Rima Khabbaz, Beth P. Bell, Anne Schuchat, Stephen M. Ostroff, Robin Moseley, Alexandra Levitt, James M. Hughes Keywords acute respiratory infections; antibiotics; antimicrobial resistance; avian influenza; Campylobacter; carbapenem-resistant Enterobacteriaceae; chikungunya; cholera; Clostridium difficile; coronavirus; Cryptosporidium; dengue; diarrheal disease; Ebola hemorrhagic fever; emerging infectious diseases; epidemiology; Escherichia coli; foodborne disease; gastroenteritis; H1N1; H3N2; H5N1; H7N9; health care–associated infections; Heartland virus; human bocavirus; human metapneumovirus; immunizations; infectious diseases; influenza; Marburg hemorrhagic fever; measles; MERS-CoV; methicillin-resistant Staphylococcus aureus; mumps; norovirus; One Health; pandemic influenza; pertussis; reemerging infectious diseases; Salmonella; SARS; Shigella; vaccine-preventable diseases; vaccines; variant influenza A; vector-borne diseases; Vibrio cholerae; West Nile virus; zoonotic diseases
Emerging and Reemerging Infectious Disease Threats
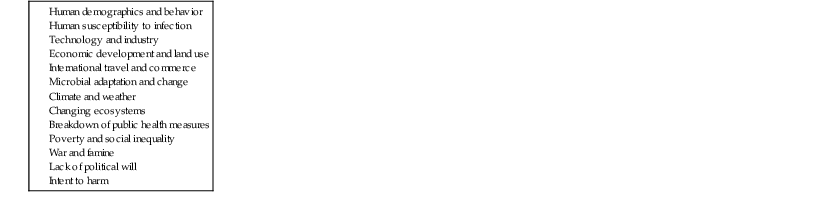
Throughout history, infectious diseases have been inextricably linked with human health, affecting the development and advancement of societies as well as human evolution.1,2 Those linkages remain well defined today, as infectious pathogens find new ways to exploit human vulnerabilities and elude control efforts across a highly connected world. Widespread movement of people, animals, and goods, exploding population numbers, urban development, environmental degradation, centralized food production, and other contributing factors (Table 14-1) have given microbes rapid and easy access to new populations and geographic areas and spawned a host of emerging and reemerging infectious diseases—the majority of which are zoonotic (Table 14-2).3 With their remarkable adaptability, emerging infections can spread quickly and gain strongholds to become endemic diseases, as most profoundly demonstrated by the decades-long pandemic of human immunodeficiency virus (HIV) infection and acquired immunodeficiency syndrome (AIDS).
TABLE 14-1
Factors That Contribute to the Emergence and Reemergence of Infectious Diseases
Data from Smolinski MS, Hamburg MA, Lederberg J, eds, for the Committee on Emerging Microbial Threats to Health in the 21st Century, Board on Global Health, Institute of Medicine. Microbial Threats to Health: Emergence, Detection, and Response. Washington, DC: National Academy Press; 2003.
TABLE 14-2
Examples of Recent Outbreaks, Pathogen Discoveries, and Other Notable Infectious Disease Events
| YEAR | EVENT |
| 2000 | Outbreak of Rift Valley fever in Saudi Arabia and Yemen, representing the first reported cases of the disease outside the African continent |
| 2003 | Global outbreak of severe acute respiratory syndrome (SARS) caused by a previously unknown coronavirus associated with Chinese horseshoe bats |
| 2003 | Cases of monkeypox in the United States linked to exotic pets imported from Central Africa |
| 2003 | Reemergence of avian influenza A (H5N1) in Southeast Asia and subsequent outbreaks in Africa |
| 2005 | Marburg hemorrhagic fever outbreak in Angola |
| 2005-2006 | Large outbreak of chikungunya in the Indian Ocean islands of Réunion and Mauritius |
| 2006 | Rift Valley fever outbreak in Kenya |
| 2007 | Ebola hemorrhagic fever outbreak in the Democratic Republic of the Congo |
| 2007 | Outbreak of Nipah virus encephalitis in Bangladesh |
| 2007 | First detection in Italy of mosquito-borne transmission of chikungunya fever, previously detected only in parts of Africa and South and Southeast Asia |
| 2007 | Hemorrhagic fever outbreak in Uganda caused by a new stain of Ebola: Bundibugyo Ebola virus |
| 2007 | Outbreak of Marburg hemorrhagic fever in Uganda |
| 2008 | Ebola-Reston virus detected in pigs in the Philippines |
| 2008 | Ebola-like outbreak in Zambia due to a previously unknown virus: Lujo hemorrhagic fever virus, an arenavirus related to Lassa fever virus, which is associated with rodents |
| 2009 | Outbreak of severe fever with thrombocytopenia syndrome (SFTS) in China caused by a novel phlebovirus (the SFTS virus) |
| 2009 | Discovery of two novel tick-borne pathogens in the United States: the Heartland phlebovirus in Missouri and a pathogenic Ehrlichia species in Wisconsin and Minnesota |
| 2009-2010 | Influenza pandemic caused by a new influenza strain, influenza A(H1N1) |
| 2009-2010 | Locally transmitted dengue in Florida, representing the first cases acquired in the continental United States outside the Texas-Mexico border since 1945 |
| 2012 | Ebola hemorrhagic fever outbreaks in Uganda and the Democratic Republic of the Congo |
| 2012 | Outbreak of Marburg hemorrhagic fever in Uganda |
| 2011-2012 | Influenza cases in the United States traced to a variant swine influenza A(H3N2) virus carried by pigs exhibited at agricultural fairs |
| 2012 | Outbreak of hantavirus pulmonary syndrome in Yosemite National Park, California |
| 2012 | A novel rhabdovirus (Bas-Congo virus) identified by whole-genome sequencing as the cause of an outbreak of acute hemorrhagic fever in the Democratic Republic of the Congo |
| 2012-2013 | Outbreak of severe respiratory disease in the Middle East caused by a novel coronavirus (MERS-CoV) that belongs to the same viral family as the SARS coronavirus |
| 2012-2013 | Influenza cases in China traced to avian influenza A(H7N9) virus in poultry |
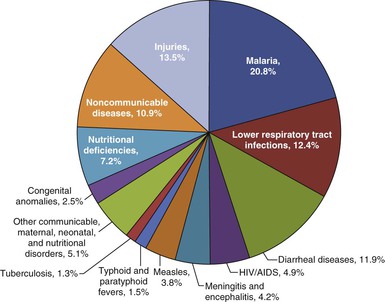
Data from the Global Burden of Disease Study 2010 (GBD 2010), a landmark collaboration of 486 scientists from 302 institutions across 50 countries,4 indicate that nearly one fourth of the estimated 52.8 million deaths that occurred in 2010 were associated with infectious diseases.5 From 1990 to 2010, overall deaths from communicable diseases declined, with significant decreases in mortality from lower respiratory tract infections (from 3.4 to 2.8 million) and diarrheal diseases (from 2.5 to 1.4 million).5 However, infectious diseases remained leading killers, especially among young children (Fig. 14-1) and accounted for large burdens of disability-adjusted life years worldwide.5,6 Although deaths from HIV infection/AIDS peaked in 2006 and have since showed steady declines owing to fewer new infections and increased availability of antiretroviral therapy and care, HIV infection/AIDS remains a leading cause of disease burden and death—responsible for an estimated 1.5 million deaths in 2010.5 Tuberculosis and malaria also continue to exact a tremendous toll, each causing approximately 1.2 million deaths in 2010.5 The multifactorial impact of infectious diseases is most prominent in low-income countries, with infectious diseases causing severe morbidity, impeding economic development, and compromising political stability.
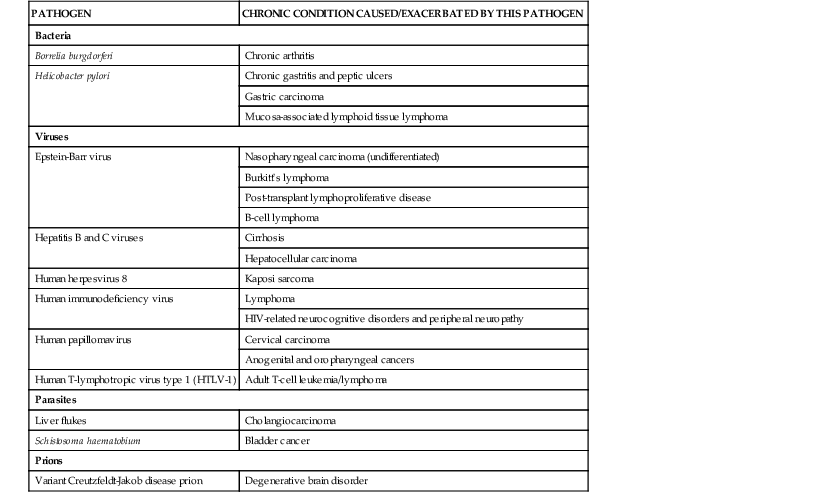
Beyond infectious diseases, microbial agents have been identified as the cause or contributing factor in a number of chronic diseases (Table 14-3). In 2008, approximately 2 million new cancer cases were linked to infections.7 Among the leading causes of cancer-related deaths, three are caused by infectious agents: hepatocellular carcinoma by hepatitis B and C viruses, cervical cancer by human papillomavirus, and gastric cancer by Helicobacter pylori bacteria. Many other potential infectious/chronic disease linkages are also being explored, including Chlamydia pneumoniae and multiple sclerosis,8,9 Alzheimer’s disease,9 and atherosclerosis10; enteroviruses and type 1 diabetes11,12; and rhinoviruses and childhood asthma.13 In addition, several genetic factors have been shown to influence infectious disease susceptibility and disease progression (Table 14-4) and hundreds of others are under investigation.14
TABLE 14-4
Examples of Genetic Factors That Influence Susceptibility to Disease or Disease Progression
| GENETIC FACTOR | DISEASE INFLUENCE |
| Alleles of the chemokine receptor gene CCR5 | Partial protection against acquisition of HIV and development of acquired immunodeficiency syndrome |
| Globin gene alleles (e.g., sickle globin and α- and β-thalassemias) | Partial protection against malaria |
| Lack of the Duffy blood group on red cells (due to a mutation in a chemokine receptor gene) | Complete protection against Plasmodium vivax malaria |
| Blood group O | Increased susceptibility to severe cholera |
| HLA alleles | May influence susceptibility to infection or course of disease with HIV, hepatitis B virus, measles, hantavirus pulmonary syndrome, malaria, tuberculosis, human papillomavirus infection, and coccidioidomycosis |
HIV, human immunodeficiency virus; HLA, human leukocyte antigen.
Modified from Levitt AM, Khan AS, Hughes JM. Emerging and re-emerging pathogens and diseases. In: Cohen J, Powderly WG, Opal SM, eds. Infectious Diseases. 3rd ed. St. Louis: Mosby; 2010.
The past few decades have provided numerous examples of the ongoing threat of infectious diseases and the ability of microbes to evolve, adapt, and survive. In particular, acute respiratory viruses are often among the most recognized emerging and reemerging infectious diseases because of the high disease burden they produce. Examples in the past decade include a novel coronavirus that resulted in the 2003 global outbreak of severe acute respiratory syndrome (SARS),15 pandemic influenza A (H1N1) in 200916; a newly recognized coronavirus causing severe disease in 2012 (Middle Eastern respiratory syndrome coronavirus [MERS-CoV])17; and avian influenza A H7N9 in China in 2013.18 Emerging and reemerging vector-borne infections also remain priorities, as mosquito-borne viruses such as dengue and chikungunya continue to appear in new areas and tick-borne diseases continue their steady rise. In addition, increased attention is being given to environmental fungi as a cause of human and animal infections. Recent examples include the emergence of Cryptococcus gattii infections in the U.S. Pacific Northwest,19,20 increasing numbers of Coccidioides infections, which are a major cause of community-acquired pneumonia in California and the southwest United States,21 and novel fungal infections as a cause of health care–associated infections (HAIs).22
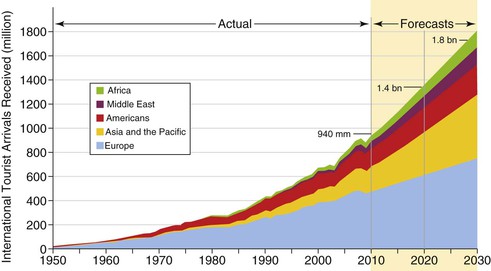
International trade and travel along with globally mobile populations present particular challenges for controlling infectious diseases, highlighting concerns for spread of known infections such as tuberculosis23 and vaccine-preventable diseases24 along with introduction of new threats.25 In 2011, international tourist arrivals approached 1 billion worldwide, and they are expected to nearly double over the coming decades (Fig. 14-2).26 Moreover, today’s globalized food supply has resulted in an increasing number of foodborne illnesses, many of which have severe consequences—especially for more vulnerable populations such as children, immunocompromised individuals, and the elderly. Also on a global level is the growing problem of resistance to antimicrobial agents, which continues to impede treatment and control efforts for an increasing number of pathogens.
Reemerging Vaccine-Preventable Diseases
The development of safe, effective vaccines coupled with large-scale immunization programs represents the ultimate solution to infectious diseases.27 Routine childhood immunization in the United States prevents approximately 20 million illnesses and 42,000 premature deaths, while saving nearly $70 billion in direct and societal costs for each birth cohort vaccinated.28 Although vaccination led to the eradication of smallpox in 1980 and has brought the world closer than ever to eradication of poliomyelitis, vaccine-preventable diseases can reemerge even in the setting of high-functioning immunization programs. A variety of factors contribute to outbreaks of vaccine-preventable diseases in the vaccination era (Table 14-5).29–32 Recently, countries in the Americas and Europe have confronted the reemergence of measles, mumps, and pertussis owing to diverse underlying causes.33–35
TABLE 14-5
Factors That Contribute to the Reemergence of Vaccine-Preventable Diseases
| FACTOR | SELECTED EXAMPLES | REFERENCES |
| Failure to vaccinate by health care system | Missed opportunities related to clinician practice, financial, or system constraints Weak or interrupted immunization services, as in humanitarian emergencies | 29, 44 |
| Failure to be vaccinated due to patient or parental refusal or deferral | Personal belief and religious exemptions Vaccine hesitancy | 32, 33 |
| Vaccine failure, including moderate or low vaccine efficacy and waning of immunity over time | Mumps vaccine efficacy in the setting of high force of infection Waning of immunity after acellular pertussis vaccination | 34, 35 |
| Pathogen “escape” from vaccine-induced immunity | Serotype replacement including capsular switching in Streptococcus pneumoniae | 31 |
Most resurgences of vaccine-preventable diseases stem from low immunization coverage. In many parts of the world, weak primary health care systems and limited access to the most vulnerable populations result in many children being unimmunized. More recently, reduced vaccine acceptance in several affluent countries has emerged as a threat to protecting communities from vaccine-preventable diseases. Whereas in the United States less than 1% of children receive no vaccines at all,36 some parents refuse one or more vaccines or decide to delay or increase intervals between vaccinations.
Measles
Two doses of measles-containing vaccines provide 95% vaccine efficacy, but at least 94% of the population must be vaccinated to ensure herd immunity, or population protection. Infants too young to be immunized and people who are immune compromised depend on herd immunity for protection. Accumulation of susceptible people in a community can result in periodic outbreaks when measles virus is circulating.30 Endemic transmission of measles has been interrupted in the United States since 2000,37 but travelers to areas where the virus still circulates account for 50 to 100 importations to the United States most years. Aggressive public health investigation of each suspected measles case is conducted to limit spread of the virus. Recently, several measles outbreaks in the United States have been associated with transmission among people who have not been vaccinated, intentionally, due to personal beliefs. In 2011, 222 measles cases occurred in the United States, the largest number of annual cases reported since 1996.38 The most important source of imported virus in 2011 was Europe, where large outbreaks affected multiple countries. A very large outbreak in France (where an estimated 20,000 cases occurred)39 was linked with importations to multiple countries in the Americas.38,40 Public health response to each outbreak is expensive.24 Because measles is rarely seen in the United States, missed diagnosis can lead to sustained exposures particularly in health care settings (Fig. 14-3).41 Ensuring appropriate infection control practices and complete immunization histories or evidence of immunity among health care workers is especially important given the infectiousness of measles virus.

Although in the Americas endemic transmission of measles has been eliminated and in the Western Pacific Region reaching this target is near, measles continues to cause more than 100,000 deaths each year—primarily in developing countries.42 Enormous progress in measles immunization through supplemental immunization activities and increasing routine coverage, particularly in Africa, has led to a 74% reduction in worldwide measles deaths.43 Despite this progress, the weak underlying immunization systems, famine, limited access associated with political disruption, and delayed emergency campaigns explain resurgences of measles in the Horn of Africa and southern Africa.44 Low first-dose measles coverage and long intervals between campaigns offering second-dose opportunities allow rapid accumulation of children susceptible to measles and can lead to large outbreaks. Poor vaccine acceptance in selected communities, ranging from the Roma communities45 to anthroposophists in Switzerland has led to sizable outbreaks in Europe as well.46
Mumps
Although mumps has decreased by nearly 99% since the prevaccination era in the United States, several large outbreaks have occurred in the United States and Europe in the past decade.34,47,48–51 Outbreak-associated disease has occurred mainly in adolescents and young adults. Despite high two-dose coverage, importation of mumps virus has been linked to outbreaks in summer camps,52 college campuses,47,49,53 and religious schools.34,51 These outbreaks were difficult to control, and although the highest risk occurred among unvaccinated persons, many case-patients had received one or two doses of mumps-containing vaccine, consistent with only 80% to 85% vaccine efficacy for one- and two-dose regimens.48,50 Although factors associated with disease include intense crowding, there is no evidence to support immune escape.54 Recent outbreaks have been notable for very little transmission to the broader community.
Although some proponents exist, the value of administering a third dose of mumps-containing vaccine in outbreaks that occur despite high two-dose coverage has been unclear because disease tends to be decreasing by the time additional doses are provided.55 Because most mumps outbreaks have occurred in unusual settings where there is extreme crowding or extensive personal contacts and most mumps is self-limited and relatively mild, it is unlikely major investments will be made to attempt to improve the efficacy of mumps vaccines.
Pertussis
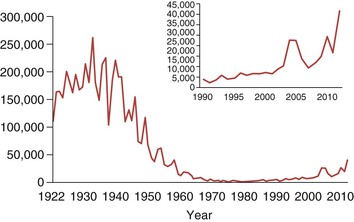
Despite decades of vaccination with first the whole-cell pertussis vaccine and, since the 1990s, acellular pertussis vaccine, pertussis is currently the least well-controlled vaccine-preventable disease in the United States. Cyclical increases are typical for pertussis, but since the 1990s the United States has experienced a continuing rise in incidence that exceeds changes due to better laboratory diagnostics or disease reporting (Fig. 14-4). The highest rates of disease, hospitalizations, and fatalities occur among infants younger than 1 year of life.56 Reported cases in teens and older children have been increasing since 2010.57 It has become increasingly clear that the transition from whole-cell pertussis virus vaccine “backbone” to acellular vaccines has changed the epidemiology of pertussis.
In 2010, California reported the highest rates of pertussis in 50 years. A retrospective analysis conducted there revealed vaccine efficacy was more than 95% within 3 years of receiving the last dose of acellular pertussis but decreased substantially by 5 years since vaccination.35,58 This explained the predominance of 7- to 10-year olds in the 2010 resurgence. By 2012, high rates of disease occurred in Washington State and several other areas,57 with surprising increases also noted among 11- and 13-year olds. Questions have been raised about whether there is differential performance of Tdap booster vaccinations among teenagers who had received acellular vaccines as young children compared with the earlier experience of teenagers who received Tdap after earlier exposure to whole-cell vaccines. Although some have speculated that bacterial strain changes noted recently might account for disease resurgence,59 the dominant view is that acellular vaccines provide good short-term protection but provide immunity that wanes more rapidly than initially expected. Program priorities in this context are to target reduction of deaths, which mainly affect infants in the first few months of life. Hence, recent recommendations for women to be vaccinated during every pregnancy are a priority for disease control.60
Acute Respiratory Tract Infection
Infections involving the respiratory tract represent one of the most dynamic areas for emerging and reemerging diseases, producing dramatic examples such as the first recognized outbreaks of legionellosis in the 1970s and hantavirus pulmonary syndrome in the 1990s. Examples in the 21st century include newly recognized pathogens such as human metapneumovirus (first identified in 2001),61 the coronavirus associated with SARS (identified in 2003),15 human bocavirus (identified in 2005),62 pandemic influenza A (H1N1) (identified in 2009),16 and a Middle Eastern novel coronavirus associated with severe respiratory illness identified in 2012.17 Other newly recognized respiratory viruses include two additional coronaviruses (NL63 and HKU1), novel human polyomaviruses KI and WU, rhinovirus groups C and D, and parechoviruses, although in some instances the role of these agents as pathogens is still being clarified.63 More virulent strains of known respiratory pathogens have also emerged. Examples of this phenomenon include human disease associated with avian influenza viruses (especially highly pathogenic avian influenza A [H5N1] and avian influenza H7N918,64), severe disease due to adenovirus type 14,65 and extensively drug-resistant tuberculosis.66
Acute respiratory tract infection constitutes a broad category of diseases that include infections of both the upper and lower respiratory tracts, such as acute pharyngitis, epiglottitis, bronchitis, pneumonia, and influenza. Although upper respiratory tract infections are capable of causing severe illness, virtually all (98%) respiratory disease–related deaths are a consequence of infection of the lower respiratory tract, especially pneumonia. Acute respiratory infections remain the leading cause of mortality from infectious diseases in the United States and around the world. The World Health Organization (WHO) estimates that 4.2 million deaths resulted from lower respiratory tract infections in 2004, accounting for 7.1% of all deaths that year.67 Among persons who died of lower respiratory tract infections, 70% (2.9 million) were residents of low-income countries. Lower respiratory tract infections are the number one cause of death in the developing world. Even in high income countries, lower respiratory tract infections are the fourth leading cause of death, responsible for 4% of all-cause mortality. Mortality from lower respiratory tract infections has the greatest impact on young children. On a global basis, 42% of all deaths from lower respiratory tract infections (mostly due to pneumonia) occur in children younger than 5 years of age.67 Significant influenza- and pneumonia-associated mortality also occurs in persons older than 65 years of age and in individuals with chronic underlying pulmonary disease. In the United States, influenza and pneumonia are the leading cause of infectious disease–related mortality and the eighth most frequent cause of death.68
Human Metapneumovirus
In 2001, human metapneumovirus (hMPV) was first reported as a cause of acute respiratory tract infections when the virus was isolated from specimens collected over a 20-year period from hospitalized children in the Netherlands with undiagnosed upper and lower respiratory tract illnesses.61 Subsequent serologic and virologic analyses of banked specimens have demonstrated evidence of hMPV infection as far back as the 1950s, and genetic studies suggest the virus is considerably older.61,69
A paramyxovirus, hMPV is closely related to respiratory syncytial virus (RSV), another member of the Paramyxoviridae subfamily of Paramyxoviridae.69,70 These related viruses have many clinical and epidemiologic features in common, and coinfections with these two pathogens have even been described.71 Studies examining whether hMPV and RSV coinfections produce more severe illness have shown conflicting results.71
Since hMPV was first identified, major strides have been made in our understanding of the impact of this agent, which appears similar to other major viral respiratory pathogens. It is known to occur globally in both high- and low-income countries, and by 5 years of age virtually all children demonstrate evidence of prior hMPV infection.72 Clinically significant illness and severe disease most commonly occur in children younger than 2 years of age, but hMPV-related illness can occur throughout childhood.73,74 In most studies, this virus (either alone or with copathogens) has been identified in 2% to 20% of children with acute respiratory tract infections, and in 3% to 7% of children hospitalized with acute respiratory tract infections or fever.69,73 Variation in rates of hMPV detection is likely due to patient selection criteria, sample collection, and diagnostic test methods. In contrast, hMPV is rarely (<1%) identified in children or adults who are not ill and when found is usually present in much lower titers than when detected during illness.69,73,75 A recent multiyear, multicenter prospective study suggests that hMPV produces 20,000 hospitalizations, 263,000 emergency department visits, and 1 million outpatient visits annually among children younger than 5 years of age in the United States.75 Because disease is also found in older children and in adults, these numbers represent an unknown proportion of the overall burden of illness due to hMPV. Multiyear studies of hMPV infection show that incidence varies from year to year and by season, with most infections in temperate locations occurring in winter and early spring.70
In children, most severe hMPV disease manifests as pneumonia or bronchiolitis and a substantial proportion of hospitalized children have underlying medical conditions, particularly asthma.73–76 Intensive care can be necessary and fatal illnesses have occurred in children with hMPV infections.77 Human metapneumovirus has also been associated with childhood upper respiratory tract infections (up to 10% in some series) as well as acute otitis media.70
Most infections with hMPV in adults are mild, but severe disease can occur, especially in the elderly and in persons with chronic pulmonary disease or congestive heart failure.78,79 This virus has been estimated to involve 3% to 7% of acute respiratory tract infections and 4.5% of acute respiratory tract infection hospitalizations in adults.79 Outbreaks associated with hMPV have been reported in both children and adults, especially among long-term institutionalized elderly, with case-fatality rates as high as 33%.79,80 As with RSV, hMPV can produce severe and recurrent disease in immunocompromised hosts, including transplant recipients, those with hematologic malignancies, and HIV infection.70,81 Ribavirin and immune globulin have been used to treat severe disease but have not been systematically assessed, and efforts are underway to develop candidate vaccines against hMPV.69,82
Genetic analyses have demonstrated two major hMPV types, designated groups A and B, with two subtypes (1 and 2) within each group; subtype variants have also been reported.69 The geographic distribution of groups and subtypes changes over time, and multiple variants can cocirculate. Periodic shifts in predominant circulating strains are thought to coincide with upsurges in disease incidence and severity. In some studies, group A viruses have been associated with more severe disease compared with group B viruses, although other series have found the opposite result or have not suggested a difference in disease severity between the two groups.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree