Extravasation
Taher Abu Hejleh
Gerald H. Clamon
The accidental extravasation of chemotherapeutic agents during intravenous administration has been reported in approximately 0.1% to 6.0% of patients.1,2 Cancer patients may be more prone to drug extravasation because of multiple venipunctures, phlebitis limiting future sites of venous access, lymphedema due to prior surgery, and generalized debility. The consequences of extravasation can vary from mild erythema and discomfort to severe pain, tissue necrosis, skin ulceration, and invasion of deep structures such as tendons or joints. Factors that affect the degree of tissue damage include the vesicant nature of the extravasated drug, the concentration of the extravasated agent, the volume infiltrated into the tissues, the site of infiltration (i.e., dorsum of the hand versus antecubital fossa versus forearm), and possibly the subsequent management by the physician or nurse. Other local reactions that do not involve drug extravasation also occur. Local phlebitis is common with nitrogen mustard (mechlorethamine), and vinorelbine, with 1,2-bis (2-chloroethyl)-1-nitrosourea (BCNU; carmustine) because of its diluent.3 Hypersensitivity reactions, often called flare reactions, with erythema and urticaria along the course of the vein, can occur with anthracyclines such as doxorubicin (Adriamycin), and daunorubicin.4 Unfortunately, these are among the drugs that may give the most severe extravasation reactions, and a very careful and cautious approach must be taken to any local reaction due to these agents.
The time course of the injury after drug extravasation varies. With the most toxic agents, such as the anthracyclines, nitrogen mustard, and the vinca alkaloids, the injury often comes on gradually. With the anthracyclines, a stinging type of pain is often felt during the extravasation. Over 7 to 10 days, erythema, heat, and pain develop, followed by progression to ulceration. The ulceration may then enlarge for 2 to 3 months.5 The edges are often red and painful, and the lesions may have a yellow necrotic base that does not heal spontaneously.4,6 Full-thickness skin necrosis may occur, and if the ulcer is over tendons or neurovascular structures, these tissues may also undergo necrosis. The tissues are thin over the dorsum of the hand, at the antecubital fossa, and over the flexor surface of the wrist, and damage to the underlying tendons and nerves can lead to joint contractures and chronic damage. In the absence of surgical intervention, many of the deep and painful lesions never heal.7 The occurrence of pain during administration of a vesicant drug should be an alert that extravasation may have occurred, even if no visual evidence is present. Agents that can cause skin ulceration are listed in Table 14.1.
MECHANISMS OF TISSUE INJURY
Several mechanisms have been proposed for severe damage caused by anthracyclines such as doxorubicin and its analogs. These agents lead to the development of free radicals that are toxic to the tissues. The ability of these agents to bind to DNA further impedes the ability of the damaged tissues to heal. Studies have shown that doxorubicin is retained in the extravasated area for months.8 It has been hypothesized that DNA-doxorubicin complexes are released from dead cells and taken up by adjacent cells by endocytosis. This sets up a continuing cycle of doxorubicin damage. Such retention and recirculation of the doxorubicin suggest that early surgical excision may be valuable in preventing further spread of injury.
Histologic studies of chemotherapy-induced ulcers in humans have been carried out 2 to 3 months after extravasation.5,7,9 Blood vessels in the ulcer are damaged, but at the margins, the blood vessels are viable. Inflammatory cells are rarely present, which suggests that the use of steroids to reduce inflammation would not be effective therapy. Dimethyl sulfoxide (DMSO) and a-tocopherol are antioxidants that might neutralize free radicals formed by anthracyclines. These agents appear to be active antidotes in some animal models and in some clinical trials in humans.
The application of cold may slow the drug diffusion throughout the tissues, prevent drug uptake into cells, and thereby interrupt the cycle of damage. In small animals and in humans, the application of cold seems to decrease injury and ulceration due to doxorubicin extravasation. Although numerous other agents have been proposed, their lack of efficacy as antidotes in small animal trials has obviated their use in human clinical trials. Dexrazoxane has become an FDA approved antidote for the management of anthracycline extravasation.10,11,12 There are reports of its successful use in patients with doxorubicin and epirubicin infiltrations. The doses of Dexrazoxane recommended are 1,000 mg/m2/day for 3 days starting within 6 hours of the injury. Dexrazoxane binds to iron, displacing it from anthracycline-iron complexes, and this may prevent free radicals from causing tissue injury. Originally approved for the prevention of anthracycline cardiotoxicity, only one of 57 patients with extravasation treated with Dexrazoxane required surgery.12
Animal Models
Extravasation injury due to anthracyclines and other chemotherapeutic drugs has been studied in the rat, the mouse, and
the pig. Rodent skin may be a less appropriate model than pig skin for the study of extravasation in humans. Rodent skin differs from human skin in that rodents have a thin vascular muscle layer fixed to the skin.13 Because of the greater vascularity, anthracycline injury in rodents is less apt to progress to ulceration. Intradermal injection is required to induce ulceration in most animal models. Most human accidental extravasations are likely subcutaneous. In animal models, intradermal injection is necessary to cause ulceration; subcutaneous injection causes minimal lesions. Increasing the dose of doxorubicin concentration or the volume injected, or both, causes larger ulcers with longer times to healing. Concentrations below 0.01 to 0.2 mg per ml injected intradermally will not cause severe ulceration, and concentrations below 0.25 mg per ml injected subcutaneously do not produce severe damage.14,15 Studies in rats that were given intradermal doxorubicin, actinomycin D, mitomycin, or BCNU, and then either potential antidotes or surgical excision of the damaged area, showed superior healing with surgical excision. Early surgical excision followed by a re-excision of nonviable tissue 1 week later led to the best healing.16 With doxorubicin injury in rats, neither hydrocortisone, propranolol, nor isoproterenol was of benefit. At increasing doses of DMSO and α-tocopherol, doxorubicin injury was alleviated in rats.17 Similarly, DMSO and α-tocopherol are effective in reducing mitomycin- and actinomycin D-induced damage in rats. DMSO and a-tocopherol did not help with BCNU dermal injury.
the pig. Rodent skin may be a less appropriate model than pig skin for the study of extravasation in humans. Rodent skin differs from human skin in that rodents have a thin vascular muscle layer fixed to the skin.13 Because of the greater vascularity, anthracycline injury in rodents is less apt to progress to ulceration. Intradermal injection is required to induce ulceration in most animal models. Most human accidental extravasations are likely subcutaneous. In animal models, intradermal injection is necessary to cause ulceration; subcutaneous injection causes minimal lesions. Increasing the dose of doxorubicin concentration or the volume injected, or both, causes larger ulcers with longer times to healing. Concentrations below 0.01 to 0.2 mg per ml injected intradermally will not cause severe ulceration, and concentrations below 0.25 mg per ml injected subcutaneously do not produce severe damage.14,15 Studies in rats that were given intradermal doxorubicin, actinomycin D, mitomycin, or BCNU, and then either potential antidotes or surgical excision of the damaged area, showed superior healing with surgical excision. Early surgical excision followed by a re-excision of nonviable tissue 1 week later led to the best healing.16 With doxorubicin injury in rats, neither hydrocortisone, propranolol, nor isoproterenol was of benefit. At increasing doses of DMSO and α-tocopherol, doxorubicin injury was alleviated in rats.17 Similarly, DMSO and α-tocopherol are effective in reducing mitomycin- and actinomycin D-induced damage in rats. DMSO and a-tocopherol did not help with BCNU dermal injury.
Table 14-1 Antineoplastic Agents Associated with Extravasation Injury | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
In a mouse model, the addition of cold to the extravasated area reduced doxorubicin injury; heat to the area exacerbated the extent of damage.18 In a mouse model, DMSO and α-tocopherol were not able to reduce doxorubicin injury.19
Hyperbaric oxygen concurrent with doxorubicin injury has been investigated in animals. Monstrey et al.20 found that giving hyperbaric oxygen for 3 days before injection of doxorubicin intradermally to rats and for 7 days after led to greater injury. This would be consistent with other reports that they cite of doxorubicin injury in animal models showing no improvement with hyperbaric oxygen. However, this does not preclude that hyperbaric oxygen could be of benefit in healing poorly vascularized ulcers that developed long after exposure to the doxorubicin and failed to heal with other conservative measures.
At least three trials in pigs gave mixed results for DMSO as an antidote for doxorubicin injury. In one trial, cooling the area reduced doxorubicin damage, but DMSO was of no benefit.21 However, in a second trial using pigs, DMSO was effective, and in a third trial, the results with DMSO were equivocal.22,23 Hyaluronidase has been reported to decrease vinca alkaloid injury in a mouse model. Simple dilution with normal saline was also effective in reducing vinca injury.24 Mild skin heating alone reduced vinca alkaloid ulceration significantly as well, whereas cooling exacerbated vinca alkaloid extravasation injury. Thiosulfate has been demonstrated in an animal model to reduce injury due to nitrogen mustard.25
Clinical Trials
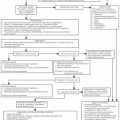
Most trials in humans involve the management of doxorubicin extravasation. Once extravasation has occurred, aspiration of any free drug through the intravenous cannula before it is removed can reduce the extent of injury. At the M. D. Anderson Hospital, in Houston, Texas, Larson2 reported 50 consecutive cases of drug extravasation that involved doxorubicin or vincristine, which were managed uniformly. The extremity was placed in a sling, and the patient was instructed to apply ice for 20 minutes four times a day for 3 days. The patient then reported to a surgeon for evaluation. If the patient had persistent pain or evidence of progressive necrosis, a wide local excision was performed. Often the wound needed to be covered with a biologic covering and later skin grafted. Using cold packs without injections of antidotes, only 12 of 50 patients required surgery. Early surgery in cases of extravasation reduced the extent of later injury in 40 patients with extravasation.16 However, even with surgery, residual damage has frequently been noted in patients with drug administered near the elbow, the wrist, or the back of the hand.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree