Rationale
Proactive monitoring programmes enable blood glucose and lipid patterns, complication status, and self-care ability to be identified and the management regimen appropriately tailored to the individual. The accuracy of the self-testing technique and appropriate maintenance of equipment is an important aspect of the individual’s ability to manage their diabetes and helps ensure management decisions are based on the best available data when used in conjunction with laboratory investigations and physical and mental assessment Self-monitoring enables people with diabetes to identify the effects of diet, exercise and other factors on their blood glucose levels, and gives them greater insight into and control over their disease.
Introduction
Monitoring blood glucose is an important part of diabetes management. The results obtained form the basis for adjusting medication, food intake, and activity levels. Urine glucose is not a reliable method of assessing metabolic control, but might still be useful for some people and in some countries where no other method is available provided the renal threshold for glucose has been established. Most glucose circulating in the blood is reabsorbed in the renal tubules, however, the capacity to reabsorb glucose is exceeded during hyperglycaemia and glucose appears in the urine. The renal threshold for glucose is fairly constant, about 10 mmol/L, but may be higher in older people and during pregnancy (Sonksen et al. 1998). Glucose in the urine represents the amount of glucose that collects in the urine since the bladder was last emptied and is therefore, a retrospective value.
People with diabetes are expected to manage their diabetes at home. They should be encouraged to continue to self-monitor in hospital if they are well enough to do so. If health professionals perform the test they should always inform the patient of the result of their blood glucose test unless they are too ill to understand the information. Blood glucose testing time can be used as teaching time.
The results of blood and urine tests are useful only if tests are accurately performed.
The following section explores monitoring blood glucose.
Monitoring 1: blood glucose
- Follow correct procedure when performing tests.
- Perform meter control and calibration tests regularly.
- Clean and maintain equipment regularly.
- Record and interpret results according to the clinical situation.
The role of blood glucose monitoring in the care of diabetes
Blood glucose monitoring provides insight into the effectiveness of the diabetes management plan. It enables direct feedback to the patient about their blood glucose.
Some experts suggest the cost and time associated with self-blood glucose monitoring is not cost effective, even when patients are taught to adjust their management regimen. For example, the DiGEM investigators undertook a randomised control trial involving people with treated Type 2 diabetes over age 25 treated with diet or OHAs and showed no statistically significant difference in HbA1c at 12 months but there was a significant change in total cholesterol (Farmer 2007). Subjective parameters such as quality of life and sense of control were not measured. Other researchers also show that people who monitor their blood glucose are younger at diagnosis and present with a higher HbA than people who do not test (Franciosi et al. 2005; Davis et al. 2006).
In contrast, the ROSSO study (Schneider et al. 2006) showed metabolic control improved in people with Type 2 diabetes who performed frequent blood glucose tests, and demonstrated a 51% lower risk of death and a 32% lower risk of micro and macrovascular complications. In addition, people who monitored were more aware of their blood glucose levels and sought advice from health professionals sooner. Likewise, Karter et al. (2006) demonstrated improved HbAlc after home blood glucose testing was instituted in the Kaiser Permanente study.
Other researchers have shown lower rates of self-blood glucose monitoring in men and those with low education level, those who do not have health insurance, in countries where equipment is not subsidised, as well as those not on insulin, those taking OHAs, having less than two consultations with the doctor annually, and not attending diabetes education programmes (Centers for Disease Control and Prevention (CDC) 2007).
These studies suggest there may be gender and age differences in the rates of selfblood glucose monitoring but the rates are similar in different countries. Nevertheless, most management guidelines continue to recommend self-blood glucose testing as an integral part of the management plan. Testing frequency should be individualised depending on glycaemic control and health status in Type 2 diabetes but at least daily when insulin and/or OHAs are used. People with Type 1 should monitor at least TDS (Canadian Diabetes Association).
Blood glucose testing is performed to:
- Monitor the effectiveness of diabetes therapy and guide adjustments to the food plan, OHAs/insulin dose, exercise/activity, mental well being and quality of life, see Chapter 2.
- Detect hyperglycaemia, which can be confirmed by laboratory blood glucose tests and elevated HbA1c levels, a marker of the average blood glucose over the preceding three months, and more recently, A1c-derived average glucose.
- Achieve blood glucose targets, which has a role in preventing or delaying the onset of diabetes-related complications and maintaining independence and quality of life.
- Diagnose hypoglycaemia, including nocturnal hypoglycaemia, which can present as sleep disturbances, snoring, restlessness or bad dreams.
- Establish the renal threshold for glucose to determine the reliability of urine testing in those rare cases where people still test their urine glucose.
- Achieve ‘tight’ control in pregnancy and thereby reduce the risks to both mother and baby.
- Provide continuity of care following hospitalisation.
Blood glucose monitoring is of particular use in:
- Frequent hypoglycaemic episodes and hypoglycaemic unawareness.
- Unstable or ‘brittle’ diabetes.
- Managing illnesses at home and when recovering from an illness.
- GDM, pregnancy and in neonates born to women with GDM and diabetes.
- Establishing a new treatment regimen.
- Stabilising OHA and/or insulin doses.
- Patients with renal failure, autonomic neuropathy, cardiovascular or cerebrovascular insufficiency where hypoglycaemia signs can be masked or not recognised.
- During investigations such as angiograms and surgical procedures.
- Detecting actual or potential medicine/medicine or medicine/herb interactions.
- During travel.
- Patients with renal failure, autonomic neuropathy, cardiovascular or cerebrovascular insufficiency where hypoglycaemia signs can be masked or not recognised.
The target blood glucose range and frequency of testing should be assessed individually when people with diabetes are in hospital. The aim is to achieve a blood glucose pattern as close to normal as possible. Generally accepted blood glucose targets are: premeal ≤5.5 mmol/L and two-hour post prandial <7.8 mmol/L (IDF 2007). However, the management regimen must target both fasting and post prandial blood glucose to achieve optimal control and reduce the risks associated with hyperglycaemia see Chapters 7, and 8.
Increasing emphasis is being placed on reducing post prandial hyperglycaemia because it is associated with increased risk of retinopathy, cardiovascular disease, increased risk of cancer and impaired cognitive function in older people (IDF 2007). Significantly, elevated post prandial hyperglycaemia is present before Type 2 diabetes is diagnosed and partly accounts for why cardiovascular complications are frequently present at diagnosis. Management of post prandial hyperglycaemia is discussed in Chapters 5 and 8.
Although the focus is on achieving optimal blood glucose control to prevent or delay the onset of diabetes complications, optimal control is often not achieved. The person is usually blamed for not ‘complying’ with recommendations. However, the progressive nature of Type 2 diabetes and clinician inertia also play a part (Grant et al. 2004). Clinical inertia refers to health professionals recognising a problem but failing to act. Like ‘non-compliance’, clinical inertia is a derogatory term for a complex phenomenon where behaviours are influenced by factors such as competing demands in the clinical setting including time constraints and patients presenting with multiple problems that cannot all be addressed at the same time (Parchman et al. 2007). However, clinician inertia combined with patient non-adherence might increase the risk of poor control and may be mutually causative.
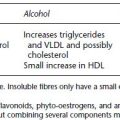
Factors that influence blood glucose levels
Guidelines for the frequency of blood glucose monitoring
The following recommendations are guidelines only; the policies and procedures of the employing institution should be followed.
Suggested protocol in hospital settings. Blood glucose tests performed before meals and before bed (e.g. 7 AM, 11 AM, 4 PM, and 9 PM) in order to obtain a profile of the effectiveness of diabetes therapy. Occasionally, urine glucose will be measured at these times for 24 hours to establish the renal threshold. As indicated, testing 2 hours after food, especially in Type 2 diabetes, may be preferable to provide information about glucose clearance from the blood stream after a meal as an indicator of cardiovascular risk. Blood glucose tests may be performed at 2 AM or 3 AM for two to three days if the blood glucose is high before breakfast and there is a possibility of nocturnal hypoglycaemia, see Chapter 6.
Blood ketones should be monitored in all patients with Type 1 diabetes and in Type 2 people during severe stress, for example, surgery, infection, and myocardial infarction if blood glucose tests are elevated. Urine ketone tests might still be used in some places but are a less reliable indicator of ketosis than blood ketones. Each person’s needs should be assessed individually and the testing schedule tailored to individual requirements where work routines and staffing levels allow. One way to achieve an individualised monitoring regime is to allow the patient to perform their own blood glucose tests where their condition permits them to do so.
Regimen for patients on insulin. Initially, for 48 hours, monitor at 7 AM, 11 AM, 4 PM, and 9 PM to assess the effectiveness of the prescribed insulin therapy. Review after 48 hours and alter testing frequency if indicated. If the insulin regimen is altered, review again after 48 hours.
Note: The timing of blood glucose monitoring depends on the insulin regimen and the action profile of the prescribed insulin see Chapter 5.
Patients using insulin pumps and those on IV insulin infusions require more frequent monitoring.
Patients on oral hypoglycaemic agents. Initial monitoring as for insulin-treated patients. Review after 48 hours and reduce monitoring frequency to twice daily, daily or once every second or third day, alternating the times of testing, as indicated by the level of control and the general medical condition of the patient.
Patients using diet and exercise. Initially, twice daily monitoring, decreasing to daily or once every second or third day, unless the patient is having total parenteral nutrition (TPN), diagnostic procedures, is undergoing surgery or is actually ill.
In the acute care setting, patients are usually ill and require at least 4-hourly monitoring. The frequency can often be reduced in rehabilitation, mental health and care facilities for the elderly, and in the end stages of life.
Special circumstances. These might require a prescription from the medical staff. They include:
Blood glucose meters
Blood glucose meters are devices used to monitor blood glucose in the home or at the bedside in hospital. The first capillary blood glucose meter was introduced in 1974. Over the following decades the technology of both meters and test strips has changed rapidly. Modern meters are small, light, only require small quantities of blood, and are accurate if the factors that influence the results are taken into account. Staff should become familiar with the system used in their place of employment. Consult the diabetes educator/specialist team or manufacturer for specific advice.
Where meters are used, a blood glucose meter quality management programme with a centralised coordinator is desirable. As part of such a programme it is recommended that:
- Individual nurses and other users demonstrate competence to use the system in operation.
- Meters are subject to regular control testing and calibration according to the manufacturer’s recommendations and are calibrated as required, usually when a new pack of strips is opened, and are appropriately cleaned and maintained and that these processes are documented.
- A procedure for dealing with inaccurate results and meter malfunction is in place.
Two main types of meter are available, reflectance photometers and biosensors. The former measures the colour change that occurs when chemical reagents in the test strip react with glucose in the blood. A light in the test chamber of the meter illuminates the test strip and the amount of reflected light is measured electronically and converted into a blood glucose concentration, which is displayed as a number in the test result window.
Biosensors measure an electrical current that is generated when glucose in the blood reacts with chemical reagents in the strip (known as a sensor). The current is generated in proportion to the concentration of glucose in the blood and is displayed in the result window as a number. Most meters can be programmed to read in mmol/L or mg/dL, which is used in the United States. Most meters also store a record of blood glucose tests that can be downloaded into computer software programmes that enable the data to be displayed in a range of ways.
Modern meters are small and light, easy to operate, and only require a very small amount of blood. Particular meters are designed specifically for particular target audiences such as children and older people, who have different requirements. For example, large result display screens and ‘talking’ meters for vision impaired people. Test strips require a minimal amount of blood. Therefore, many of the systems errors associated with early meters have been eliminated. However, inaccuracies still occur and are mostly due to technique errors.
Meter technology changes rapidly and health professionals need to be aware that the system in use in the hospital may be different from the system the person uses at home and note the following points.
Although blood glucose readings obtained from the fingertip most closely correlate with arterial glucose, alternative site testing (from sites other than the fingertip such as the forearm, abdomen and thigh) are available and cause less discomfort but only yield small quantity of blood ~3 μL. However, blood glucose levels vary among different sites. For example, there is a lag in increases and reductions in blood glucose by up to 30 minutes at the forearm compared with the fingertip, which can lead to delay in detecting and treating hypoglycaemia (Jungheim et al. 2002). Less variation occurs between the palm and ball of the thumb.
Continuous glucose monitoring systems
The technology to enable continuous glucose monitoring is developing rapidly towards the ultimate ‘closed loop system’. Fingerprick blood glucose tests may miss many hypo and hyperglycaemic levels: continuous blood glucose monitoring systems enable ‘real-time’ continuous blood glucose levels to be identified. Sampling generally occurs from interstitial and tissue sites. Interstitial glucose concentrations are often lower than capillary concentrations during the night compared with capillary glucose (Monsod et al. 2002. However, continuous monitoring enables the trend toward hyper or hypoglycaemia (trend analysis) to be monitored and preventative action to be taken.
Glucowatch® G2 Biographer
The Glucowatch® G2 Biographer Glucose Monitoring System is a non-invasive blood glucose monitoring method that works by iontophoresis to extract tissue liquid and monitor blood glucose approximately every 20 minutes. It shows a good correlation with capillary glucose but has a lag time similar to alternative site testing and may underestimate the actual level (Garg et al. 1999).
The device works by reverse iontophoreses and uses an electric current that stimulates sweat production. Glucose is absorbed from the sweat by an autosensor, a small disposable pad, on the back of the device. The autosensor transforms the electrical signal to a glucose reading that can be displayed by pressing a button. The autosensor must be changed every 24 hours. An alarm sounds if the blood glucose goes too low or too high. The Glucowatch® holds up to 4000 tests in the memory and is only approved for adult use at present. The manufacturer, The Animas Corporation, announced they would discontinue selling the current model in the US because new products are being developed. The sensors will be available until July 2008 (http://www.glucowatch.com, accessed February 2008).
Continuous glucose monitoring system (CGMS)
The CGMS system consists of a pager-sized glucose monitor, disposable subcutaneous glucose sensor, a cable connecting these two components to a communication system that stores data, which is downloaded into a computer software program that enables the results to be displayed in graph form. Glucose concentrations are measured every 10 seconds; 1440/day. Glucose sensors need to be changed after 72 hours. At least four capillary blood glucose measurements are required each day to calibrate the CGMS and when there is likely to be a variation such as following severe hypoglycaemia or a glucose load (Guerci 2003).
Glucose targets can be assigned, the duration and frequency of hypo and hyperglycaemic episodes, and modal time determined using modern software. This provides important information that can help health professionals and patients understand the differences between their home blood glucose testing results and HbA1c and detect unrecognised hypoglycaemia. It is primarily used to determine blood glucose profiles before using insulin pumps, during GDM, in paediatrics, and to detect unrecognised hypoglycaemia rather than for routine home monitoring because of the cost. Other CGMS systems include the Pendragon Medical Company impedance spectroscopy system (Caduff et al. 2003) and the Freestyle Navigator Continuous Glucose Monitoring System (Weinstein et al. 2007).
Interpreting different results
Patients often comment that their blood glucose results are different from the results obtained using the meter in the outpatient clinic and doctor’s rooms or at when they retest their blood glucose after a few minutes. Blood glucose meter tests only reflect individual points in time and may not detect fluctuations in blood glucose especially post prandially and overnight. CGMS is useful to detect such fluctuations.
Different meters give different results even when the tests are performed correctly and close together in time but generally should not differ by more than ~5%. Squeezing the finger to obtain a drop of blood can dilute the sample with tissue fluids and affect the accuracy of the test result.
Likewise, capillary glucose values are likely to differ from laboratory values reported on venous blood. Capillary glucose is ~5% higher than venous glucose. Laboratory values can be affected by glycolysis. Glucose in whole blood decreases by ~5–7% per hour because of the glycolytic enzyme activity in red blood cells. Thus venous samples should be sent to the laboratory promptly or kept at 4°C for short periods if it is not possible to transport the sample immediately. Preservatives such as fluoride in blood tubes slow but do not stop glycolysis in blood samples.
People are often confused by the different ways of reporting blood glucose (mmol/L or mg/dL) and HbA1c (%). Meter blood glucose results may not give an accurate indication of the average blood glucose level or of the minute fluctuations that occur minute-by- minute, see continuous blood glucose monitoring on the previous page. Discrepancies between blood glucose meter readings and HbA1c could be used as an opportunity to explore testing technique, other factors that affect the results of both testing methods and the individual’s feelings about diabetes and its management. The differences may be a sign of underlying stress, especially in adolescents (Rose et al. 2002) see Chapter 13.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree