General Approach to the Treatment of Diabetes Mellitus
Ramachandiran Cooppan
Since the last edition of this textbook, major scientific advances have increased our understanding of the pathophysiology underlying both type 1 and type 2 diabetes and have fueled new approaches to therapy. New insights into the mechanism of insulin action and insulin resistance, greater understanding of the mechanisms of controlling insulin secretion, and advances in genetics and in immunology have contributed to this explosion of knowledge. Furthermore, a number of randomized prospective studies demonstrating the benefits of tight glycemic control and the availability of new oral therapies and insulin formulations provide a compelling rationale for improving the overall level of diabetes care.
The results of the Diabetes Control and Complications Trial (1), the Kumamoto Trial (2), and the United Kingdom Prospective Diabetes Study (3) have provided conclusive evidence that tight glycemic control will prevent the onset, as well as delay the progression, of the long-term microvascular complications of type 1 and type 2 diabetes. A more recent follow-up of the Kumamoto study (4) noted that the optimal degree of glycemic control to prevent or delay complications is a glycosylated hemoglobin (HbA1c) level of less than 6.5%, a fasting glucose level of less than 110 mg/dL, and a 2-hour postprandial blood glucose level of less than 180 mg/dL.
DIABETES AS A WORLDWIDE HEALTHCARE PROBLEM
Diabetes mellitus has become an international healthcare crisis that requires new approaches to prevention and treatment. During the last 20 years, the prevalence of diabetes has increased dramatically in many parts of the world. Although genetic factors play a role in the etiology, especially of type 2 diabetes, the growing problem of obesity that parallels improved economic status in some developing countries is a major environmental factor in this epidemic of diabetes. On the other hand, in many parts of the developing world, low birth weight and maternal malnutrition during pregnancy may be a major factor underlying the insulin resistance syndrome and thus in an increased risk of diabetes in later life.
At least 120 million people throughout the world suffer from type 2 diabetes, and it is projected that the number will increase to 220 million by the year 2010. This disease is now a worldwide public health issue that not only costs many nations millions of dollars for healthcare but also robs many developing economies of their most precious resource, their workers. Data almost a decade old gave an estimated prevalence of type 2 diabetes in the United States of 14 million persons that caused an estimated 300,000 deaths and resulted in healthcare expenditures of $100 billion (5).
Some of the world’s most highly indebted and poorest nations do not have sufficient resources to pay back their debt and to also provide care for patients with diabetes, adding to the problem. In these areas, a lack of adequate insulin supplies is a major problem for young children with type 1 diabetes, and many do not survive more than 1 year after onset of disease. Solutions to this problem must be forthcoming, because treatment for patients with type 1 diabetes exists and should be widely distributed (6).
CHANGING DIAGNOSTIC CRITERIA FOR DIABETES
In 1997, the American Diabetes Association (ADA) changed the diagnostic criteria for diabetes mellitus and recommended that
the use of Roman numerals for the two major forms of diabetes mellitus be discontinued and that Arabic numerals 1 and 2 be used instead. The earlier change in the classification from insulin-dependent diabetes mellitus (IDDM) and non-insulin-dependent diabetes mellitus (NIDDM) to type 1 or type 2 was an attempt to move away from a treatment-based classification to one based on underlying pathophysiology. This new system removed the confusion that emerged when patients classified as having NIDDM under the old nomenclature were treated with insulin because of disease progression. Would these patients now be classified as having IDDM or were they merely patients with NIDDM who now required insulin therapy? The pathophysiologic approach allows for the spectrum of changes in the underlying disease process that develop with time and provides a rationale for treatment changes based on this progression.
the use of Roman numerals for the two major forms of diabetes mellitus be discontinued and that Arabic numerals 1 and 2 be used instead. The earlier change in the classification from insulin-dependent diabetes mellitus (IDDM) and non-insulin-dependent diabetes mellitus (NIDDM) to type 1 or type 2 was an attempt to move away from a treatment-based classification to one based on underlying pathophysiology. This new system removed the confusion that emerged when patients classified as having NIDDM under the old nomenclature were treated with insulin because of disease progression. Would these patients now be classified as having IDDM or were they merely patients with NIDDM who now required insulin therapy? The pathophysiologic approach allows for the spectrum of changes in the underlying disease process that develop with time and provides a rationale for treatment changes based on this progression.
In making these changes, the ADA also revised the diagnostic criteria for diabetes and introduced a new category, impaired fasting glucose (IFG). The old criteria required a fasting plasma glucose level of 140 mg/dL or higher or a glucose level of 200 mg/dL or higher 2 hours after a 75-g glucose challenge to establish a diagnosis of diabetes. These older criteria also were in line with the recommendations of the World Health Organization. The new criteria were developed to allow earlier diagnosis of diabetes that would, in turn, lead to early treatment and, it is hoped, to a reduction in diabetes-related complications (7). Studies in Egypt and the United States demonstrated a correlation between the development of retinopathy and a fasting glucose level of more than 108 to 116 mg/dL (8,9). Not all groups are enthusiastic about these changes in the diagnostic criteria. Some are concerned that undo emphasis on the fasting glucose concentrations will reduce the use of the oral glucose tolerance test that may be necessary to identify individuals with impaired glucose tolerance (IGT), which is associated with greater rate of progression to clinical diabetes and is a risk factor for cardiovascular disease (10,11). Furthermore, there is concern that the new criteria may increase the prevalence of diabetes in many parts of the world and strain already limited healthcare resources (12,13), although, of course, the new criteria do not increase the actual prevalence of diabetes but only that of diagnosed diabetes.
Advances in molecular biology and genetics have helped to elucidate the mechanism of insulin action and to identify specific gene mutations [e.g., glucokinase gene in maturity-onset diabetes of the young-2 (MODY 2)] that can lead to diabetes. In addition, outcome data clearly support the benefits of strict glycemic control in retarding both the development and progression of the long-term microvascular complications in both type 1 and type 2 diabetes mellitus. These studies on glucose control have been complemented by studies on macrovascular disease that demonstrate the major benefits derived from aggressive treatment of hypercholesterolemia and elevated blood pressure in patients with diabetes.
The increase in the number of oral medications for treating type 2 diabetes has now made it possible for providers not only to choose therapies based on the underlying pathophysiology of diabetes but also to use drugs that work synergistically by addressing different pathophysiologic abnormalities. The benefits of this approach, which often allows the use of submaximal doses of different agents, are improved glycemic control and a reduction of the adverse effects of the medications used. The challenge in type 2 diabetes is to start treatment early and to use combination therapies that address both the insulin resistance and insulin secretory defects of the disease. The introduction of rapid-acting human insulin, as well as the new long-acting insulin analogues, has made it possible to approximate normal insulin secretion through the use of basal and premeal (bolus) insulin regimens.
The “cure” for diabetes still eludes us. However, the progress made in the development of new approaches to growing and transplanting β-cells and in immunosuppressive therapy lends hope to the possibility that transplanted β-cells, even those not rendered immunoneutral, will survive for the long term and render patients with type 1 diabetes insulin-independent (14).
The approach to a chronic disease such as diabetes requires treatment goals that include both the maintenance of the well-being of the affected individual and the prevention of the long-term complications associated with the disease. The relationship of glucose control to the microvascular complications has been validated; the challenge is to make practical use of this information by improving the delivery of appropriate care. This requires close collaboration among all members of the healthcare team involved in the care of patients with diabetes. Despite the dramatic results of the Diabetes Control and Complications Trial (DCCT), for most patients, there has been no major shift in the care of type 1 diabetes that will provide the benefits noted in the intensive therapy trials. It is gratifying that those patients who were in the intensive treatment arm of DCCT and are now part of the Epidemiology of Diabetes Interventions and Complications (EDIC) trial have continued to benefit from participation in the intensive treatment arm for as long as 4 years after the trial’s end. Unfortunately, this group has experienced some deterioration in overall glycemic control outside the environment of a rigorously controlled clinical trial (15). The cost-effectiveness of intensive treatment also has been examined and found to be worthwhile compared with the cost of treating the complications when they occur. To achieve aggressive goals of glycemic control, self-monitoring of blood glucose (SMBG) must be a standard for all patients. Moreover, patients should have access to the appropriate monitoring equipment, independent of the type of diabetes, and with the frequency of testing determined by the medical professionals and the patient.
Many variations of practice guidelines for diabetes are now available; however, adherence to these guidelines has not been optimal in many instances (16). There are many reasons for this, and these must be assessed carefully if progress is to be made in this area. Current treatment guidelines are based on outcomes data derived from controlled clinical trials and extensive physician experience. A mechanism is now needed to translate these guidelines into a format that will be both practical and realistic in clinical practice. The care of patients with a chronic disease such as diabetes, while benefiting from the modern revolution in information technology, still has as its basis the caring, compassionate, and understanding relationships between the patient and members of the healthcare team. Unfortunately, current reimbursement systems do not support the establishment or maintenance of these relationships and thus work against efforts to provide optimal care to patients with diabetes.
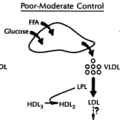
The major clinical issue in patients with type 2 diabetes, in addition to that of achieving symptomatic control of hyperglycemia, is the enormous risk of cardiovascular disease and the problems arising from microvascular complications. An appreciation of the interrelationships of the various risk factors that lead to coronary heart disease and the benefits of treating these vigorously is growing rapidly. Multiple studies on cholesterol lowering [Scandinavian Simvastatin Survival Study (4S) and Cholesterol and Recurrent Events trial (CARE)] (17,18); blood pressure control [United Kingdom Prospective Diabetes Study (UKPDS) and Hypertension Optimal Treatment (HOT) study] (19,20); and the use of aspirin (21), inhibitors of angiotensin-converting enzyme [Heart Outcomes Prevention Evaluation trial (HOPE)] (22), and β-blockers reveal significant benefits in patients with diabetes. While these randomized controlled clinical trials have been conducted primarily in subjects
without diabetes, the subgroups with diabetes also had significant reductions in major cardiovascular events and death. The recent data from the Atherosclerosis Risk in Communities (ARIC) Study showed that the risk for diabetes in patients with hypertension is increased by two and a half. The study also noted that the risk of development of diabetes was not increased by thiazide diuretics but was increased by β-blockers. However, the benefits of the use of β-blockers following myocardial infarction have been validated in the literature, so the risk of developing diabetes should be considered of secondary importance in this group of patients (23).
without diabetes, the subgroups with diabetes also had significant reductions in major cardiovascular events and death. The recent data from the Atherosclerosis Risk in Communities (ARIC) Study showed that the risk for diabetes in patients with hypertension is increased by two and a half. The study also noted that the risk of development of diabetes was not increased by thiazide diuretics but was increased by β-blockers. However, the benefits of the use of β-blockers following myocardial infarction have been validated in the literature, so the risk of developing diabetes should be considered of secondary importance in this group of patients (23).
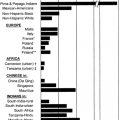
The treatment plan for patients with diabetes also will be affected by the prevalence of the disease in the population. The prevalence of type 2 diabetes is higher in certain ethnic groups, such as Native Americans (especially the Pima Indians) (24), Hispanic Americans, African Americans, and Asian Americans (25,26,27). For many of these groups, access to good medical care is affected by factors such as socioeconomic status, insurance coverage, cultural background, language barriers, individual and group health beliefs, educational level, and peer behavior. These factors present special problems that will have to be addressed if these patients are to achieve optimal outcomes.
Diabetes in the older population also is a special issue because of the increase in the prevalence of diabetes with aging, the multiple other conditions being treated in the elderly population, and the risks associated with polypharmacy. There is an urgent need to approach the treatment of diabetes in these patients with enthusiasm and to set appropriate goals for therapy. Treatment must be individualized, and the relationship of risks to benefits must always be carefully evaluated, but age, per se, is not a reason to alter the target goals for glycemic control. Although most elderly patients with diabetes have type 2 disease, many of them have type 1 (insulin-dependent diabetes) disease—not only because type 1 diabetes can present for the first time in the elderly but also because many patients with type 1 diabetes are living long enough to be included in the elderly group. The elderly do not always present with the classical symptoms and signs of hyperglycemia, so the physician must consider this diagnosis, especially in those with neuropathy, nonhealing ulcers, and recurrent infections (28).
Although this chapter will focus on the general approach to the treatment of the patient with diabetes in the outpatient setting, the principles also apply to inpatients. The material presented here is intended as a general overview of the treatment of diabetes; other chapters in this text are devoted to specific issues.
AN INITIAL APPROACH
Once the diagnosis of diabetes has been established, the question of initiating therapy must be addressed. Those patients who present with diabetic ketoacidosis or who are markedly hyperglycemic and symptomatic should be admitted to the hospital for urgent treatment. The need for hospitalization at diagnosis applies primarily to patients with type 1 diabetes, especially children.
At this initial stage, the physician or healthcare professional who is seeing the patient should obtain a detailed history and perform a complete examination with appropriate laboratory testing. The future progression of the patient’s care will be affected by a number of factors, including the physician’s treatment philosophy, the patient’s healthcare beliefs and competence at self-care, and the availability of a team consisting of a dietitian, diabetes educator, exercise physiologist, and, when needed, social workers and psychologists. Unfortunately, not all components of this team may be available in the general office practice; however, most communities do have these resources, and patients should be referred to them, as appropriate, to achieve optimal glucose control.
The approach must consider the “whole person” with diabetes, not just the levels of glycemic control to be achieved or the therapy to be used to accomplish this (i.e., insulin or oral antidiabetic therapies). To this end, a strong, integrated team approach is the one most likely to succeed. Although, as noted above, the complete team may not exist in most cases, the physician and the patient can make considerable progress together, with other components of the team, especially the diabetes educator and dietitian, coming from the community.
The Patient History
A detailed history is the foundation of good diabetes care. Knowledge about the age of the patient and the clinical presentation often help the physician determine whether the patient has type 1 or type 2 diabetes. This is not a laboratory-validated diagnosis but a clinical assessment to assist in choosing the initial treatment. The clinician bases the classification on aspects of the patient’s history such as age, body weight, family history, duration of symptoms, and the results of the blood glucose and the HbA1cdeterminations. Considerable heterogeneity exists, especially in type 2 diabetes, in the clinical presentation as well as in the underlying pathophysiology. Some patients actually may have a slowly progressive form of autoimmune diabetes. These tend to be younger adults and generally require insulin therapy relatively soon. These patients can be diagnosed by measuring certain autoimmune markers in the blood, such as antibodies to insulin and glutamic acid decarboxylase (GAD). The increasing prevalence of type 2 diabetes in adolescents makes it necessary to differentiate type 1 from type 2 diabetes in this group of patients. Another problem is the difficulty in assigning a definite date for the onset of diabetes, particularly for type 2 diabetes, which can be asymptomatic for many years, a determination that has implications concerning the risk for diabetes complications. At the Joslin Clinic, both patients with new-onset diabetes and those seeking consultation for existing disease are mailed a detailed metabolic questionnaire about symptoms, current therapy, family history, exercise patterns, and other medical problems and therapies. Particular attention must be paid to histories of coronary artery disease, peripheral vascular disease, hypertension, and renal disease in the patient and the family. Patients also are asked to keep a record on a dietary assessment sheet or in a food diary for 2 or 3 days, including the times of their meals and the types and quantities of foods eaten. This information helps the dietitian design an appropriate meal plan based on the patient’s food preferences and lifestyle. With new information-technology systems, patients can access these questionnaires electronically and enter the information from home. This will avoid mail delays, help get the information in a timely manner, and enhance the patient’s visit with the physician.
Physical Examination
The physical examination is a fundamental part of the initial evaluation. Special attention should be paid to the height and weight, body mass index (BMI), blood pressure (lying down and standing up), and vascular status. A careful examination of peripheral pulses and auscultation of carotid and femoral vessels for bruits is extremely important in obtaining a baseline for the future. The neurologic examination must include a careful search for evidence of neuropathy. Not only are muscle strength and reflexes tested, vibration, position sense, and appreciation
of application of a 10-g monofilament to the feet must also be assessed. While these clinical methods lack the precision of a detailed laboratory neurologic evaluation, they still permit the clinician to obtain a baseline picture and to obtain further investigations in appropriate patients.
of application of a 10-g monofilament to the feet must also be assessed. While these clinical methods lack the precision of a detailed laboratory neurologic evaluation, they still permit the clinician to obtain a baseline picture and to obtain further investigations in appropriate patients.
In a study of 189 patients with diabetes and 88 control subjects, Thivolet et al. (29) used a graduated tuning fork to measure the sensitivity of the feet to vibratory sensations and noted that 51% of patients with clinical symptoms of neuropathy in the extremities, 70% of those with absent tendon reflexes, and 75% of those with abnormal nerve-conduction velocities had limited vibration sensation. On the other hand, the study by Dyck et al. (30) revealed the problems present in assessing the epidemiologic data on diabetic neuropathy. Part of the problem is the variety of clinical types of neuropathy and the characterization of neurologic dysfunction. With multiple clinical entities and variable presentation, the best the clinician can do is to look for and document the presence of neuropathy. In a recent study, Perkins et al. (31) reported on the usefulness of four simple tests: 10-g Semmes-Weinstein monofilament examination, superficial pain sensation, vibration testing by the on-off method, and vibration testing by the timed method. They found excellent sensitivity and specificity for each of the tests from the reported operating characteristics. The timed-vibration method took longer to perform than the others, but each of the other tests took less than 10 seconds and should therefore be part of the annual examination for neuropathy. If the history and physical examination are atypical for diabetes, an additional workup should be undertaken and a referral to a neurologist considered.
The physician also should pay special attention to the patient’s feet, carefully palpating the dorsalis pedis and posterior tibial, popliteal, and femoral pulses. Skeletal deformities such as hallux valgus, bunions, callouses, and hammertoes must be carefully documented. The combination of vascular disease and neuropathy is the major cause of foot infection and nontraumatic amputation in patients with diabetes.
Finally, a careful funduscopic examination is done, although this should not substitute for an evaluation by an ophthalmologist with experience in diabetic eye disease. Some new methodologies using nonmydriatic digital retinal imaging serve as an excellent screening technique to prioritize the need for formal ophthalmologic evaluation.
Laboratory Studies
The choice of laboratory tests performed is in part determined by the clinical presentation of the patient. If the patient is in a state of diabetic ketoacidosis or is symptomatic from marked hyperglycemia, the degree of hyperglycemia, the acid-base status, electrolytes, and the presence of acetone are urgently assessed. For the nonacute situation, at the patient’s first visit, the minimum tests required are a complete urinalysis and determinations of blood glucose and HbA1c. It is now usual to add to these a chemistry panel that includes measurements of lipids, liver and kidney function, and electrolytes and a complete blood count. If possible, the lipid measurements should be done on the patient in the fasting state to obtain an accurate determination of the triglyceride level. It may be necessary for the patient to make a separate visit to the office or laboratory for these tests. In most cases, lipids also are evaluated on the first visit. Total cholesterol, triglycerides, high-density cholesterol, and low-density cholesterol are determined. Lipid studies are an important aspect of diabetes assessment because of the high risk of macrovascular disease, especially in the patient with type 2 diabetes (32).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree