Genetic Testing by Cancer Site: Skin
Michele Gabree
Meredith Seidel
Many hereditary cancer predisposition syndromes are associated with cutaneous findings. Identification of unique dermatologic features provides an opportunity to distinguish hereditary cancer syndromes with similar associated internal malignancies. Although skin findings are an important diagnostic tool for a number of cancer syndromes, including Cowden syndrome, Birt–Hogg–Dubé, hereditary leiomyomatosis renal cell carcinoma, and others (Table 14.1), this section will focus on skin cancer as well as tumor syndromes with cutaneous findings that are not included elsewhere in this book, including hereditary melanoma, basal cell nevus syndrome (BCNS), and neurofibromatosis type 1 (NF1) and neurofibromatosis type 2 (NF2).
The identification of dermatologic abnormalities and their association with internal malignancies often require thorough observation from clinicians. A consultation with a dermatologist may be helpful to identify specific dermatologic abnormalities. In some cases, biopsy and pathology may be necessary for a diagnosis.
Genetic Counseling
Genetic counseling for hereditary skin diseases is similar to the process for other cancer predisposition syndromes. The genetic counseling process generally includes a detailed family and medical history, risk assessment, discussion of benefits, and limitations of available genetic testing, including possible test results, discussion of medical management, and implications for family members.19 Dermatologic evaluation and review of pathology records pertaining to the cutaneous findings may provide clarification on specific dermatologic observations. Consultation with a dermatologist and/or other specialist who is knowledgeable about hereditary syndromes is often essential to a clinical evaluation. When possible, reviewing the medical records of family members is also helpful to confirm dermatologic diagnoses, as reports of some skin findings in family members may contain some inaccuracies.20
Table 14.1 Summary of Hereditary Cancer Syndromes with Cutaneous Features | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Hereditary Skin Cancer and the Neurofibromatoses
In addition to a few known single-gene disorders associated with skin cancers, confounding environmental factors, including solar ultraviolet radiation, as well as other genetic factors also are known to be associated with a varying degree of skin cancer risk. Separately, other hereditary tumor and cancer predisposition syndromes, such as NF1 and NF2, contain benign cutaneous features as common and sometimes
predominant findings. General characteristics of a hereditary cancer predisposition syndrome include multiple tumors or cutaneous features in one individual, multiple affected family members, and individuals or families with related tumors, cancers, or unique physical characteristics. In some cases, young age at onset may also suggest a higher likelihood of a hereditary syndrome.
predominant findings. General characteristics of a hereditary cancer predisposition syndrome include multiple tumors or cutaneous features in one individual, multiple affected family members, and individuals or families with related tumors, cancers, or unique physical characteristics. In some cases, young age at onset may also suggest a higher likelihood of a hereditary syndrome.
Hereditary Melanoma
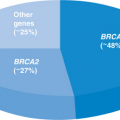
Approximately 10% of melanoma cases are attributed to hereditary predisposition. Hereditary melanoma has been associated with mutations in two genes, cyclin-dependent kinase inhibitor 2A (CDKN2A) and cyclin-dependent kinase 4 (CDK4). Mutations in CDK4 are rare and have been identified in only a few hereditary melanoma families.21 Of families with hereditary melanoma, defined as three or more diagnoses of melanoma in one family, approximately 20% to 40% will have a detectable mutation in CDKN2A.22
CDKN2A and CDK4 both function as tumor suppressors. CDKN2A encodes two transcripts: p16 and p14ARF through alternate reading frames. The majority of CDKN2A mutation-carrying families have been found to have mutations that affect the p16 protein. Mutations affecting the function of p14ARF are reportedly rare in cutaneous melanoma families.23
Phenotype
Hereditary melanoma has also been referred to as familial atypical mole melanoma syndrome.24 Although the presence of atypical moles has been associated with an increased risk for melanoma, it has not been identified as a strong predictor of CDKN2A mutation status.25,26
The penetrance of CDKN2A mutations has been observed to be dependent on geography. This is likely due to varying environmental and other genetic factors across geographic regions. A study of CDKN2A carriers selected based on positive personal and family history of melanoma observed the melanoma risk for CDKN2A mutation carriers to be 58% in Europe, 76% in the United States, and 91% in Australia.27 In a population-based study of patients with melanoma, the penetrance of CDNK2A mutations was observed to be lower (28% risk for melanoma by the age of 80 years).28 Variants in the melanocortin 1 receptor (MC1R) gene have been associated with increased CDKN2A penetrance.29 The prevalence of MC1R has been observed to differ with ethnic background and is one example of a genetic factor influencing melanoma risk that varies by geographical region.30
In addition to melanoma, other cancers have also been observed in increased frequency in CDKN2A mutation carriers. Most notably, an increased risk for pancreatic cancer has been reported in some CDKN2A mutation–carrying families.31 Less commonly, an increased risk for other cancers, including neural system tumors, nonmelanoma skin cancers, uveal melanoma, and head and neck cancers, has also been reported in individuals with CDKN2A mutations.31,32
Table 14.2 Referral Criteria for Hereditary Melanoma Genetic Counseling | ||||
|---|---|---|---|---|
|
In the United States, which is an area of moderate to high melanoma incidence, genetic counseling for hereditary melanoma has been generally recommended in families in which (1) three or more relatives are affected with melanoma; (2) one individual has three or more primary melanomas; or (3) both pancreatic cancer and melanoma are present in one family (Table 14.2).15 Early age at onset in the absence of a family history of melanoma is not highly suggestive of a CDKN2A mutation.33,34
Genetic Testing
Clinical testing for CDKN2A and CDK4 is available in the United States at several commercial laboratories. However, some of the laboratories offering hereditary melanoma testing perform analysis of only CDKN2A, given the relatively low-frequency CDK4 mutations reported.
The utility of genetic testing for CDKN2A mutations remains a source of debate. This is partly due to the relatively low frequency of CDKN2A mutations in families with melanoma. In addition, many individuals with a personal and/or family history of melanoma are under close surveillance and aware of risk-reduction recommendations; therefore, genetic test results would not alter clinical management.25 Also, the role of pancreatic cancer surveillance in CDKN2A carriers remains under investigation. Some studies have suggested that knowledge of CDKN2A mutation status improves short-term compliance to risk-reducing behaviors.35,36 However, information regarding the long-term impact of CDKN2A testing is limited at this time. The possible genetic test results for an individual undergoing CDKN2A genetic testing are shown in Table 14.3.
Individuals with a CDKN2A mutation have a 50% of passing the mutation on to their children.
Medical Management
CDKN2A mutation carriers, or individuals at 50% risk to be a carrier, should be monitored carefully for melanoma through clinical and self-examinations
(Table 14.3). In addition, CDKN2A carriers are recommended to avoid prolonged direct sunlight and utilize sun-protective clothing and sunscreen.25,37
(Table 14.3). In addition, CDKN2A carriers are recommended to avoid prolonged direct sunlight and utilize sun-protective clothing and sunscreen.25,37
Table 14.3 CDKN2A Genetic Testing Results and Medical Management Recommendations | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||
Individuals who test negative for a familial CDKN2A mutation may also have an increased risk for melanoma. However, this risk has been observed to be lower than the melanoma risk for CDKN2A mutation carriers.28
As noted in Table 14.3, CDKN2A mutation carriers, especially those with a family history of pancreatic cancer, are candidates for pancreatic cancer surveillance and should discuss the risks, benefits, and limitations of screening with a gastroenterology specialist.38 However, to date, the effectiveness of pancreatic surveillance remains under investigation.39
Basal Cell Nevus Syndrome
BCNS, also known as Gorlin syndrome or nevoid basal cell carcinoma syndrome, is an autosomal dominant syndrome associated with cutaneous findings, including basal cell carcinoma, as well as skeletal system, nervous system, and ocular abnormalities.40 Although BCNS has complete penetrance, the expression is variable.41
BCNS is thought to be relatively uncommon, and the incidence of BCNS has been estimated to be 1:30,827 to 1:57,000.42 The variable expression may cause difficulty in diagnosing BCNS.
BCNS has been associated with mutations in the patched gene 1 (PTCH1) gene. PTCH1 functions as a tumor suppressor in the sonic hedgehog (Shh) pathway, which is also involved in embryonic development.43 Chromosomal abnormalities of 9q22.3 region, which includes PTCH1, have been reported in a few individuals with features of BCNS as well as other features, including short stature, developmental delay, and seizures.44 Rarely, mutations in other genes, including SUFU and PTCH2, have also been reported in individuals with features of BCNS.45,46
Phenotype
The phenotype of BCNS is variable, and some characteristics are present at different life stages. Therefore, it is important to obtain a complete medical history, including physical examination and dermatologic, cardiac, and gynecologic examinations as well as radiologic studies to confirm a diagnosis of BCNS.
The clinical manifestations of BCNS include the following:
Skin
Basal Cell Carcinoma
Approximately 50% to 75% of individuals with BCNS will develop basal cell carcinomas.47 Typically, basal cell carcinomas develop in the late teens through the 30s, but some published reports have indicated the detection of basal cell carcinomas in early childhood in individuals with BCNS. The presence of basal cell carcinomas is also dependent on other factors, including skin type and radiation exposure, including sun exposure.40,41
Noncancerous Cutaneous Features
Skeletal
Skeletal abnormalities, including rib and spinal abnormalities, are reported with increased frequency in BCNS. The majority of individuals with BCNS are reported to have macrocephaly.48
Central Nervous System
Ectopic Calcification
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree