Direct-to-consumer Personal Genome Testing and Cancer Risk Prediction
Cecelia A. Bellcross
Patricia Z. Page
Dana Meaney-Delman
A 32-year-old woman presents for her annual physical examination. The patient indicates her sister was diagnosed with breast cancer at age 39 years. The clinician refers the patient for genetic counseling and schedules her for a baseline mammogram. The patient goes online and discovers she can learn her “genetic risk” for breast cancer for a few hundred dollars. She is very reassured when her results come back indicating she has a “7.2% lifetime risk of developing breast cancer, which is 40% less than for females of European ancestry.” On the basis of these results, she cancels her mammogram. At her next annual visit, her breast examination reveals a concerning lump in her left breast. The patient is ultimately diagnosed with a stage IIB triple-negative invasive ductal carcinoma. The delayed cancer genetics evaluation reveals a strong paternal family history of breast and ovarian cancer, and she is found to carry a BRCA1 mutation.
A 35-year-old man sees an ad for a $99 special on personal genome testing and sends in his sample. The report he receives back indicates he is at increased risk for prostate cancer. He talks with his parents to ask about prostate cancer in the family and learns instead that several individuals in his mother’s family had early colon cancer. Intrigued by this, he asks his doctor about a connection between colon and prostate cancer, and the doctor refers him to a cancer genetic specialist who works with the family and ultimately determines they carry a Lynch syndrome gene mutation.
A 25-year-old with a low risk of breast cancer—based on family history and other traditional risk factors—is given the “one size fits all perfect gift” of a personal genome scan that will tell her about her genetic risk for more than “200 diseases and conditions.” When she learns her breast cancer risk is “50% greater than the average women” and is in the “red zone,” she schedules a consultation with a breast surgeon and requests a mammogram. She is recommended to have a repeat mammogram in 6 months to follow microcalcifications. However, because of her anxiety, a biopsy is performed, and result of which is negative. While waiting for her biopsy results, she tells her sister that she had a positive genetic test for breast cancer, whose physician then orders BRCA1/2 testing.
Although the above scenarios are hypothetical, they are quite plausible and are used to illustrate some of the concerns—and possible benefits—associated with direct-to-consumer (DTC) availability of genomic-based tests, which provide risk information for health conditions such as cancer.
In this chapter, we describe the history and methodologic considerations behind DTC genomic profiling, using examples that focus on cancer risk prediction. We explore the literature regarding consumer and provider knowledge and utilization of DTC genetic testing, and the controversy that has surrounded this industry. In addition, we address policy recommendations and regulatory actions, and the changing landscape of the DTC genetic testing market in response. Finally, we take a brief look at public health implications of DTC genetic testing and the future of genomic-based medicine.
Definition, History, and Methodologic Considerations
What is DTC Genetic Testing?
DTC genetic testing refers to genetic tests that are marketed to the public, where the consumer is able to order the test online or by phone, usually without the assistance of a health care provider. Although the term DTC genetic testing has been used in many contexts, our focus will be tests that scan for multiple, common DNA variants associated with disease, as opposed to tests for rare single-gene conditions or DTC marketing.
According to the Genetics and Public Policy Center, as of August 2011, there were 27 companies offering DTC genetic testing for more than 250 health conditions and traits.1 Along with information about ear wax type, dancing ability, or risk-taking tendencies, one can learn about genetic risks for multiple, common, and serious health conditions such as Alzheimer disease, diabetes, heart disease, and cancer. These companies vary in the types of tests they offer, and how their risks are calculated, but share the commonality that although the tests are performed in a Clinical Laboratory Improvement Amendment certified laboratory, those involving genomic risk profiling have not undergone research-based evaluation of clinical validity or utility and are not Food and Drug Administration regulated.
The data from the Genetics and Public Policy Center included information on 11 companies offering DTC genetic testing for a total of 44 different types of cancer.1 Nine of these companies did not require involvement of a health care provider to order testing. Table 3.1 provides information on the five companies that still offer testing in this manner, along with information on the types of cancers included and approximate cost.
The Development of the DTC Genetic Testing Industry
DTC genetic testing was a natural entrepreneurial offshoot of the Human Genome Project. In particular, the advent of genome-wide association studies (GWASs)—which
first appeared in the literature in 2005 and have risen almost exponentially since—sought to find genetic markers associated with common diseases, in part to fulfill the promise of the Human Genome Project to provide personalized genomic medicine.7 These studies use millions of “single-nucleotide polymorphisms” (SNPs) that have been found throughout the human genome. Essentially, a case-control approach is used, where the genomes of 100s to 1,000s of individuals with a particular condition (e.g., breast cancer) and a population of controls without the condition are scanned for SNPs that show differential distribution between the two groups, resulting in odds ratios for the associated genotypes.
first appeared in the literature in 2005 and have risen almost exponentially since—sought to find genetic markers associated with common diseases, in part to fulfill the promise of the Human Genome Project to provide personalized genomic medicine.7 These studies use millions of “single-nucleotide polymorphisms” (SNPs) that have been found throughout the human genome. Essentially, a case-control approach is used, where the genomes of 100s to 1,000s of individuals with a particular condition (e.g., breast cancer) and a population of controls without the condition are scanned for SNPs that show differential distribution between the two groups, resulting in odds ratios for the associated genotypes.
Table 3.1 Cancer Risk Prediction Tests Offered by DTC Genetic Testing Companies Without Involvement of a Health Care Provider (As of April 15, 2012) | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Early GWASs were plagued by multiple erroneous assumptions that discredited most of the initial results. However, over time, more rigorous methodology, involving much larger sample sizes, higher levels of statistical significance, replication, and control for population stratification, was used. These studies have resulted in identification of more than 1,400 SNPs with “true” associations for more than 237 human traits and diseases, including breast, prostate, colon, lung, thyroid, and many other cancers.8
The rise of DTC genetic testing very closely followed the early influx of GWAS publications, with many companies entering the market in 2008.9 These companies not only capitalized on this research, but also recognized the limited access to genetic testing in the existing health care infrastructure and the desire of consumers for convenience, privacy, and the right to own their own genetic information.9
Although the success of GWASs in identifying SNP-based disease associations cannot be argued, the initial promise of this approach in allowing for “personalized genomic medicine” has yet to be realized, despite the claims of the DTC testing companies. This is in part because the vast majority of SNPs are associated with very low odds ratios for common diseases—typically in the range of 1.1 to 1.4—and thus have minimal impact on absolute risk.10,11,12,13 Furthermore, identified SNPs account for only a small proportion (5% to 10%) of the known heritability of most common diseases.13,14,15 Finally, much remains unknown regarding the impact of both gene–gene interactions and gene–environment interactions on an individual’s predisposition to disease.16
DTC Genomic Profiling for Cancer Risk
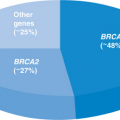
Most cancer genetic testing available DTC is performed using genomic profiles, which involve testing for multiple SNPs that have been associated with a specific cancer. The most common method used to calculate the person’s disease risk involves conversion of the odds ratios of the genotype at each SNP to relative risks, then combining them in a simple multiplicative model. This overall relative risk is then compared with the general population risk for this cancer, to provide a percent increase and/or a revised absolute risk (Fig. 3.1). This method is highly dependent on the background population risks used, and assumes all SNP effects are independent.
Although most of the companies use well-validated SNPs, they do not use all the same ones in the same way. This means that the disease risk estimates provided may differ from company to company, with one predicting an increased and the other an average or decreased risk. Evidence of this phenomenon has been reported in several publications and attributed to differences in the number/type of SNPs, variation in risk modeling approaches, and average general population risks used.17,18,19 Table 3.2 illustrates the differences in the number of SNPs used and their reported effects for the two largest DTC genomic profiling companies (23andMe2 and deCODE3) for some common cancers.
Perhaps, even more concerning are data that suggest that as new disease-associated SNPs are added to a specific disease profile, a person’s risk may be reclassified.16,20 Both 23andMe and deCODE provide consumers with ongoing updates,
such that a person who originally received a “lower than average” result for a specific cancer may find themselves at “average” or “above average” risk in the future. Although the possibility of risk reclassification is disconcerting, so too is the finding by Singleton et al.21 that only half of the websites of companies offering genomic risk profiling discussed how consumers would receive updated risk information, or even that their risks could change.
such that a person who originally received a “lower than average” result for a specific cancer may find themselves at “average” or “above average” risk in the future. Although the possibility of risk reclassification is disconcerting, so too is the finding by Singleton et al.21 that only half of the websites of companies offering genomic risk profiling discussed how consumers would receive updated risk information, or even that their risks could change.
It is also important to clarify that the cancer risk estimates provided do not adjust for family history of the cancer or take into account other known risk factors. For example, a man who is morbidly obese, smokes two packs of cigarettes a day, and has a father with colon cancer at age 50 years will be given the same predicted risk for colon cancer as a man without these risk factors who has the same SNP profile.
Value of Genomic Risk Profiling for Cancer
All of the above issues underline the importance of considering both clinical validity and utility when interpreting the results of SNP-based genomic profiles as a measure of disease risk. Specifically, how accurate is the risk prediction provided by the SNP profile, and will this information result in changes in medical management or health
behaviors that improve outcome? The accuracy of the risk prediction can be measured by the area under the receiver operating characteristic curve (AUC), which plots sensitivity against the false-positive rate. A test that predicts no better than chance will have an AUC of 0.5—essentially a flip of the coin—whereas a test with an AUC of 1 can perfectly predict who will and will not develop the disease. Unfortunately, few studies have been conducted that provide the data needed to assess the clinical validity of most cancer risk prediction tests based on genomic profiling. Those that have been published; however, suggest these profiles have limited predictive ability.
behaviors that improve outcome? The accuracy of the risk prediction can be measured by the area under the receiver operating characteristic curve (AUC), which plots sensitivity against the false-positive rate. A test that predicts no better than chance will have an AUC of 0.5—essentially a flip of the coin—whereas a test with an AUC of 1 can perfectly predict who will and will not develop the disease. Unfortunately, few studies have been conducted that provide the data needed to assess the clinical validity of most cancer risk prediction tests based on genomic profiling. Those that have been published; however, suggest these profiles have limited predictive ability.
Table 3.2 Comparison of Two Companies’ SNP profiles for Breast, Colon, Ovarian, and Prostate Cancer | ||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||
For example, Wacholder et al.22 reported an AUC of only 0.597 for a breast cancer profile involving 10 SNPs. Even adding these 10 SNPs to the Gail risk model for breast cancer only slightly improved its predictive ability from an AUC of 0.58 to 0.62.22,23 Similarly, in the case of prostate cancer, Zheng et al.24 reported an AUC of 0.61 using age, geographic region, and family history, which rose only to 0.63 when the five strongest SNPs were added to the model. Although AUC data are not available for many of the cancers listed in Table 3.1, the use of a small number of SNPs with odds ratios typically less than 1.4 would suggest similarly poor predictive accuracy. Furthermore, the question of whether the use of genomic profiling leads to appropriate alterations in medical management or behavior that actually results in improved health outcomes (i.e., clinical utility) remains, at this point, essentially unanswered.25
It should be noted that although the majority of testing performed by DTC genetic testing companies focuses on these SNPs with low cancer-associated odds ratios, there are exceptions.
For example, 23andMe evaluates three SNPs that are essentially markers for the three BRCA1/2 Ashkenazi Jewish founder mutations. In sharp contrast to the other breast cancer risk SNPs, identification of one of these BRCA1/2-related mutations is highly predictive of disease, with odds ratios for breast and ovarian cancer of 10- to 20-fold and mean lifetime risks of 65% and 40%, respectively.26 The significance of being negative for the three BRCA1/2-associated SNPs is primarily relevant for individuals of Jewish ancestry. Those of other ethnic groups would require full sequence analysis of these genes, which is not available DTC. Thus, DTC genomic profiling for cancer risk may result in the unexpected revelation of a significant hereditary cancer risk or false reassurance that such a risk has been ruled out. Some companies also test for SNPs in genes that have been suggested as modifiers of BRCA1/2 penetrance, which could be misinterpreted as actual BRCA mutations.
Consumer Issues Associated with DTC Genetic Testing
Awareness, Attitudes, and Utilization
Despite the widespread availability of DTC genetic testing for the past several years, it is unclear the extent to which consumers are either aware of or accessing DTC genetic testing for health
reasons. In a 2008 cross-sectional survey of US consumers, whereas 22% of individuals were aware of DTC genetic testing for health risks, only 0.3% had actually accessed such tests.27 A 2008 study in the United Kingdom found only 13% were aware of internet-based personal genome testing.28 Data obtained from the 2009 Behavior Risk Factor Surveillance System of four co-operating states (combined n = 16,439) demonstrated awareness of DTC genomic profiling for health risks ranged from 15.8% to 29.1%, although fewer than 1% of participants in each state reported having used the testing.29 Even in one study of social networkers, almost half of the participants (47%) were aware of DTC genetic testing, yet only 6% had ever undergone the testing.30,31 Although 23andMe reports that more than 100,000 individuals have accessed their test,32 a 2010 publication, which used the website traffic of three largest companies as a proxy for test uptake, concluded that the demand for genomic profiling was relatively low.33
reasons. In a 2008 cross-sectional survey of US consumers, whereas 22% of individuals were aware of DTC genetic testing for health risks, only 0.3% had actually accessed such tests.27 A 2008 study in the United Kingdom found only 13% were aware of internet-based personal genome testing.28 Data obtained from the 2009 Behavior Risk Factor Surveillance System of four co-operating states (combined n = 16,439) demonstrated awareness of DTC genomic profiling for health risks ranged from 15.8% to 29.1%, although fewer than 1% of participants in each state reported having used the testing.29 Even in one study of social networkers, almost half of the participants (47%) were aware of DTC genetic testing, yet only 6% had ever undergone the testing.30,31 Although 23andMe reports that more than 100,000 individuals have accessed their test,32 a 2010 publication, which used the website traffic of three largest companies as a proxy for test uptake, concluded that the demand for genomic profiling was relatively low.33
Data from the Multiplex Initiative34 provide an important look at issues of utilization within the context of a research setting. This project was designed to mirror the approach used by commercial DTC genetic testing companies, but uses web content that focuses on health literacy and risk communication.35,36 Testing was provided at no cost, and those who chose to pursue received education from a research co-ordinator regarding the risks and benefits of testing. Among 1,959 people who were eligible and completed the baseline survey, 612 (31%) visited the website to consider testing. Of those who registered a decision (n = 528), almost half decided against undergoing testing.
Much of the existing literature regarding consumer attitudes and utilization of DTC genetic testing is based on data obtained on so-called early adopters, who generally have confidence in their ability to understand genetics and navigate the Internet and health care system and perceive that results will influence their health behaviors.36,37 Another group that appears particularly interested in DTC genetic testing is of those who are simply interested in “setting the trend,” many of whom proudly blog about their results.38 While relaying optimism about the promises of genomic research, they may express skepticism about the current technology. Yet, other early adopters express belief in the importance of the information to their health, as well as curiosity and fascination with the science.39 Some would-be consumers are more cynical and report that DTC companies are “just trying to sell something” and that this approach is merely a “marketing ploy,” intended to generate revenue for the company without a direct benefit to the consumer.40
Several studies have examined characteristics associated with awareness of and/or interest in online personalized genomic risk assessment. As expected, Internet-savvy individuals are more likely to be aware of testing.36,41 Other predictors of consumer awareness of DTC genetic testing include white race, higher levels of education, greater income, older age, female sex, and numeracy variables.27,42 In a UK study of the public, only 5% indicated a hypothetical interest in testing that costs £259, but 50% expressed interest in a free test.28 Individuals with higher levels of education and those of white race have also been shown to be more willing to pursue testing, with effects influenced by socioeconomic status, affiliation with a health care system, and cost.36,43,44 In the Multiplex Initiative, further predictors of test utilization included motivation to change health behaviors, confidence in genetics knowledge, and perceived severity of the health conditions involved.31




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree