accept that they have had a heart attack. Risk factor modification may not be seen as essential. The person may present with hypertension, heart failure, cardiogenic shock or, in the elderly, diabetic ketoacidosis or hyperosmolar coma.
Diabetes may be diagnosed at the time of an infarct or during cardiac surgery. Emotional stress, and the associated catecholamine response, leads to increased blood glucose levels in 5% of patients admitted to coronary care units (CCUs). The blood glucose may normalise during convalescence; however, counselling about diabetes and its management is important especially if other diabetes risk factors are present. Tact and sympathy are necessary when informing the patient about the diagnosis of diabetes in these situations.
Medicines and cardiovascular disease
Many types of medicines are needed to prevent and manage cardiovascular disease (see also Chapter 5). The choice of medicines depends on the clinical indication, patient factors such as contraindications and risk of medicine interactions, availability, and cost. Commonly used medicine types include:
- Antithrombotic medicines to prevent thromboembolism generally and during coronary procedures and surgery, prevent stroke in patients with atrial fibrillation, prevent thromboembolism in patients with prosthetic heart valves, and treat acute MI. Types of medicines include Vitamin K antagonists (warfarin), heparin (enoxaparin), platelet aggregation inhibitors (aspirin), and thrombolytic enzymes (alteplase). These medicines require frequent monitoring and interact with many other medicines including complementary medicines (CAM).
- Cardiac medicines to treat arrhythmias (cardiac glycosides such as digoxin), heart failure antiarrythmics such as amiodarone), relieve cardiac symptoms such as angina (vasodilators such as isorbide), treat high and low blood pressure, cardiogenic shock and MI (cardiac stimulants such as adrenaline).
- Antihypertensive agents often used as primary prevention to reduce the risk of microvascular disease. These include low dose diuretics as first-line treatment (frusemide), peripheral vasodilators (oxpentifylline), calcium channel blockers (amlodipine). Antihypertensive therapy is usually selected according to the comorbidities present to achieve blood pressure 130/80 in people with cardiovascular disease. The first-line medicine for people with diabetes and hypertension is an ACE or an ARB; the most appropriate choice in an older person following a MI is a calcium channel blocker to reduce the risk of stroke, however, most people require several antihypertensive medicines (European Society of Hypertension 2007).
- Beta blocking agents (atenolol, metorpolol, propanolol), which can be used with a diuretic and an ACE inhibitor.
- Medicines acting on the renin–angiotensin system such as ACE inhibitors, which are first-line treatment in heart failure, left ventricular dysfunction following MI, and diabetes in the presence of microalbuminuria (ramipril); angiotensin 11 antagonists (irbesartin), which are used if the person cannot tolerate ACE. For example, ACE inhibitors are associated with a three times higher rate of cough.
- Lipid lowering agents such as HMG-CoA reductase inhibitors (statins, e.g., atorvastatin), which reduces LDL cholesterol, fibrates, which are first choice if triglycerides are elevated, nicotinic acid, which lowers both cholesterol and triglycerides but is not tolerated very well (Australian Medicines Handbook 2006). Ongoing trials using statins include CORONA, GISSI-HF, and UNIVERSE (Leite-Moreira & Castro-Chaves 2008) that will further clarify the place of these medicines in managing heart failure.
However, these medicines are not always prescribed optimally. For example, anithrombotic medicines, ACE inhibitors, ACE, and beta blocker combinations, and antihypertensive agents are under utilised (National Institute of Clinical Studies 2005). Patient non-adherence with many medicines is high and is a significant limiting factor in achieving optimal outcomes.
Complementary medicines (CAM)
Recently, WS 1442, a formula of Crateaegus monogyna (hawthorn) was shown to increase intracellular calcium concentration, contractile force, action potential and the refractory period, improve coronary blood flow and reduce preload and after load (Pittler et al. 2008). Animal studies have also demonstrated a smaller area of infarction after induced MI. These findings suggest WS 1442 may have a place in managing cardiovascular disease, but that place is not yet defined.
Coenzyme Q10 (CQ-10) lowers systolic and diastolic blood pressure and reduces inflammation, suggests individuals with mild-to-moderate hypertension and cardiac disease may benefit from CQ-10 supplements (Rosenfeldt et al. 2007), but like W1442, its place is under researched. CQ-10 is an antioxidant and is present in LDL-c where it reduces the potential for LDL-c to be oxidised and become atherogenic. Some experts suggested CQ-10 might be a useful addition to statins to reduce myotoxicity. However, while it may have a place in some people, at present there is no recommendation to use it in all patients taking statins (Barenholtz & Kohlhaas 2006).
Other complementary therapies such as massage, meditation, and Tai Chi can help reduce stress, improve quality of life and manage pain, see Chapter 19. But should be used within a quality of medicine framework.
Patients with an acute cardiovascular event are usually cared for in CCUs or stroke units, but patients in other wards may develop cardiovascular problems. A longer stay in CCU may be indicated for people with diabetes, because 35% of patients die, often in the second week after the infarct (Karlson et al. 1993). People with diabetes and unstable angina, MI without ST elevation or STEMI have a higher mortality risk within one year of the onset of acute coronary syndrome than non-diabetics (Donahoe 2007).
Silent MI may be relatively common in common critical care settings and the diagnosis can be difficult and is often missed due to analgesia controlling chest pain, intubation, sedation, and coma (Lim et al. 2008). Cook (2008) suggested screening for elevated troponin levels in critically ill patients together with and ECG could reduce mortality and that elevated troponins might be predicative of mortality. Although more research is needed, these findings might be particularly relevant to people with diabetes where the risk of cardiovascular disease is likely to be high.
Short-and long-term morbidity and mortality can be improved by IV insulin/glucose infusion followed by multidose subcutaneous insulin injections (Malmberg et al. 1995). Acute myocardial infarction causes a rapid increase in catecholamines, cortisol, and glucagon. Insulin levels fall in the ischaemic myocardium and tissue sensitivity to insulin falls and impairs glucose utilisation by cardiac muscle. Free fatty acids are mobilised as fuel substrates and potentiate ischaemic injury by direct toxicity or by increasing the demand for oxygen and inhibiting glucose oxidation. IV insulin during acute episodes and subcutaneous insulin for three months after the infarct may restore platelet function, correct lipoprotein imbalance, reduce plasminogen activator inhibitor-1 activity and improve metabolism in non-infarcted areas of the heart.
The need for invasive procedures depends on the severity at presentation and the results of relevant investigations. Pfisterer (2004) showed invasive treatment provided short-term symptomatic relief, reduced the rate of revascularisation and hospitalisation and less frequent use of antianginal medicines, compared to medicine treatment. In the longer term, both strategies were effective in older patients with angina. Mortality risk factors included age >80 years, prior heart failure, left ventricular ejection <45%, and the presence of two or more comorbidities.
Mental health and cardiovascular disease
Anxiety is common among people with cardiac disease and can have serious consequences for self-care and long-term outcomes if it is not recognised and managed to prevent depression. However, anxiety can be life saving if it prompts the person to seek help early (Moser 2007). Significantly depression is an independent risk factor for cardiovascular disease and its prognosis. Both depression and heart disease are associated with social isolation and lack of social support (Bunker et al. 2003). These factors need to be considered when estimating cardiovascular risk.
Several trials have investigated the cardiovascular benefit of treating depression. These include ENRICH (cognitive behaviour therapy and SSRI medicines), which is difficult to interpret but which showed no significant difference between treatment and usual care. SADHART (SSRI), which showed improvements in mild-to-moderate depression but no significant differences in cardiac events. The results of CREATE (SSRI (citalopram) and interpersonal psychotherapy) are not yet available but suggest depression improves but HbA1c does not significantly improve (Reddy 2008).
The effects on mental health may change; for example, Gudjhar & Dunning (2003) found people with diabetes were most concerned about the implications of the MI immediately after the event and less concerned about the impact of diabetes on their long-term physical health, mental health, and quality of life. Patient generated quality-of-life tools were used. As people recovered and realised they would survive, about four months after the MI, concern about the MI began to diminish and pre MI worry about diabetes re-emerged.
Depression may increase cardiovascular risk and vice versa via several mechanisms:
- Risk behaviours such as inadequate diet and inactivity, smoking and non-compliance with medicines.
- Effects on autonomic function by enhancing sympathetic nervous system activity and heart rate variability.
- Consequence Model – Inflammatory processes with sub-chronic elevation of cytokines activate the stress response and inhibit serotonin. MI might also induce physical changes in the brain that are mediated by the inflammatory response and cause depression.
- Coincidence model – autonomic dysregulation decreased heart rate variability and increased risk of ventricular arrhythmias, changes in platelets, inflammation and changes in endothelial function some of which might be linked to dietary factors. For example, increasing omega-3 fatty acids improves cardiac function (Lesperance & Frasure-Smith 2007).
Objectives of care in hospital
Nursing care should be planned to avoid constantly disturbing the patient and allow adequate rest and sleep. The objectives of care are to:
- Treat the acute attack according to medical orders and standard protocols.
- Stabilise cardiac status and relieve symptoms.
- Prevent extension of the cardiac abnormality and limit further episodes.
- Retain independence as far as possible.
- Achieve and maintain euglycaemia.
- Provide psychological support.
- Prevent complications while in hospital.
- Counsel about risk factor modification.
- Educate/re-educate about diabetes.
Nursing responsibilities
- Many patients on OHAs are changed to insulin during the acute phase to improve blood glucose control.
- Insulin is usually administered via an infusion at least for the first 48 hours. Only clear insulin is used. Insulin infusions are discussed in Chapter 7. The patient should be eating and drinking normally before the infusion is removed, and a dose of subcutaneous insulin given to prevent hyperglycaemia developing.
- increase blood glucose levels.
- cause hypokalaemia.
- Beta blockers reduce mortality by >30%. Ace inhibitors improve blood pressure and cardiac remodelling and stabilise the rate of progression of renal disease. There is a close association between cardiac and renal disease in diabetes.
- Monitor fluid balance and maintain accurate charts, to help assess kidney function.
- Monitor blood pressure, lying, and standing. Some antihypertensive medications can cause orthostatic hypotension. Counsel the patient to change position gradually, especially on getting out of bed or out of a chair.
- Monitor ECG.
- Observe for weakness, fatigue, CCF or unexplained hyperglycaemia, which may indicate a further infarct.
- Provide appropriate skin care to prevent dryness and pressure areas.
- Monitor serum electrolytes, cardiac enzymes, blood gases and potassium levels. Report abnormalities to the doctor promptly. Fluctuating potassium levels can cause or exacerbate cardiac arrhythmias.
- Prevent hypoglycaemia by careful monitoring of blood glucose and carbohydrate intake.
In many cases previous metabolic control was suboptimal and insulin therapy indicated for some time before the infarct occurred.
Some OHAs are contraindicated if cardiac, renal, and/or liver disease is present (see Chapter 5).
- Autonomic neuropathy is present.
- Non-selective beta-blocking agents are used.
Medical tests/procedures (see Chapter 9)
Rehabilitation
Structured rehabilitation after an acute cardiovascular event and heart failure improves long-term outcomes, reduces social isolation, and improves function and quality of life.
- Recognition of hypoglycaemia.
- Correct insulin technique.
- Correct blood glucose monitoring technique.
- Possible indicators of further cardiac problems.
- Dietary assessment and advice.
- Risk factor modification.
Modifying risk factors associated with the development of cardiac disease
Current cardiovascular management guidelines focus on reducing global cardiovascular risk, which requires a proactive approach and attention to multiple risk factors taking age into account. Cardiovascular risk can be stratified and individualised to enable personalised teaching using tools such as the QRISK and ASSIGN in the UK and the Framingham algorithm, which is sex-specific and is based on the presence of hypertension, dyslipidaemia, and smoking. The Systematic Coronary Risk Evaluation (SCORE) based on cholesterol, blood pressure, and age was developed for European countries (Zannad 2008). Significantly, research suggests that doctors do not adequately assess cardiovascular risk and this contributes to patients not achieving management targets (Bohm 2008). Other researchers found general practitioners overestimate the risk of diabetes complications but the impact on patient care and service utilisation or outcomes was not reported (Haussler et al. 2007).
Patients require both information and support to manage diabetes and reduce the risk of adverse health outcomes. Personalised information is more effective than generalised information. Management targets are described in Chapter 2. As indicated in Chapter 16, helping people determine their cardiovascular age could be a useful way to help people understand their cardiovascular risk and enhance their adherence to risk reduction strategies.
Key messages are to:
- Stop smoking.
- Avoid high calorie foods and high fat intake especially trans fats to achieve sensible weight reduction. Include omega-3 fatty acids in the diet. Reduce salt intake. Suitable diets are described in Chapter 4 and include the DASH and Mediterranean diets
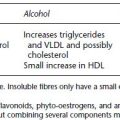
- Limit alcohol intake.
- Maintain a healthy weight range suitable to age and developmental stage. In particular reduce abdominal obesity.
- Increase regular exercise/activities.
- Achieve acceptable blood glucose levels. However, the ACCORD trial in Type 2 diabetes was halted after 18 months when an interim analysis showed an increased number of deaths in the intensive control versus (HbA1c target <6%) control groups.
- Reduce blood lipids. If this is not achieved by diet and exercise lipid lowering agents are needed, see Chapter 5. High LDL-c, low HDL-c, and mixed hyperlipi-daemia significantly increase the risk of developing cardiovascular disease (Hansel 2007).
- Reduce blood pressure by an appropriate diet and exercise and stopping smoking. Tight blood pressure control is important and people are often prescribed three or more antihypertensive agents. The choice of medication is individualised and includes reducing blood glucose as part of a comprehensive cardiovascular risk management plan (Lowe 2002). Hypertension is also a risk factor for poorer performance on verbal and concept formation tests in Type 2 diabetes (Elias et al. 1997), which has implications for self-care and activities of daily living.
- Secondary prevention programmes such as cardiac rehabilitation are important to help individuals regain the best possible functioning.
- Manage stress. Long-term stress is associated with increased risk of cardiovascular disease in both men and women and high level of trait anger in middle aged men with hypertension is associated with increased risk of hypertension progression to a cardiovascular event (Player et al. 2007).
- Seek treatment for depression.
- Patients with known cardiac disease should have a written action to plan to follow if they experience chest pain. They should know early management is important and not to delay presenting to hospital. The plan might include using short-acting nitrate medicines, resting, taking aspirin if they are not already prescribed this medicine, calling an ambulance, notifying their doctor, and wearing medic alert information.
Telephone coaching
Telephone coaching patients with coronary heart disease and suboptimal lipids improves adherence to medication therapy and dietary advice. It contributes to an improved lipid profile and could be an important aspect of cardiac rehabilitation programmes (Vale et al. 2002). The COACH protocol is currently under investigation in a general practice setting with practice nurses providing coaching with support for the COACH investigators (Young et al. 2007).
Cerebrovascular disease
The brain is supplied with blood by four main arteries: two carotids and two vertebral arteries. The clinical consequences of cerebrovascular disease depend on the vessels or combination of vessels involved.
Transient ischaemic attacks (TIAs) arise when the blood supply to a part of the brain is temporarily interrupted without permanent damage. Recovery from a TIA usually occurs within 24 hours. If TIAs occur frequently they can indicate impending stroke. Small repeated strokes that cause progressive brain damage can lead to multi-infarct dementia, which is common in diabetes. Signs that this is occurring are:
- Gradual memory loss.
- Diminished intellectual capacity.
- Loss of motor function.
- Incontinence.
Strokes are classified as thrombotic or haemorrhagic and occur when a major vessel is blocked. They frequently cause permanent damage requiring prolonged rehabilitation and often significantly reduced self-care potential and quality of life. In these cases diabetes management should be discussed with the family or carers who will be responsible for assisting the person with diabetes.
The risk factors for cerebrovascular disease are similar to those for cardiovascular disease. High BMI >25 kg/m2 and systolic hypertension increase risk of death after a stroke among men (Chen 2008). However, there appears to be some significant differences between man and women. Women may have worse outcomes after acute stroke than men if they do not receive thrombolytic therapy and women are more likely to benefit from thrombolytic therapy than men (Lutsep 2008). Likewise, healthy women over age 65 benefit from alternate day aspirin (100 mg) to prevent stroke but aspirin has not been shown to prevent strokes in healthy men (Ridker et al. 2005).
There are also gender differences in response to treatment and outcome following acute stroke. Women with carotid artery stenosis have a lower risk of recurrent stroke than men and receive less benefit from surgical treatment of moderate carotid artery stenosis than men (Alamowitch et al. 2005). Women with intracranial stenosis are at higher risk of recurrent stroke than men (Williams et al. 2007).
Poor sleep quality is also linked to increased risk of vascular events including stroke and daytime sleepiness may be an independent risk factor for stroke conferring a 4.5-fold increased risk (Boden-Albala 2008).
Signs and symptoms
- A careful history will elicit failing mental function.
- Carotid bruits are usually present and can be evaluated using Doppler studies.
- Angiography is required in symptomatic cases.
Management
The preventative measures outlined for cardiovascular disease apply to cerebrovascular disease. Carotid endarterectomy is indicated if the carotid arteries are significantly narrowed. Low-dose aspirin may be beneficial.
Nursing responsibilities include care during investigative procedures (see Chapter 9). Rehabilitation focuses on returning the person to optimal functioning and independence within their capabilities.
Driving assessment needs to be undertaken and assessed regularly, see Chapter 10.
DIABETES AND EYE DISEASE
- Encourage independence. People with visual loss are capable of caring for themselves if they are provided with appropriate tools and information. However, visual impairment has a profound impact on an individual’s ability to learn diabetes self-care tasks and on their psychological wellbeing.
- Maintain a safe environment.
- Orient patient to the environment and staff.
- Explain procedures carefully and fully recognising the person is not a visual learner
- Return belongings to the same place.
- Use appropriate teaching style to the individual’s learning style.
Rationale
Retinopathy is a significant complication of diabetes. Prevention and early identification of people at risk are essential. Nurses need to be aware of the impact of visual loss on the self-care and psychological wellbeing of people with diabetes and their role in preventative care. Other vision changes occur in people with diabetes in addition to diabetic retinopathy, for example, macular degeneration is common in older people. Age-related macular degeneration might be related to elevated levels of high-sensitivity CRP. Cataracts and glaucoma have a higher incidence in diabetes but also occur in non-diabetics.
Introduction
Visual impairment and blindness are significant complications of diabetes. The specific cellular mechanisms that lead to reduced visual acuity have not been defined. (Antonetti et al. 2006) proposed a combined nerve and vascular mechanism that causes loss of neurons, which compromises neurotransmission and altered structure and function of retinal cells types. Macular cysts could scatter light and reduce the quality of the image and/or visual function could decline as a result of fluid accumulation in the retina. The neurons are susceptible to circulating amino acids, antibodies and/or inflammatory cells that reach the retina through leaking capillaries. The vascular leakage can affect vision even when macular oedema is not present (Antonetti et al. 2006). There is also evidence that cognitive ability declines over time in people with diabetes and may be linked to complications such as proliferative retinopathy (Ryan et al. 2003).
Key changes in the eye include:
- Maculopathy: macular oedema and macular ischaemia. The macular may be distorted or elevated or vitreous haemorrhages may occur and distort the ocular media (Antonetti et al. 2006).
- Retinopathy – stages of retinopathy have been described based on a system of photographic grading that requires comparison with a standard set of photographs showing different features and stages of retinopathy (DRS 1981; EDTRS 1991)
- Generalised ocular oedema
- Lens opacity – cataract
- Papillopathy – optic disc swelling that occurs in Type 1 diabetes.
Retinopathy occurs in almost all people with Type 1 diabetes after 20 years duration of diabetes and 70% of people with Type 2 diabetes (DRS 1981; DCCT 1993). Retinopathy occurs as a result of microvascular disease that manifests as increased capillary permeability and closure of the retinal capillaries, which causes vascular leakage, retinal oedema, and accumulation of lipids that is seen as hard exudates in the retina and retinal ischaemia.
Risk factors for retinopathy
The factors that lead to an increased risk of retinopathy include:
- Long duration of diabetes.
- Poor metabolic control.
- Renal disease.
- Pregnancy in people with diagnosed diabetes. Pregnancy may exacerbate existing retinopathy, see Chapter 14 (but it does not usually develop in women with gestational diabetes).
- Smoking.
- Hypertension.
People with diabetic eye disease are at greater risk of developing other diabetes-related complications unless they are screened regularly, take appropriate preventative action and treatment is commenced early.
Visual impairment from non-diabetic causes can coexist with diabetes. People with diabetes also have an increased incidence of glaucoma and cataracts and there is an increasing correlation with age-related macular degeneration. Many of the underlying causes that lead to macular degeneration are also associated with diabetes, seeTable 8.2. Poor vision can be a significant disadvantage during diabetes education and general living because most diabetic and general health information contains essential visual components (IDF-DECS 2000).
Table 8.2 Risk factors for age-related macular degeneration (Lim 2006). Many of these are similar to the risk factors for diabetic retinopathy and the same risk reduction strategies apply to both conditions. The table shows modifiable and non-modifiable factors. Sun exposure, and iris and hair colour do not appear to be associated with AMD (Khan et al. 2006).
| Modifiable factors | Non-modifiable factors |
| Cigarette smoking, the risk increases with long duration of smoking. | Increasing age: for both exudative and non-exudative AMDa |
| Diet high in fats especially monounsaturated and polyunsaturated fats. Linoleic acid increases the risk for advanced AMD. | Ethnicity. AMD is more prevalent in whites.Especially for the components of late AMD, increased retinal pigmentation and retinal pigment epithelial depigmentation. Cataracts and glaucoma are more common in Blacks. |
| Omega-3 fatty acids are associated with lower risk. | |
| High GIb foods is related to the development of retinal pigmentation abnormalities (Chui et al. 2006). Emerging research suggests a diet rich in fruit and vegetables especially carotenoids may help prevent AMD. Vitamins C and E and zinc (van Leeuwen et al. 2005) | |
| High BMIc. The risk of developing AMD increases with increasing BMI and geographic atrophy could be associated with high BMI, low education and antacid use (Clemons et al. 2005). | Genetic inheritance |
| Hypertension is associated with exudative AMD but not non-exudative AMD | |
| Hypercholesteraemia is also associated with exudative AMD. | |
| Inflammation. Recent studies suggest C-reactive protein is associated with intermediate and advanced AMD (Seddon et al. 2004). |
a AMD: age-related macular degeneration.
b GI: glycaemic index.
c BMI: body mass index.
Eye problems associated with diabetes
- vitreous haemorrhage
- retinal detachment
- retinal artery occlusion.
- good blood glucose control can slow the rate of progression in Type 1 diabetes (DCCT 1993)
- regular eye examinations (commencing at diagnosis in Type 2 and within 5 years in Type 1)
- non-mydriatic fundus photography, as the name suggests, does not require mydriatic eye drops to be used. This means people do not have to wait long periods to have their eyes examined and can drive themselves home after the procedure. The procedure is not painful but the patient should be warned that the flash of light is very bright. Retinopathy screening committees in both Australia and the UK recommend indirect fundoscopy and digital photography to screen for retinopathy
- retinal photography
- confocal microscopy is increasingly being applied to diabetes complication screening, especially to detect eye changes and neuropathy. Confocal microscopy enables greater contrast to be achieved and three-dimensional images to be created that show great detail. The technique uses a spatial pinhole to eliminate out of focus light and flare. It enables faster diagnosis, is non-invasive and painless.
- fluorescein angiography.
Resources for people with visual impairment
People with significant visual loss often require assistance to perform blood glucose monitoring and to administer their own insulin. It is important to encourage independence as far as possible. Careful assessment is important and should include assessment of the home situation.
Vision Australia and the Royal National Institute for the Blind in the UK offer a variety of services for people who have degrees of visual loss. These services include:
- Assessment of the home situation to determine if modifications are necessary to ensure safety at home.
- Low vision clinics.
- Talking library and books in Braille.
- Training on how to cope in the community with deteriorating vision.
Other help includes:
- Services such as pensions, which may be available from the government.
- Seeing eye dogs (guide dogs for the blind).
- A range of diabetes products are available that can help visually impaired people remain independent (see next section).
The community nurses and home-based services play a major role in maintaining visually impaired people in their own homes.
Aids for people with low vision
Various magnifying devices are available to help people continue to care for themselves. They can be obtained from diabetes associations and some pharmacies specialising in diabetic products. Other aids include:
- clicking syringes, Instaject devices, clicking insulin pens
- chest magnifying glass (available from some opticians); Magniguide – fits both 50 and 100 unit syringes and enlarges the markings
- location tray for drawing up insulin if syringes are used.
- strip guides for accurate placement of the blood onto the strips
- talking blood glucose meters, blood pressure monitors, and talking weight scales
- meters with large result display areas.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree