Rationale
Nurses are often the person’s first point of contact. People with diabetes expect them to have some knowledge about the impact of diabetes on their sexual health. Sexuality is an integral component of health and sexual problems affect all aspects of health and well being. Sexual dysfunction in men with diabetes is well documented but sexual dysfunction among women with diabetes is not well understood. The sexual response is an interaction between two (usually) people. Sexual dysfunction is also likely to involve both partners in the relationship (Masters & Johnson 1970). Nurses are ideally placed to be able to emphasise the need for primary prevention and early identification of sexual difficulties and to dispel sexual mythology.
Sexual health
Sexual health is a core aspect of an individual’s general wellbeing and is the result of an integration of many components into a unified complex system – endocrine hormonal regulators, and the vascular, nervous, and psychological systems. Diabetes can profoundly affect the individual’s sexual identity and the physical ability to engage in sexual activity. Maximising sexual health should be an integral part of an holistic management plan for people with diabetes. Management should include education about, screening for where relevant, and managing general issues such as safe sex, contraception, sexually transmitted diseases, and the importance of planned pregnancies. Thus a life continuum approach may be required.
Contraception
Female contraception is described in Chapter 14. Contraception options for men include:
- Condoms.
- Withdrawal before ejaculation, which is not recommended and has a high failure rate for pregnancies and sexual satisfaction.
- Billing’s method, which requires cooperation from female partners.
- Vasectomy.
Male contraceptive agents under study include depo-Provera, which stops spermatogenesis.
Sexual issues are highly sensitive and must be approached with tact and consideration of the person’s culture, sexual beliefs, and their privacy and confidentiality. Thus, although partners can often provide important information about their partner’s sexual functioning, they should not be included unless the individual agrees.
The World Health Organisation (WHO) (1975) stressed the importance of sexuality as an integral component of health and defined sexual health as:
The capacity to control and enjoy sexual and reproductive behaviour, freedom from shame, guilt and false beliefs which inhibit sexual responsiveness and relationships. Freedom from medical disorders that interfere with sexual responsiveness and reproduction.
(WHO 1975)
By the WHO definition, the majority of the general population as well as people with diabetes do not achieve sexual health!
Masters and Johnson first described the human sexual response in 1970. They described four phases: arousal, plateau, orgasm, and resolution (Masters & Johnson 1970). These phases blend into each other and sexual difficulties can occur in one or all of them. Kaplan (1979) described a biphasic response that involved parasympathic nerve activity – vasocongestion, vaginal lubrication and erection; and sympathetic nerve activity – reflex muscle contraction, orgasm, and ejaculation. Kaplan’s description makes it easier to see how diabetes can affect physical sex given that autonomic neuropathy causes nerve damage, see Chapter 8.
Sex counsellors continue to utilise many of the sexual counselling techniques developed by Masters and Johnson. Sexual difficulties do not occur in isolation from other aspects of an individual’s life and relationships and a thorough assessment and history is necessary to identify the causal factors. Masters and Johnson found that age and chronic disease processes do not affect female sexual responsiveness as severely as they affect male sexuality. In addition, the sexual response is more varied in women than in men. While these are old references, they are still relevant and widely cited in the relevant literature.
Sexual development
Sexual development occurs across the lifespan:
- Chromosomal sex is determined at fertilisation.
- 3–5 years – diffuse sexual pleasure, fantasies and sex play. Often form a close relationship with a parent of the opposite sex.
- 5–8 years – interest in sexual differences, sex play is common.
- 8–9 years – begin to evaluate attractiveness and are curious about sex.
- 10–12 years – preoccupation with changing body and puberty. Adolescents are often sexually active by this age, thus sex education should start early and information provided in accordance to the child’s capacity to understand and using appropriate language.
- 13–20 years – puberty, development of self-image and sexual identity.
- Late 30–early 40 – peak sexual responsiveness.
- Menopause – variable onset and highly individual effect on sexuality.
- Old age – physical difficulties and limited opportunity.
Effective sex and diabetes education should be part of the diabetes management plan so that problems can be identified early and optimal sexual functioning maintained. Health professionals and people with diabetes often have limited information about the impact diabetes can have on their sexuality. Sex education, good metabolic control, early identification, and management of sexual problems are important, but often neglected, aspects of the diabetes care plan. When a sexual problem is identified the focus is often on dysfunction and performance rather than on what is normal, which can have a negative psychological impact on sexuality. Changing the focus to what can be achieved and focusing on feelings, intimacy, love, and warmth have a big impact on general and sexual well being.
Sexual problems
Sexual satisfaction is a combination of physical and emotional factors. Sexual problems can be:
- Primary – usually defined as never having an orgasm.
- Secondary – difficulties occur after a period of normal functioning. Most sexual difficulties fit into this category.
- Situational – where the situation itself inhibits sexual activity, other sexual problems may also be involved.
Possible causes of sexual difficulties and dysfunction
Sexual difficulties usually involve two people. It may be a shared problem or each person may have individual issues that need to be considered. Interpersonal factors, the relationship and environmental and disease factors need to be explored with the couple involved.
- Ignorance and misinformation, which are common, despite the sexually permissive society of today. A great deal of readily available literature in magazines and on television with an overemphasis on performance sets up unreal expectations.
- Guilt, shame, and fear, which may be fear of getting pregnant, contracting a sexually transmitted disease, not pleasing their partner or being rejected by them.
- Gender insecurity/uncertainty and sexual preference.
- Non-sexual concerns, for example, about finances, children, job.
- Past sexual abuse.
- Physical condition, for example, presence of diabetes especially diabetes complications such as autonomic neuropathy and vascular disease.
- Sexual relationships are one of the most complex undertakings people ever make; yet most people prepare for it casually.
- Communication problems – the most common sexual difficulty.
- Lack of trust.
- Different sexual preferences and desires, for example, frequency of intercourse.
- Relationship difficulties that can include difficulties associated with alcohol and violence or be related to disease process, including diabetes.
- Changes in lifestyle, for example, having children, retrenchment, retirement, and illness.
- Depression, anger, guilt, anxiety, fear, feelings of helplessness, changed body image and self-identification as a victim, lowered self-image and self-esteem may or may not accompany the disease. Loss of libido is one of the classic signs of depression.
- Pain, debilitation associated with changed mobility, for example, arthritis, bad odour associated with infections, cardiac and respiratory problems and sleep apnoea, and snoring. Some people worry about resuming sexual activity after an MI. Education can help allay such fears.
- Disease processes and hormonal imbalance, including diabetes, as well as other endocrine and reproductive conditions.
- Medications, for example, antihypertensive and antidepressive agents.
- Hypoglycaemia during intercourse can be frightening and off-putting, especially for the partner, and inhibit spontaneity and enjoyment in future encounters.
- Tiredness and decreased arousal and libido are associated with hyperglycaemia.
- Mood disorders such as depression and other psychological problems may be present but mood can change with hypo- and hyperglycaemia and can cause temporary sexual problems.
- Lack of privacy.
- Limited opportunity, for example, older people in aged care facilities.
- Uncomfortable, noisy surroundings.
Sexuality and older people
Older people are capable of having fulfilling sexual relationships but often lack the opportunity or are constrained by environmental factors, ageist attitudes, sexual stereotypes and disease processes (see Chapter 12 ). Sensory impairment can change the individual’s response to sexual stimulation and the multiplicity of medications required by many older people can inhibit sexual functioning.
Touch is important throughout life and caring touch as distinct from providing nursing care is often lacking. Touch can provide a great deal of sexual pleasure when intercourse is not possible. Many older people are deprived of touch in aged care facilities or when a partner dies.
Women
The biological effect of diabetes on male sexual functioning has been well documented. The effects of diabetes on sexual function in women are poorly understood and the evidence for any effect is less conclusive than the evidence for the effects on male sexual functioning (Leedom et al. 1991). Physicians regularly ask men about their sexual functioning but not women (House & Pendleton 1986; Bernhard 1991). Although these are old studies there is no indication that things have changed. There is no real evidence that physical function in women is impaired by diabetes in the same way as it is in men, except decreased vaginal lubrication in older women with Type 2 diabetes. This could be due to normal ageing, related to diabetic neuropathy or other causes such as inadequate arousal. More women achieve orgasm from foreplay than from intercourse (Clarke & Clarke 1985) and this may also be a factor.
Women who have difficulty accepting that they have diabetes report higher levels of sexual dysfunction than those who accept their diabetes. Type 2 diabetes has a pervasively negative effect on women’s sexuality (Schriener-Engel et al. 1991). There appears to be little or no effect in women with Type 1 diabetes but they often have concerns about pregnancy, childbirth, and hypoglycaemia during sex (Dunning 1994). There is a positive correlation between the degree of sexual dysfunction and the severity of depression that illustrates the connection between physical and psychological factors and the need for an holistic approach.
Changing blood glucose levels can have a negative transient effect on desire and sexual responsiveness and women often report slow arousal, decreased libido and inadequate lubrication during hyperglycaemia. Desire can fluctuate with stages of the menstrual cycle but this also occurs in women without diabetes. However, there is no correlation between the presence of complications and sexual difficulties in women with diabetes (Campbell et al. 1989; Dunning 1993). Polycystic Ovarian Disease and its effects could have adverse psychological effects (see Chapter 14 ).
The developmental stage of the individual should also be considered when assessing sexual health and the impact of diabetes when planning sex education and counselling.
- Children and adolescents – diabetes can affect normal growth and development if it is not well controlled and menarche and puberty can be delayed. This could impact negatively on body image and the development of sexual identity and self-esteem. Eating disorders and insulin manipulation can compound the problem.
- Young adulthood – attracting a partner, successful pregnancy and birth can be areas of fear and concern that affect sexual health (Dunning 1994). Hyperglycaemia can occur during menstruation resulting in tiredness, decreased arousal and libido. Vaginal thrush is common and causes itch and discomfort during sexual intercourse. It may be associated with taking oral contraceptives or antibiotics for intercurrent illness. Thrush and balanitis can inhibit male sexual activity.
- Older age group – hormonal changes due to menopause and associated fatigue and depression inhibit sexual enjoyment. Often a long-term partner’s life course is different and this affects their sexual relationship. There are fewer partners and opportunities for sexual activity for older women especially those in care facilities.
Specific problems should be investigated depending on their presentation. Preventative sexual health care such as breast self-examination, mammograms, and cervical (pap) smears should be part of the care plan.
Men
Diabetes does have physical effects that cause erectile dysfunction (ED). Other ED causes include:
- Vascular damage, both systemic atherosclerosis and microvascular disease.
- Neurological diseases such as spinal cord damage, multiple sclerosis, and diabetic neuropathy.
- Psychological causes such as performance anxiety, depression and mood changes may be associated with hypo-or hyperglycaemia.
- Endocrine diseases that result in lowered sex hormones: testosterone, SHBG, prolactin, FSH, and LH. Hypogonadism can occur in chronic disease.
- Surgery and trauma to genitalia or its nerve and vascular supply.
- Anatomical abnormalities, for example, Peyronie’s contracture, which is often associated with Dupuypten’s contracture and other glycosylation diseases including diabetes, see Chapter 10.
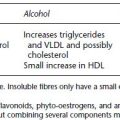
- Medicines such as thiazide diuretics, beta blockers, lipid lowering agents, antidepressants, NSSRI, smoking, alcohol, and illicit drug use.
- Normal ageing.
ED is defined as the inability to achieve or maintain an erection sufficient for satisfactory sexual performance – penetration and ejaculation. It is common in men with diabetes especially if other diabetic complications are present. It occurs in 50% of men 10 years after the diagnosis of diabetes especially those who smoke. ED is gradual, insidious and progressive (Krane 1991). ED may be a predictor of cardiovascular risk and there is a higher incidence of undiagnosed coronary disease in men with ED. Elevated blood fats and hypertension and antihypertensive agents also play a part in the development of ED. Lowered sperm counts are associated with obesity, smoking and poor diet.
ED significantly reduces the man’s quality of life especially in the emotional domain and has a negative effect on self-esteem. However, ED also has a significant effect on the man’s partner. Partners play a key supportive role in the man’s treatment and treatment success (Dean et al. 2008). When sexual functioning improves, improvement in mental and social status follows. Other sexual issues for men are fatigue, fear of performance failure, and concern about not satisfying their partners, but most men do not involve their partners when they seek advice about ED (Dean et al. 2008).
Investigation and management
A thorough history and physical examination are required. Some of the questions that need to be asked are very personal, which may be difficult and stressful, thus time, privacy, and tact are essential. The assessment includes diabetic complication status and blood glucose and lipid control, identifying the cause and determining the extent of the dysfunction, for example, using rigiscan and snap gauge to determine whether nocturnal erections occur, and sleep apnoea studies. There is an association between poor sleep, sleep apnoea and ED. Doppler studies are carried out to determine local blood flow. Testosterone, FSH, LH, SHBG, and prolactin levels are measured. Management consists of:
- Good metabolic control to prevent ED.
- Early intervention if ED occurs.
- Assessing fitness for sex and modifying risk factors, for example, losing weight, managing pain, smoking cessation, and reducing alcohol intake.
- Appropriate diet and exercise programme. Tai Chi and strength training can improve flexibility and strength and general well being in older men.
- Sex education that includes setting realistic expectations and planning for regular sexual health checks, for example, prostate disease.
- Diabetes education.
- Counselling, which should include partners and inform them about treatment options to help the couple find fulfilling sexual alternatives if the man cannot achieve erections.
Medication management
Oral medicines
Medication management includes oral phosphodiesterase type 5 (PDE-5) inhibitors Sildenafil (Viagra), Vardenafil (Levitra), and Cialis, which are vasodilators that enhance the natural sexual response. They can cause visual disturbances (‘blue vision’), transient hypotension and can unmask cardiac ischaemia. PDE-5 medicines are contraindicated if nitrate medications are used and when cardiovascular disease is present. Cimetidine and Ketoconozale can increase Viagra levels and Rifampicin decreases them.
Other oral medicines currently under study include sublingual apomorphine (UPRIMA), which acts centrally and enhances the response to stimulation and oral phentolamine (VASOMAX), which improves penile blood flow (Endocare 2004).
Urethural and injected medicines
Urethurally introduced medicines such as MUSE have a success rate between 30% and 50% of men. Side effects include urethral pain and burning in 7–10% of men who use this medicine.
Intracavernosal therapy or penile injections such the vasoconstrictor agents papaverine, alprostadil (Caverject), VIP, and the vasodilator phentalamine. Men and/or their partners need to learn the technique of penile injections, which should be done under supervision. A rare but serious side effect is priapism, which requires urgent treatment to reverse the effects of the vasoconstricton. Other side effects include the formation of scar tissue, bruising, and rarely infection at injection sites. Caverject sometimes causes pain in high doses.
Non-pharmacological therapy
Non-pharmacological therapy includes external vacuum pumps. Vacuum devices are a simple effective method of achieving an erection. A man suffering from ED invented a device called ErecAid® in the 1960s. It consists of a clear plastic cylinder, which has either a manual pump or batteries and a special tension ring. The penis is placed into the cylinder and the man or his partner holds the device firmly against the body to form an airtight seal and then pumps the air out of the cylinder, which creates a vacuum and causes the penis to become erect. The special tension ring is inserted over the device around the base of the penis to maintain the erection, and the device is removed. The whole process takes about two minutes and the erection is maintained for about 30 minutes (longer than natural erections). The ring must be removed after intercourse.
Vacuum pumps have very few side effects. Sometimes, small red dots called petechiae and bruising can occur on the penis but these are not harmful. They are more likely to occur if the individual is on anticoagulant medicines. The temperature in the penis drops 1–2 degrees, which is caused by the tension ring. The device can be difficult to use, so learning how to use it, is important. It can reduce sexual spontaneity so it is very important that the man discusses sexual issues and their management options with his partner.
Hormone replacement therapy
Hormone replacement therapy (testosterone) might be indicated in 3–4% of men, but is contraindicated in men with liver disease, cardiovascular disease, renal disease, and prostate cancer. These contraindications probably apply to many men with diabetes. Testosterone comes in various dose forms including oral, injections, and implants.
Complementary medicines for sexual problems (CAM)
Men with sexual health problems commonly use CAM especially if they receive conflicting advice and worry a lot about the problem (Trutnovsky et al. 2001). CAM can be used to improve general health and well being and mange stress that can have benefits for sexual health, see Chapter 19. Likewise, recommendations about the importance of eating a healthy diet and exercise and adequate rest and sleep to sexual health are important. Often supplements such as flaxseed oil, vitamins E, and C and zinc are recommended. However, rigorous evidence for most is lacking and some are harmful. CAM therapies appear to target three main sexual issues: improving sexual ‘stamina’, aphrodisiacs, overcoming erection problems.
Commonly used CAM medicines include the following. They are often used in combination:
- Horney goat weed
- Passion treatment
- Damiana
- Yohimbe
- Asian Ginseng
- Goji berries, which are sometimes referred to as ‘natural viagra’ and also come chocolate coated.
Many so-called aphrodisiacs carry significant health risks (often for animals) and are not recommended. These include powdered rhino horn, crushed pearls, Spanish fly, and animal testicles.
The risks and benefits of these medicines are not known and they may interact with conventional medicines including those used to manage sexual problems. Therefore, it is important to ask men and women with sexual health problems about CAM use. The US FDA warned people about two unapproved dietary supplements sold online to treat ED: ‘Blue Steel’ and ‘Hero’, which contain active ingredients with similar actions sildenafil. These products could interact with conventional nitrate medicines and cause hypotension. People might unwittingly seek such alternatives if conventional ED medicines are contraindicated.
Involving partners in ED management
Partner may be able to contribute important information about the man’s general health and sexual history but should only be involved if they are willing and the man agrees. The man, and ideally his partner, need to be involved in selecting the best management option. Partner’s attitudes affect the man’s uptake of and adherence to ED treatment and long-term management is more successful if the partner is involved (Fisher et al.2005). The Index of Sexual Life (ISL) (Chevret et al. 2004) is a validated tool developed to assess women’s sexual desire and satisfaction when their partner has ED.
Chevret et al. (2008) and Fisher et al. (2005) found partners of men with ED had significantly reduced sexual drive, orgasm, satisfaction, and frequency of sex compared with partners of men who did not have ED and prior to the onset of ED. In addition, partners of men with ED are more likely to have sexual dysfunction or avoid sexual activity.
A number of studies demonstrate significant improvements in sexual function, satisfaction, and quality of life for both partners following treatment, especially with PDE-5 medicines (Fisher et al. 2004) but discontinuation rates with these medicines appear to range between 10 and 45% (Madduri 2001).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree