Fig. 4.1
TES (transanal endoscopic surgery) platforms . Rigid platforms include (a) TEM (transanal endoscopic microsurgery) (Richard Wolf Medical, Vernon Hills, IL, USA). (b) TEO (transanal endoscopic operation) (Karl Storz Endoscopy-America, Inc. El Segundo, CA, USA). TAMIS (transanal minimally invasive) platforms include (c) SILS (single incision laparoscopic surgery, Covidien, Mansfield, MA, USA). (d) GelPOINT path (Applied Medical, Rancho Santa Margarita, CA, USA)
Until recently, adoption of transanal endoscopic surgery was confined to a few high volume and centers of expertise. Wider adoption was limited by the prohibitively high costs of the rigid TEM and TEO platforms, scarcity of training centers , and long learning curve required to achieve technical expertise in these procedures. In 2009, at the height of popularity of single-incision laparoscopy, an alternate transanal endoscopic setup using single-incision laparoscopic disposable transanal ports was reported, which was called transanal minimally invasive surgery (TAMIS) [20, 21].
TAMIS has popularized transanal endoscopic approaches through improved access, as disposable equipment is more readily available, less expensive, and compatible with standard laparoscopic equipment [21]. TAMIS platforms are shorter and pliable, thereby increasing the freedom of motion and limiting instrument collision (SILS Port, Covidien, Mansfield, MA, Fig. 4.1c; GelPOINT Path, Applied Medical, Rancho Santa Margarita, CA, Fig. 4.1d). The shorter length, however, limits the extent of proximal rectal wall retraction and exposure, particularly beyond the second or third haustral valves [22]. Rather than using an anchoring arm to stabilize the platform and the stereoscope, a standard laparoscopic camera and scope are used. TAMIS procedures therefore require two operators, a camera holder and an operating surgeon. While a number of case series have been published demonstrating the preliminary feasibility and safety of TAMIS, these studies are relatively small and the data short-term, with no long-term oncologic results of TAMIS yet described.
TES as Compared to TAE and TME
TEM has long been considered an ideal minimally invasive approach to resect large rectal adenomas not amenable to complete endoscopic resection with a colonoscope, incompletely resected adenomas with dysplasia or intramucosal adenocarcinoma, small low-risk carcinoids, and other miscellaneous benign rectal pathologies. Until recently, however, the use of TEM for cancer was most widely accepted for the resection of rectal cancers in patients refusing more oncologically appropriate radical resection, radiation, or abdominoperineal resection and for palliative resection in patients considered medically unfit to undergo radical resection (Fig. 4.2). Routine use of TEM in the curative resection of T1 and T2 rectal cancers has been controversial because of unacceptably high rates of local recurrence reported in early series on local excision using TAE and TEM relative to radical resection rates. More contemporary published series, however, have demonstrated that local excision via TEM/TEO may be used with a curative intent in carefully selected cases of T1 rectal cancer with acceptable oncologic outcomes.
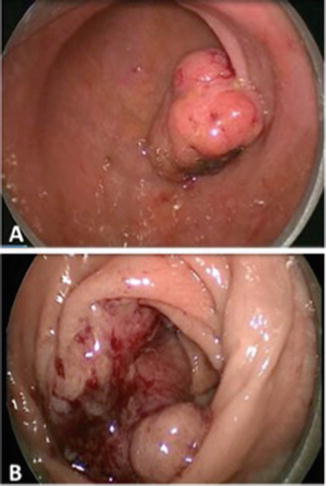
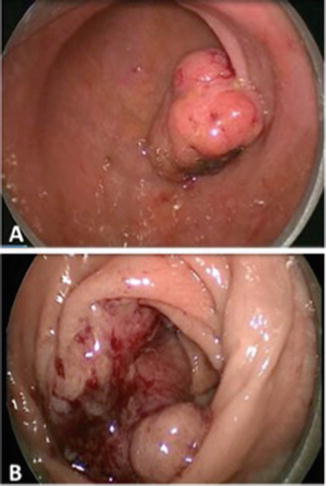
Fig. 4.2
TES resection of malignant rectal lesions : (a) Full-thickness curative resection of a 3 cm upper rectal polyp with a small focus of well-differentiated invasive adenocarcinoma (pT1, sm1, LVI). (b) Full-thickness for a mid-rectal bleeding T2 rectal cancer in a patient with dementia and major medical comorbidities, not eligible for radical resection of CRT
Several studies have demonstrated equivalent or superior outcomes of TEM for rectal cancer as compared with other methods of local excision [13, 23]. A recent meta-analysis by Clancy et al. reviewed six studies that compared outcomes from TAE and TEM. Cohorts were highly heterogeneous and included a mix of adenomas and adenocarcinomas as well as tumors of various stages. There were no differences in overall complication rates, but TEM was associated with higher negative margin rates (OR 5.28), reduced specimen fragmentation (OR 0.10), and lower rates of local recurrence (OR 0.25) when compared with conventional transanal excision [15]. However, studies included in this meta-analysis were retrospective, with varying definitions of specimen fragmentation and local recurrence. Although randomized studies comparing local excision techniques are lacking, superior oncologic outcomes with TEM are presumably secondary to the better visualization and more precise dissection that can be accomplished with this approach as compared to TAE. Despite this evidence, TAE is still more commonly used than TEM or TAMIS in many centers because of lack of specific training in TES, low volume of cases, and higher costs related to these procedures [13].
Although originally developed to treat benign disease, indications for TEM have expanded over the last 30 years to include the curative treatment of rectal adenocarcinoma via full-thickness endoscopic excision in select cases. Selection of appropriate tumors for local excision rather than radical resection remains a topic of controversy [24–27]. Unacceptably high local recurrence rates in heterogeneous cohorts treated with TEM alone are still quoted, despite their inherent biases. These earlier retrospective case series reported mixed data from TAE and TEM cohorts and did not use current staging modalities including pelvic MRI. Further, T1 tumors were not sub-analyzed based on histopathologic features that are now known to be of prognostic significance for lymph node metastasis and local recurrence. More contemporary TEM series have demonstrated comparable oncologic outcomes in select cohorts with low-risk T1 tumors relative to radical resection with TME [28]. Authors have adopted standard preoperative staging and detailed pathologic review in order to identify patients with very low risk of occult nodal disease who would in effect likely be overtreated by radical surgery, thus incurring unnecessary morbidity. These carefully selected T1 rectal tumors can usually be safely offered TEM alone as curative therapy. Moreover, there is mounting evidence to support the potential use of TEM in combination with adjuvant or neoadjuvant chemotherapy for more advanced lesions, when carefully selected [29, 30].
Indications for TES
Benign Disease
TEM was originally developed as an alternative minimally invasive endoscopic approach for rectal adenomas and is currently the preferred approach to resect large or carpeting adenomas that cannot be removed via conventional colonoscopy, particularly in centers that do not use endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) techniques [13, 24, 25]. In such cases, when an underlying malignancy is not suspected, TEM with submucosal dissection can be used in a manner similar to endoscopic submucosal dissection, in order to avoid large full-thickness rectal defects [31, 32]. TEM is also commonly used in the setting of incomplete resection by piecemeal polypectomy or EMR, when a focus of high-grade dysplasia or intramucosal adenocarcinoma with unascertainable or positive deep margins of resection is discovered upon pathology review. In such cases, full-thickness excision of the polypectomy scar by TEM, TEO, or TAMIS is not only diagnostic of any residual tumor or more advanced disease but also therapeutic, as it achieves definitive resection of the lesion [33]. TEM has also been used for a variety of other tumors including early-stage rectal carcinoid, GIST tumors, and presacral tumors, as well as other benign conditions including repair of complex rectourethral and rectovaginal fistulas, stricturoplasty, and repair of colorectal anastomotic complications [34].
T1 Rectal Cancer
Selection of appropriate patients for treatment of rectal cancer with TES alone remains a topic of controversy. Of particular concern are the overall high rates of local recurrence following TEM for unselected T1 tumors, with some early studies reporting rates of local recurrence as high as 26% [35]. Such unacceptably high rates of local recurrence have driven efforts to identify risk factors for lymph node involvement and local recurrence of T1 rectal tumors and better identify T1 tumors that may be suitable for excision by TEM.
Several studies have sought to determine histopathological risk factors for local recurrence. One of the most important risk factors identified has been the degree of submucosal invasion. As described by Kikuchi et al., T1 lesions can be further classified by the level of penetration of tumor into the submucosa , with sm1 representing invasion into the upper third, sm2 into the middle third, and sm3 into the deepest third [36]. The depth of submucosal invasion according to this classification is predictive of local recurrence following TEM, with depth greater than sm1 being highly predictive of local recurrence [37]. In one cohort of 48 patients who underwent TEM for T1 cancer, 10.4% experienced local recurrence at a median follow-up of 54 months. Of these, none of 26 patients with sm1 lesions developed recurrence, while 5 of 22 patients with sm2–sm3 lesions recurred. This suggests that T1 sm2–sm3 lesions may behave more like T2 tumors and are not suitable for treatment with TEM alone. This finding is not surprising given that the degree of submucosal invasion is highly associated with the likelihood of positive lymph nodes, with sm1 lesions having a 0–3% chance of lymph node positivity, whereas T1 sm2–sm3 and T2 lesions have 15–25% lymph node positivity [38].
Additional important histopathologic risk factors for local recurrence following local excision include poor differentiation grade, lymphovascular invasion (LVI) , positive resection margins (R1 resection), large tumor size, and the presence of tumor budding [39]. Doornebosch et al. have reported on the importance of tumor size in predicting local recurrence [40]. Out of 62 patients with T1 tumors, the overall 3-year local recurrence following TEM was 31%, with significantly higher local recurrence for tumors larger than 3 cm relative to tumors smaller than 3 cm (39% versus 11%). Local recurrence was lowest in the subgroup of tumors less than 3 cm with no evidence of sm3 submucosal invasion (7%).
Tumor budding refers to the presence of small discrete clusters of tumor cells (less than five cells) at the invasive tumor edge [41]. Tumor budding has been consistently demonstrated in multivariate analyses to be an independent adverse prognostic factor associated with local recurrence and metastases, as well as significantly worse overall and disease-free survival in colorectal cancer [42]. For submucosally invasive colorectal carcinomas that are candidates for endoscopic resection by EMR or ESD, several large studies have shown tumor budding to be an independent prognostic factor associated with lymph node metastases, local recurrence, and cancer-related death [43]. In a series of 251 submucosally invasive colorectal carcinomas that were ultimately resected using radical resection, high tumor grade, LVI, and tumor budding were the three factors independently associated with lymph node metastases [44]. Compared to patients without any of those risk factors, patients with 1, or 2–3 of those risk factors, had a significantly higher rate of nodal metastases (1% versus 21% versus 36%). This suggests that local excision with polypectomy or TEM with negative resection margins would be sufficient treatment for early T1 colorectal carcinoma with no such risk factors [44, 45]. In the series of 62 T1 rectal cancers resected using TEM by Doornebosch et al., the 3-year local recurrence for tumors less than 3 cm without budding was 10% compared with 38% in tumors greater than 3 cm and with budding [40].
With respect to current consensus and guidelines for the management of early rectal cancer, the 2015 NCCN guidelines currently recommend TEM as an alternative approach for the management of select T1 cancer [46]. According to these guidelines, adenocarcinoma that is to be treated with TEM should have no radiographic evidence of lymph node involvement based on preoperative endorectal ultrasound (ERUS) and/or pelvic MRI, be less than 3 cm in diameter and less than 30% of the rectal circumference, be well to moderately differentiated, and be within 8 cm of the anal verge. These guidelines are based on several recent series that have reported local recurrence rates following TEM of T1 rectal cancers selected using the above selection criteria comparable to those following radical resection. Despite this evidence, there remains considerable controversy with regard to whether TES is a valid alternative to TME for T1 cancer. For example, in a review of 11 national or international guidelines on management of rectal cancer, only eight recommended the use of TES in the treatment of low-risk early rectal cancer [47].
This debate is particularly relevant given the increasing adoption of EMR and ESD for en bloc resection of superficial colorectal cancer (intramucosal adenocarcinoma or T1 sm1 cancers), which has been associated with good short- and long-term oncologic outcomes [25, 48, 49]. In a recent European Association for Endoscopic Surgery (EAES) consensus statement on early rectal cancer, full-thickness excision down to the mesorectum was considered the procedure of choice in order to achieve R0 en bloc resection for T1 tumors determined preoperatively to be well to moderately differentiated, without lymphovascular and perineural invasion, less than 4 cm in diameters and involving <30% of the rectal wall circumference [50]. With regard to ESD, the EAES consensus quoted two recent studies , including one which retrospectively compared 30 ESD and 33 TEM patients for resection of non-polypoid rectal mucosal adenocarcinomas or submucosally invasive adenocarcinomas. No significant differences were noted in en bloc resection rates or R0 resection rates (96.7% versus 97%), procedural or postoperative complications , or need for additional treatment such as radical resection or adjuvant treatment. ESD was associated with shorter operative time and length of hospital stay, and no local recurrence or distant metastases were noted over the study period [48].
T2 Rectal Cancer and Locally Invasive Tumors
While TEM , TEO, and TAMIS are considered acceptable alternatives for curative resection of carefully selected T1 rectal tumors, TES as a unimodal treatment for T2 or T3 cancer—outside of the palliative setting—is considered oncologically inadequate, due to the higher rates of lymph node metastasis, ranging 12–28% and 36–66% in T2 and T3 disease, respectively [16]. In an early study, Lee et al. retrospectively evaluated 17 patients treated with TEM and 83 patients treated with radical resection for T2 lesions [51]. No patients received adjuvant therapy. Local recurrence was 19.5% in the TEM group as compared to 9.4% in the radical surgery group (p = 0.035), although disease-free survival was similar in the two groups. Borschitz et al. reviewed their experience with 40 T2 patients treated with TEM [52]. Of these, 20 patients underwent TEM alone with no further surgery or adjuvant therapy. Over a median follow-up of 59 months, 35% developed local recurrence and 30% systemic metastases. Among patients with high-risk histopathological features such as poorly differentiated tumors or evidence of LVI, the local recurrence rate was as high as 50%. Local recurrence in the case of T3 disease treated with TEM alone is as high as 100% in some case series [53].
The use of neoadjuvant chemoradiation therapy (CRT) prior to full-thickness TEM excision of high-risk T1, T2, and even more advanced rectal cancers, specifically in patients demonstrating clinical downstaging during chemoradiation, has shown particular promise as an alternative treatment strategy to radical rectal cancer resection with TME. Lezoche et al. recently published long-term results from a randomized control trial of patients with preoperatively staged T2 N0 tumors on the basis of ERUS and/or pelvic MRI [30]. A total of 100 patients who underwent neoadjuvant treatment were then randomized to undergo either TEM or laparoscopic TME . At a median follow-up of 9.6 years, the local recurrence rate in the TEM group was comparable to that of the radical surgery group (6% versus 8%, respectively). Moreover, complications and morbidity were lower in the TEM group. Other groups, however, have cautioned early adopters of this strategy about the high incidence of wound-related complications noted in radiated patients undergoing TEM excision of residual tumors or scars. Complications include rectal wound dehiscence which has been associated with severe and refractory pain [54].
Most recently, advocates of organ-preserving strategies have gone one step further and investigated the outcomes of non-operative management of rectal cancers that have demonstrated complete clinical regression following neoadjuvant therapy. This so-called watch-and-wait approach has been evaluated by Dr. Habr-Gama’s group in 70 patients with T2 to T4, N0 to N2 rectal cancers without evidence of metastases. Intensive chemoradiation achieved a 68% rate of complete clinical response 10–12 weeks following completion of treatment, as demonstrated by the lack of gross evidence of residual tumor or other mucosal irregularity on endoscopy or imaging following CRT [55]. These patients were subsequently observed and a sustained complete clinical response was observed in 51% of the entire cohort at 3-year posttreatment. The remaining 49% with evidence of recurrent disease underwent immediate or salvage surgery with either TEM or radical surgery. Several European series have corroborated the findings from the Habr-Gama group [29, 56, 57]. With more aggressive CRT regimens, the rates of complete clinical response have surpassed the historical 20% rate, although this has occurred at the expense of increase toxicity and possibly overtreatment early rectal tumors.
While the possibility of multimodal treatment with chemoradiation and local excision for T2 lesions shows promise, current NCCN guidelines recommend that this treatment regimen be used only in the experimental setting [46]. While not currently indicated for curative intent, TEM with or without chemoradiation is still frequently used as compromised or palliative treatment for more advanced lesions in patients who are considered medically unfit to undergo radical resection using either an open or laparoscopic approach. Palliative treatment with TEM is also pursued in those who refuse surgery that could result in permanent colostomy .
Tumor Location and Tumor Size
Prior recommendations considered tumor distance greater than 8–10 cm from the anal verge to be a contraindication to TEM, particularly for anterior tumors of the upper rectum, due to the increased risk of peritoneal entry during full-thickness resection [58]. Inadvertent peritoneal entry during full-thickness TEM excision was previously considered to be a complication requiring immediate conversion to laparotomy with low anterior resection or fecal diversion in order to mitigate the risk of leak and infection [59, 60]. From an oncologic standpoint, peritoneal entry during TEM excision of a rectal tumor was also thought to increase the risk of tumor cell spillage and thus the risk of peritoneal tumor implants [61]. Several contemporary studies from experienced TEM operators have demonstrated that peritoneal entry occurred more commonly during full-thickness resection of lesions located in the upper rectum , anteriorly or laterally along the rectal wall [62–64]. These studies showed that in experienced hands, peritoneal defects could be sutured closed transanally without increase in morbidity. Finally, several studies have demonstrated no adverse short or long-term oncologic outcomes in patients in whom peritoneal entry occurred during TEM excision of rectal tumors [61, 65]. Based on these studies, tumor location 10 cm or more from the anal verge is no longer considered a contraindication to TEM surgery, as long as full-thickness suture closure of rectal defects can be achieved transanally by experienced operators [62, 63, 65–67]. It is important to note that with respect to more complex rectal lesions, the TAMIS published experience with upper rectal lesions is limited, with only three small series reporting on seven cases of peritoneal entry during TAMIS for upper rectal tumors, with conversion to laparoscopy or laparotomy required in six out of seven cases. This has raised the concern that shorter TAMIS platforms may not be adequate to perform full-thickness resection for high-risk rectal tumors [20, 22, 68]. Overall, only lesions within reach of the 15–20 cm rigid proctoscope , and otherwise amenable to resection with TEM, should be considered or full-thickness endoscopic excision.
At the other extreme end of the rectum, TAMIS platforms do not permit access to rectal polyps located within 4 cm of the anal verge [69]. For lesions partially or entirely located within the distal 4 cm of the anorectal canal, the TEM and TEO platforms can often be pulled back maximally to permit exposure without losing excessive pneumorectum. This is in contrast to TAMIS where resection must be combined with a standard TAE approach for the distal-most dissection.
With respect to rectal tumor size, near-obstructing, near-circumferential, and circumferential tumors constitute a contraindication for transanal endoscopic resection with TES. This is in large part because of the difficulty encountered in removing bulky lesions intact with clear margins, suturing large defects with the TEM instrumentation, as well as high risk of rectal stenosis or incomplete closure with this method [26].
Technical Considerations for TES
Preoperative Workup and Staging
Comprehensive preoperative workup is essential in selecting patients who are appropriate candidates for TES as a curative surgical approach. Preoperative assessment consists of complete clinical evaluation including digital rectal examination to assess anal sphincter tone, tumor location with respect to the anal sphincters, and anorectal ring, as well as tumor fixation. Preoperative workup also includes a colonoscopy to evaluate for synchronous lesions and careful pathology review of the biopsied rectal lesion to confirm eligibility for TES. Rigid or flexible proctoscopy is also performed preoperatively by the operating surgeon to accurately determine the distance from the anal verge, tumor size and extent of rectal wall involvement, and orientation along the rectal wall [26, 66]. This assessment is essential in order to assess feasibility of the resection and select the positioning on the operating table .
Standard rectal cancer staging is performed and includes carinoembryonic antigen (CEA) serum levels , CT scans of the chest, abdomen, and pelvis to rule out distant spread, and a pelvic MRI and/or endorectal ultrasound (ERUS) . While the T-stage accuracy of ERUS is largely operator dependent, ERUS is limited in its accuracy in assessing nodal status, with accuracy rates ranging 65–81% [70]. The reported T-stage accuracy of ERUS ranges from 63 to 95% across studies [66]. The accuracy reported in multi-institutional studies is usually lower than that reported in single-institution or single-operator studies, which may relate to variations in equipment as well as the steep learning curve and operator-dependent expertise required to achieve consistency in performance and interpretation of ERUS. Overall, ERUS is relatively less accurate at differentiating between T1 and T2 lesions, with one multi-institutional study reporting only 57% accuracy, as compared with individual studies reporting up to 88% accuracy in identifying T1 lesions with this modality [71, 72]. Despite the accuracy obtained by highly skilled practitioners, a recent study showed that the results of ERUS rarely changed the management plan for patients undergoing TES when used in conjunction with other preoperative staging modalities [73].
Pelvic MRI has supplanted ERUS as the preferred modality for rectal cancer staging. Although standard MRI imaging has comparably low sensitivity (66% versus 67%) and specificity (76% versus 78%) for lymph node assessment, it provides assessment of the circumferential radial margin (CRM) , as well as detailed measurements of the tumor relative to sphincters, prostate, vagina, and even the peritoneal reflection [74]. Recent studies have highlighted 3 Tesla MRI imaging as a promising technology to improve nodal staging in rectal cancer. This technology may provide morphologic details beyond nodal size, which is not a reliable predictor of lymph node involvement. When nodal size is combined with other characteristics such as spiculation, indistinct borders, and heterogeneity of internal structure, great accuracy in predicting lymph node involvement may be achieved. In one study that investigated 437 lymph nodes in 42 patients, the sensitivity and specificity for identifying positive nodes were 85% and 97%, respectively, when using 3 Tesla MRI [75]. There is hope that accuracy of preoperative staging will continue to improve with new developments in radiographic technology [66].
Instrumentation
The original transanal microsurgery platform was developed by Gerhard Buess with support from the Richard Wolf Company (Tubingen, Germany). It consists of a rigid beveled proctoscope, 4 cm in diameter, with two lengths (12 and 20 cm) to allow for ease of operation in different parts of the rectum (Fig. 4.1a). The rectal lesion is visualized through a binocular stereoscope that allows for 3D visualization of the rectal lesion with up to sixfold magnification. The proctoscope also accommodates three 5 mm channels for specialized instruments that are angled at their tip. The 20 cm TEM proctoscope is the longest transanal platform commercially available, providing access to the upper rectum and even the rectosigmoid colon. The narrow diameter and rigidity of the metal proctoscope complicates instrument maneuvering through the platform and limits hand movement of the surgeon and instrument separation, resulting in collisions and crossing of instruments. The operating surgeon must rely on rotational movements as opposed to the typical retraction and levering of laparoscopic surgery. For this reason, the specialized laparoscopic tools used in TEM are angled at their tip to facilitate transanal dissection [24].
The system is secured to the operating table with a multi-jointed clamp, creating a stable operating platform. The scope is inserted through a dedicated port built onto the platform, which provides a stable view during dissection. The Wolf TEM setup includes its own combined pump and insufflation system to maintain consistent distention of the rectum, even during smoke evacuation and fluid suctioning [76]. The proctoscope has a detachable faceplate that provides an airtight seal and allows insufflation of the rectum. Pneumorectum is typically accomplished with pressures of 8–16 mmHg, although pressures as high as 20 mmHg are described to maintain adequate visualization in the face of rectal collapse [20].
The transanal endoscopic operation (TEO) platform , from Karl Storz GmbH (Tuttlingen, Germany), has been modified from the original TEM platform to allow for use with a 5 mm laparoscopic camera (Fig. 4.1b) [25]. This system also provides a 4 cm beveled rigid proctoscope that comes in two lengths (7.5 and 15 cm), with a faceplate with three ports in addition to the dedicated camera port (12, 5 and 5 mm), that accommodate conventional laparoscopic instruments. The system also includes an articulated proctoscope holder to secure the system to the operating table. Insufflation is provided with a standard CO2 insufflator and tubing, and the scope is compatible with the standard laparoscopic camera and laparoscopic tower. The TEO system does not have a built-in system for smoke evacuation, which is achieved by standard laparoscopic suctioning or venting through small valves on the platform itself. This system is lower in cost than the more specialized Wolf TEM system and seeks to decrease the operating room setup time and lessen the learning curve for TEM with the use of more familiar laparoscopic equipment [77]. It should be noted that because of the similarity between TEM and TEO rigid metal platforms, recent studies do not necessarily distinguish between the two rigid platforms and may use the terms TEM and TEO interchangeably, or refer to them as TEM or TES rigid platforms.
In 2009, transanal minimally invasive surgery (TAMIS) was described as an alternative minimally invasive endoscopic setup to resect rectal lesions [20, 21]. The original report is described using a single-incision laparoscopic port, typically used for single-incision laparoscopy, and inserting it transanally in combination with a standard laparoscopic camera, scope, and instruments, to perform submucosal or full-thickness rectal resection. Since this first report, two commercial devices, the GelPOINT Path (Applied Medical, Rancho Santa Margarita, CA) and SILS Port (Covidien, Mansfield, MA), have been FDA-approved for the use in TAMIS (Fig. 4.1c, d). Other single-incision laparoscopic platforms have been used for TAMIS, including several platforms that are not currently commercially available in the United States. One group described using a simpler and cost-effective transanal access device consisting of a surgical glove assembled onto a wound retractor inserted transanally, in combination with laparoscopic trocars and instruments [78]. TAMIS has the advantage of disposable equipment that is more widely available, less expensive, and faster to set up in the operating room than the TEM or TEO platforms. The disposable port will sometimes be sutured to the surrounding perianal tissue to avoid dislodgement [21]. The available devices have three channels that can accommodate standard laparoscopic instruments ranging from 5 to 15 mm, including both rigid and flexible-tipped scopes [22]. The use of extra-long straight laparoscopes, deflectable-tip laparoscopes, and conventional endoscopes can help overcome some of the limitations of maneuvering a rigid scope through TAMIS platforms and reduce instrument collision [79]. High definitions and 3D imaging can also be incorporated to improve image quality and depth of perception. In addition, articulating laparoscopic instruments that were designed for the use in single-incision laparoscopy can be incorporated in TEM, TEO, and TAMIS procedures in an effort to facilitate reaching difficult angles.
Recently, high-flow CO2 insufflation units (Olympus, Center Valley, PA and Stryker, San Jose, CA) have been used in conjunction with TEM/TEO and TAMIS platforms for active smoke and mist evacuation. These insufflators provide automatic smoke evacuation and high-speed CO2 insufflation that responds quickly to CO2 leaks resulting from suctioning and maintaining a stable pneumorectum and stable field of view. The Airseal® insufflation system (SurgiQuest, Inc., Milford, CT, USA) uses a cannula though which a continuous flow circuit occurs, evacuating CO2 and smoke, recirculating filtered and high-pressure CO2, and maintaining a stable pneumorectum. The 5–12 mm cannula can only be used through TAMIS platforms and has been described as a useful tool to maintain a stable pneumorectum [80].
Robotic technology has recently been combined with TAMIS, with the first clinical case of robotic transanal endoscopic resection reported in 2012 [81]. A handful of small case series have since reported preliminary outcomes of robotic transanal endoscopic resection of rectal lesions using a glove port technique , which allows for greater working angles for the robotic arms [82, 83]. Despite a cumbersome perianal setup, and increased costs associated with robotic procedures, the preliminary data demonstrates feasibility of this approach with proposed advantages of ergonomically favorable dissection and suturing.
Preoperative Preparation and Operating Room Setup
Patients typically undergo full mechanical bowel preparation and/or administration of enemas prior to surgery in order to clear the rectum and to allow for adequate visualization. Some surgeons will use enemas or full mechanical bowel preparation selectively, based on anticipation of the possibility of full-thickness excision with peritoneal entry. Most surgeons also use standard perioperative parenteral antibiotic prophylaxis as well as thromboembolic prophylaxis. General anesthesia with complete muscle paralysis is usually recommended for TES in order to avoid abdominal wall contractions during procedures and minimize CO2 leakage. One recent case report and one case series have demonstrated the safety of performing TAMIS under spinal anesthesia [69, 84].
Regarding patient positioning, patients are either placed in the supine, prone jackknife, or lateral decubitus position (Fig. 4.3). Standard operating tables are used in combination with leg stirrups or, alternatively, split leg operating tables can be used. The TEM and TEO platforms traditionally require rectal lesion to be in a dependent position for ease of operation. This preference is based on the original design of both platforms, which are beveled at their tip, with the angled camera fixed at the superior aspect of the platform. Thus, for anterior rectal lesions, the patient is typically placed in the prone jackknife position, whereas for posterior lesions, the patient is placed in dorsal lithotomy. For lateral lesions, the traditional teaching is to place patient in the lateral decubitus positioning. Most experienced TEM and TEO surgeons will perform these procedures routinely in dorsal lithotomy regardless of the location of the lesion [76]. TAMIS is usually performed in the dorsal lithotomy position, and the use of a deflectable-tip scope and articulating instruments greatly facilitates exposure and visualization during these procedures [20].
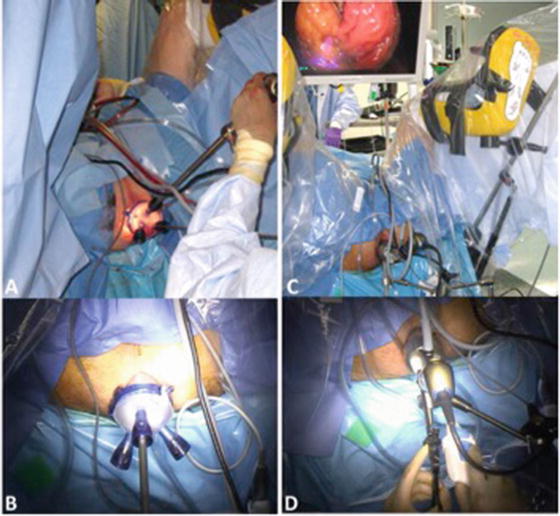
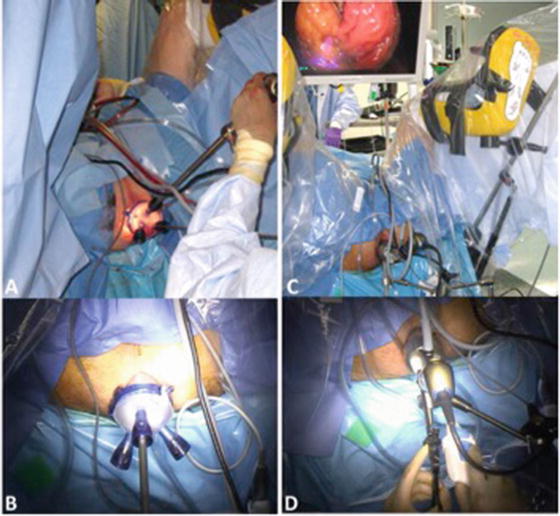
Fig. 4.3
TES setup . The patient is positioned in lithotomy position and the monitor is placed in between the patient’s legs for improved ergonomics. The TAMIS platform is inserted transanally and procedures are performed by an operator and an assistant to hold the camera (a, b). The TEM/TEO rigid platform is inserted transanally, and the platform is secured to the OR table using a U-shaped platform holder. The procedure is performed by a single operator (c, d)
One relative indication for placing patients in prone position includes preoperative anticipation of peritoneal entry during full-thickness excision of high-risk rectal lesions [65]. High-risk lesions for peritoneal entry include anterior and lateral lesions located in the upper rectum or rectosigmoid, as well as circumferential or near-circumferential lesions [61–64]. Peritoneal entry through large rectal wall defects can result in the rapid accumulation of CO2 into the abdominal cavity and collapse of the rectum. In such cases, closure of the rectal wall defect can be very difficult due to poor exposure. Preemptively positioning the patient in prone position prior these cases limits the amount of CO2 leakage into the abdominal cavity and helps maintain a stable pneumorectum throughout the case [65].
Dissection
Following patient positioning , transanal platform insertion, and CO2 distention, the lesion is localized and dissection is initiated (Fig. 4.4). By convention, the lesion is scored circumferentially with electrocautery marks to map out the planned resection margins. In the case of suspected or proven rectal invasive adenocarcinoma, this is followed by full-thickness circumferential dissection through the rectal wall until the mesorectum, or perirectal fat is reached. A 5–10 mm resection margin is usually achieved in order to maximize the likelihood of R0 resection [25, 26, 85]. Submucosal and full-thickness dissection is traditionally accomplished with monopolar cautery, using conventional reusable laparoscopic hooks, spatulas, or articulating disposable instruments based on surgeon’s preference and availability. Bipolar energy devices and ultrasonic shears can also be used to improve hemostasis and reduce dissection time. Hemostasis can also be achieved using laparoscopic clips or sutures . Some surgeons routinely excise a portion of the mesorectum attached to the segment of rectum removed in order to increase the chance of including some lymph nodes in their specimen for improved staging. Others have performed rectal sleeve resections for near-circumferential and circumferential rectal tumors. However, more extensive rectal dissection may be associated with higher morbidity, including bleeding, suture line dehiscence and leak, complex perirectal infections, and inadvertent injuries to surrounding organs, as well as postoperative urinary retention [86, 87]. In their series of 196 TEM cases, Guerrieri et al. reported two urethral injuries in male patients which occurred during wide anterior rectal dissection [86]. In addition, wider-than-indicated rectal dissection, including mesorectal dissection, may complicate or compromise the safe performance of salvage TME if warranted based on final pathology results from the TEM procedure. Scarring and inflammation form along the mesorectal plane after prior rectal dissection, which can significantly impact TME procedures.
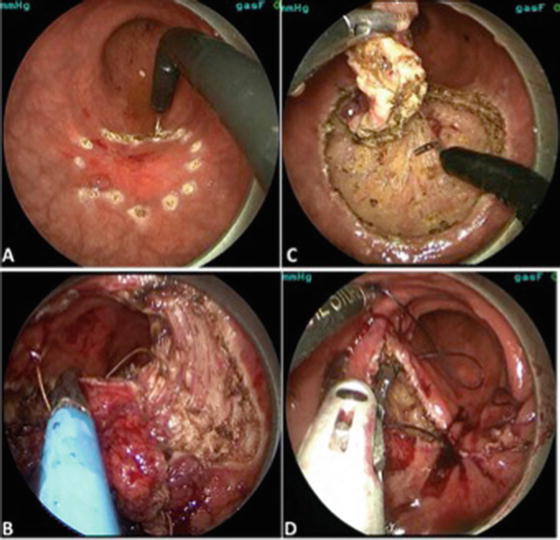
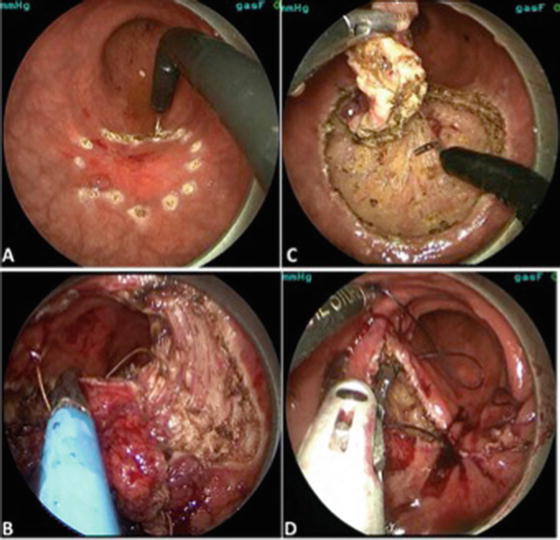
Fig. 4.4
Procedural steps for TES . Following setup and insufflation of the rectum, the lesion is scored with monopolar cautery circumferentially (a). The lesion is dissected endoscopically either along the submucosal plane (b), or full-thickness, down to the mesorectum or perirectal fat (c). Full-thickness rectal defects are closed with sutures (d)
Following full-thickness dissection, the specimen is oriented with sutures and mounted on a hard surface with pins or sutures for accurate pathologic assessment of resection margins (Fig. 4.5).


Fig. 4.5
Orientation of the TES specimen. Following exteriorization of the resected specimen, it is oriented with sutures for accurate pathologic assessment of all resection margins
Loss of Pneumorectum and Peritoneal Entry
As previously mentioned, peritoneal entry is not an uncommon occurrence during TEM and is no longer considered a complication. Overall, the reported rate of peritoneal entry during TEM ranges from 0 to 32.3% [62, 88] but across large contemporary series with more than 300 patients, that rate is lowered to 5–10.7% [89, 90]. To date, only three TAMIS series of 32–75 patients have reported a 2–9.4% incidence of peritoneal entry [20, 22, 68]. Entry into the peritoneal cavity, with subsequent difficulty maintaining adequate pneumorectum and visualization, presents a considerable technical challenge to the surgeon (Fig. 4.6). For this reason, surgeons will routinely place patients with high anterior lesions, where the risk of accidental peritoneal entry is greatest, in the prone position to mitigate the impact of CO2 leakage into the peritoneal cavity on successful closure of rectal wall defects [65]. This allows the surgeon to minimize gas losses and maintain a stable pneumorectum. Other strategies to maintain pneumorectum include complete muscle paralysis, minimizing CO2 leakage, increasing the pressure of CO2 insufflation, and decompressing the pneumoperitoneum with a Veress needle or trocar [20]. Over time, and in experienced centers as demonstrated in large contemporary TEM series, conversion rates following peritoneal entry have steadily decreased, with conversion rates ranging from 0 to 40% but averaging 10% or less [65]. Interestingly, among the three TAMIS series that reported a total of seven cases of peritoneal entry during TAMIS for upper rectal tumors, six required conversion to laparoscopy or laparotomy from inability to effectively close the rectal wall defect. This may reflect the long learning curve required for managing these complex rectal lesions, and the currently small experience with TAMIS to date. But it may also reflect technical limitations of shorter TAMIS platforms , which do not always permit adequate retraction and exposure of the proximal rectum.
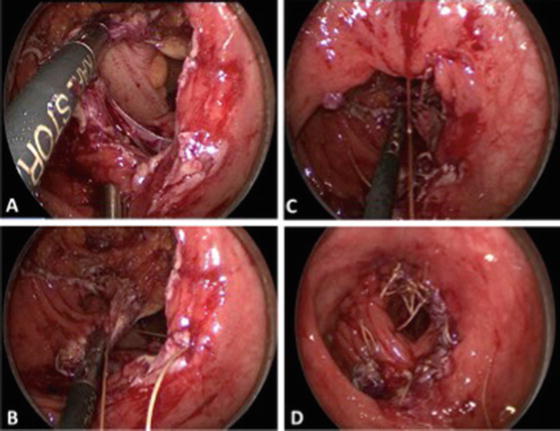
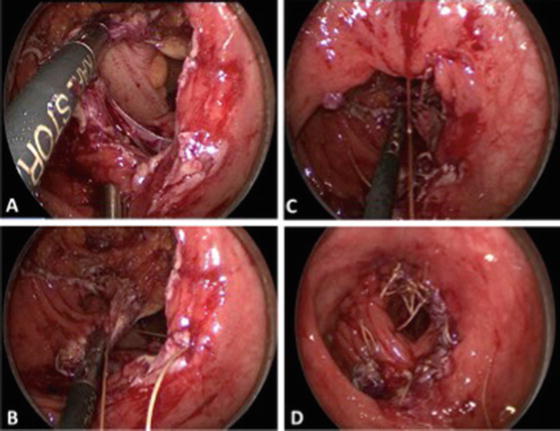
Fig. 4.6
Peritoneal entry during TES . Full-thickness resection of a rectal lesion located anterolaterally in the upper rectum results in peritoneal entry with visualization of the rectosigmoid (a). The adverse consequences of CO2 leakage into the abdominal cavity are mitigated by the prone position (b). The rectal defect is closed using interrupted and continuous absorbable sutures without adverse outcomes (c, d)
With regard to the morbidity associated with peritoneal entry, several studies have reported no increase in the rate of postoperative complications relative to TEM cases without peritoneal entry [61–65]. Notably, there has been no demonstrated increased risk of pelvic sepsis or abscess formation following peritoneal perforation. Fewer studies have evaluated the oncologic impact of peritoneal entry during TEM performed for rectal cancer. Morino et al. followed 13 patients with rectal adenocarcinoma in whom peritoneal perforation occurred during TEM [65]. At a median follow-up of 48 months (range 12–150), no cases of liver or peritoneal metastasis occurred. Two patients with T2 and T3 tumors developed local recurrence and subsequently died of lung metastases .
Rectal Defect Closure Techniques
Many techniques and devices can be employed for closing rectal wall defects during TES. In some select cases, particularly for low or posterior rectal lesions, or in cases of partial-thickness excision, the rectal wall defect can be left open, as there is some evidence that leaving the defect open does not increase complications for such lesions [91]. In a recent study by Hahnloser et al., 35 patients underwent TAMIS for lesions located at a mean of 6.4 ± 2.3 cm from the anal verge, with the rectal defect left open. This group included both full-thickness and partial-thickness defects. No increase in complications was noted between this group and the 38 patients in whom rectal defects were closed [68]. Of note, only 6% of the 35 open rectal wall defects were located anteriorly compared to 28% of 38 closed rectal wall defects. Clearly, for larger, full-thickness lesions, and in particular for high-risk lesions where peritoneal entry has occurred or is suspected, complete and airtight closure is required to decrease the risk of leak and intra-abdominal abscess formation [76, 92]. Prior to closure, particularly in the event of an incomplete bowel preparation and ongoing fecal contamination of the rectal wound , the area can be irrigated with dilute iodopovidone. Most TES surgeons close the defect with running or interrupted absorbable monofilament sutures. A variety of suture materials are described including glycolide and trimethylene carbonate (Maxon), polydioxanone (PDS), and polyglactin (Vicryl) [76]. Intracorporeal suturing devices and techniques can be used, including extracorporeal knot tiers. In order to overcome the technical difficulty of knot tying through a transanal rigid platform, the TEM instruments include an angled needle holder, and sutures can be secured with specialized silver bullets (Richard Wolf, Knittlingen, Germany). Alternatively, a V-loc barbed absorbable suture (Covidien) can be used to avoid having to make a knot. Finally, disposable automated suturing devices can facilitate knot tying including the Endo Stitch™ device (Covidien) and the Cor-Knot device (LSI Solutions, Victor, NY). If peritoneal entry occurs, some authors advocate closing the defect in two layers [76]. In cases where there is concern that the closure is not airtight, further investigation with a gastrografin enema would be recommended in order to rule out a leak .
Postoperative Management and Follow-Up
Following submucosal and low-risk full-thickness TES cases, patients are routinely discharged home on the same day [93]. Patients who have undergone full-thickness excision with peritoneal entry, or patients with extensive medical comorbidities, are typically admitted overnight for observation. Administration of postoperative antibiotics is not routinely recommended, nor is routine imaging, in the absence of clinical indications.
There are no specific guidelines for postoperative surveillance specific to patients who have undergone TES for rectal adenocarcinoma [47]. Current practice follows standard NCCN guidelines for rectal cancer surveillance, including clinical evaluation, CEA, and endoscopic surveillance by flexible sigmoidoscopy every 3–4 months for the first 3 years and every 6 months until year 5 [26, 94]. Other standard testing includes yearly CT scans until year 5 as well as surveillance colonoscopy at 1 year followed by 3 years post-resection. There is no NCCN guideline for surveillance pelvic MRI. However, following TES excision of T1 rectal tumors, particularly T1 tumors with borderline or high-risk features that were or were not treated with TME or adjuvant chemoradiation, most surgeons will recommend bi-annual or annual pelvic MRI for 5 years to rule out locoregional pelvic recurrence .
Outcomes of TES
Operating Time
The average operating time reported in large TEM and TEO case series for rectal neoplasms ranges from 70 to 95 min [28, 53, 86, 95–98]. Some smaller series have reported mean operative times as low as 45 min [35, 99]. Variations in OR time relate to size of the lesion, submucosal versus full-thickness dissection, distance from the anal verge, closure versus non-closure of rectal defects, complexity of the rectal defect closure, and management of intraoperative complications such as bleeding, CO2 leakage, and peritoneal entry . Additionally, there is a clear learning curve for TEM, with possible improvement in operative time as the surgeon becomes more experienced with the equipment [90].
A small randomized study by Serra-Aracil et al. comparing TEM and TEO in 34 eligible patients with rectal lesions found no differences in lesion characteristics, postoperative morbidity, and final pathology between the platforms used. Although there was a trend toward shorter operative time with TEO, including time to mount the equipment and perform the excision and suture closure, this difference was not statistically significant [98].
Reduced operating time from shorter operative setup and faster procedure completion are commonly cited as one of the main advantages of TAMIS over TEM/TEO as reported by its many adopters. The initial report of TAMIS reported a mean operative time of 86 min which has progressively decreased with a recent series reporting mean operating time of 57 min [21, 100]. Another series reported a median operating time as low as 45 min [69]. To date, no prospective comparative or randomized trial of TEM, TEO, and TAMIS procedures has been published comparing operating time and other perioperative variables.
Mortality and Morbidity
A major advantage of TES is the improved safety profile relative to TME [51, 101–103]. Mortality is well under 1% across most series, even in patients with multiple comorbidities who are deemed unable to tolerate a radical operation [104]. The overall complication rate following TEM is also relatively low relative to standard colorectal resections, with most complications being minor and transient. Published 30-day morbidity rates range from 6 to 23% in the largest TEM/TEO series with cohorts ranging from 262 to 693 patients [25, 53, 88, 89, 100, 101, 105]. Major complications are noted in less than 10% of cases [13, 76, 106]. The most commonly reported surgical complication following TEM is hemorrhage, which is reported in 1–13% of patients, and is usually managed non-operatively [76]. The most common nonsurgical complication is urinary retention, with incidence reported around 5% on average (range, 5–10%) [53, 89]. Other surgical complications include suture line dehiscence, which can range from minor defects usually managed non-operatively with antibiotics and bowel rest, to major defects with leakage and sepsis, requiring return to the operating room for washout and fecal diversion. Additional major TES complications include perirectal and presacral abscess, fistulas, and rectal stenosis. Rare complications include organ injury, with two cases of urethral injury reported following TEM resection of anterior-based lesions [107]. In the largest multicenter series published to date, among 693 combined TEM and TEO cases, conversion to conventional TAE or abdominal procedures was required in 4.3%, and the 30-day morbidity was 11.1%, with hemorrhage and suture dehiscence being the most common surgical complications and urinary tract infections being the most common nonsurgical complication [90].
The relatively low morbidity following TEM procedures is reflected in the short hospital stay and minimal postoperative analgesic requirement. Up to 50% of patients undergoing TEM for rectal cancer are safely discharged on the day of surgery as reported in several recent series [93]. When patients are admitted for observation, average length of hospital stay ranges from 0 to 5 days, with reasons for admission ranging from management of major medical comorbidities to observation following complex cases involving peritoneal entry [24].
In the more limited literature on TAMIS, the published incidence of postoperative complications range from 0 to 25%, with bleeding and urinary retention reported as the most common complications [22]. One review of published TAMIS outcomes between 2010 and 2013 reported a total of 29 complications among 367 patients (7.9%) treated for rectal neoplasms [108]. Bleeding occurred in 2.7% of patients and suture dehiscence in 0.5% of patients. There were no deaths reported following TAMIS, and the average length of hospital stay was only 1.9 days. In the absence of comparative studies evaluating rigid metal versus TAMIS platforms, there is no data on differences in morbidity, mortality, or length of stay between approaches .
Functional Outcomes
By virtue of the prolonged dilation of the anal sphincter by the 4 cm wide rigid and semirigid anal platforms, there is some concern that TEM, TEO, and TAMIS procedures might not only transiently impact anorectal function but might cause permanent deterioration in fecal continence, particularly in patients with compromised anal sphincter tone at baseline. Interestingly, while multiple small TEM studies have documented a transient decrease in sphincter resting pressures on anal manometry that was proportional to the duration of the procedure, resting pressures were noted to return to baseline value 12 months postoperatively [109–111]. Other objective functional measurements, such as mucosal electrosensitivity and rectal compliance, were found not to be generally affected [110]. More importantly, changes in resting anal sphincter pressures did not translate into any detrimental effects on continence. Indeed, a majority of patients reported no change and even some improvement in anorectal function following TEM for rectal lesions. In a study of 41 patients who underwent TEM, Cataldo et al. found no significant changes in the Fecal Incontinence Severity Index (FISI) or the Fecal Incontinence Quality of Life (FIQL) scores reported 6 weeks postoperatively relative to preoperative scores [112]. A recent study that longitudinally assessed anorectal function and quality of life score in 102 TEM patients at 6, 12, 26, and 52 weeks postoperatively relative to baseline values found that the general quality of life scores (EQ-5D) was significantly lower at 6 and 12 weeks but returned toward baseline at 26 weeks. Similar to prior studies, anorectal function as assessed by colorectal functional outcome (COREFO) was worse at 6 weeks postoperatively but returned to baseline at 12 weeks postoperatively [113].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree