Diabetes and the Healthcare System: Economic and Social Costs
James L. Rosenzweig
In the United States, the medical costs of diabetes are substantial. As the prototype of the chronic disease involving multiple organ systems, diabetes has presented a great challenge to the healthcare system at a time of transition from traditional fee-for-service reimbursement to managed care and capitation. In the United States, a significant proportion of the individuals with diabetes have undiagnosed disease (1). A review of all of the currently accepted performance measures and indicators of quality of care
for patients with diabetes shows that goals for care are not being met in the United States and in the world at large (2,3).
for patients with diabetes shows that goals for care are not being met in the United States and in the world at large (2,3).
In reviewing the management of diabetes mellitus, one must be aware of certain general principles. First of all, diabetes is a complex, chronic disorder. Unlike some other chronic disorders, such as asthma and osteoarthritis, it involves multiple systems. Diabetes is not just an endocrine disease, and control of glycemia, although important, is not the only aim of therapy. Prevention and treatment of the long-term complications of the disease comprise a major part of the overall care of diabetes. Many of the efforts of treatment involve measures that have incremental effects and result in changes in patient behavior that have no perceivable benefit to the patient at the time of intervention but may have significant effects many years later. In accomplishing these goals, the primary caregiver must be able to work in a team with specialists and educators.
PREVALENCE OF DIABETES IN THE UNITED STATES AND IN THE WORLD
Diabetes is one of the most common chronic diseases affecting people in the United States. It is estimated that currently 18.2 million Americans have diabetes, representing 6.3% of the population. This figure includes 13 million individuals with diagnosed diabetes and an estimated 5.3 million people who are currently undiagnosed and untreated. It is estimated that approximately 798,000 new cases of diabetes are diagnosed each year (4). The prevalence of diabetes in the United States increased progressively during the second half of the 20th century, with an approximately 40% increase recorded since the late 1970s. It is clear that the overall burden of diabetes will increase substantially worldwide in the next 20 years.
Several factors have contributed to the increasing burden of diabetes in the United States and worldwide. These include a specific increase in the risk factors for type 2 diabetes, such as increasing obesity (5,6) and lack of adequate physical activity (7), both of which have been shown to increase the likelihood of developing diabetes (8,9). The increased aging of the population worldwide (10) is contributing to the prevalence of a disease associated with aging. In addition, the United States has seen a rapid and proportionately greater growth of those minority populations at the greatest risk for type 2 diabetes and its associated complications (11), as well as of populations throughout the world with increased risk (12). Another factor contributing to the apparent increase in the prevalence of diabetes has been the improvement in surveillance systems for diabetes, which has allowed better assessment of the true burden of diabetes (13).
Many additional new cases probably still go undiagnosed. Data from the National Health Interview Survey indicate that approximately 93% of all people with diabetes have characteristics of type 2 diabetes (14). The prevalence of both diagnosed and undiagnosed diabetes increases progressively with age—from approximately 1.6% of individuals 20 to 39 years of age to approximately 20% of individuals 60 years of age and older. The great majority of individuals older than age 40 years have type 2 diabetes (even a majority of those younger than 40 have type 2 diabetes).
Both diagnosed and undiagnosed diabetes are especially prevalent in minority ethnic populations. When the prevalence is standardized for age and sex, diabetes is 1.6 times more prevalent among non-Hispanic African Americans and 1.9 times more prevalent among Hispanic Americans than among non-Hispanic whites (15). Impaired fasting glucose levels, a condition that is thought to be a precursor to, and to predispose individuals to, type 2 diabetes, is significantly more prevalent in Hispanic-Americans than among non-Hispanic whites and tends to occur at earlier ages in this ethnic population. The incidence and severity of the major secondary complications of diabetes are also greater in these populations than in the general population.
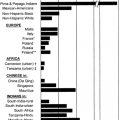
Although the incidence of diabetes will continue to increase substantially in the United States and other developed nations, the rate of increase will be much more rapid in developing countries, which are much less able to handle the financial burden imposed by either conventional or intensive treatment of diabetes. The World Health Organization estimates that the number of people in the world with diabetes may nearly double by the year 2030, approaching 360 million people (16). Enormous increases in diabetes are projected for Southeast Asia, the western Pacific, the eastern Mediterranean, and the Americas. The actual cause of this increasing worldwide epidemic is not entirely clear, but it is likely related to decreased physical activity and changes in diet related to the industrialization in these regions (Fig. 46.1).
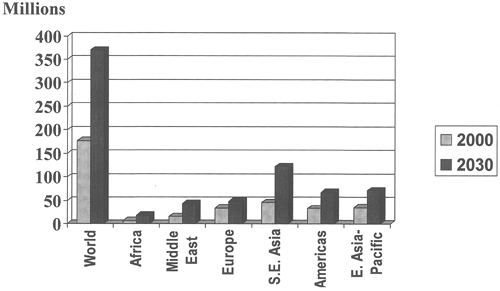 Figure 46.1. Number of persons with diabetes mellitus in the world, by geographic region, in the year 2000, compared with projected estimates by the World Health Organization (WHO) for the year 2030. (Adapted from data from WHO. Available at: http://www.who.int.easyaccess1.lib.cuhk.edu.hk/ncd/dia/databases4.htm. Accessed March 4, 2004.) |
IMPACT OF THE COMPLICATIONS OF DIABETES
Diabetes has a major impact on the health of the U.S. population. It is the leading cause of new blindness, end-stage renal disease (ESRD), and non-trauma-related amputations in adults. Care for diabetes and its complications consumes approximately 15% of
the total healthcare expenditures in the country. That figure is out of proportion to the 6% prevalence of diabetes, reflecting the excess morbidity of and medical care required by patients with diabetes.
the total healthcare expenditures in the country. That figure is out of proportion to the 6% prevalence of diabetes, reflecting the excess morbidity of and medical care required by patients with diabetes.
Diabetes is associated with a substantially increased mortality risk in both men and women. Risk of death is increased threefold to fivefold for persons age 45 to 64 and twofold to threefold for those age 65 to 74. The relative risk declines with advanced age as mortality due to other disease increases. In each age group, women with diabetes have a greater relative mortality risk than do men with diabetes. In the United States, approximately 18% to 20% of those persons who die between the ages of 45 to 74 years have diabetes (17).
People with diabetes are two to four times more likely to experience heart attack or stroke than are people without diabetes (4). People with diabetes younger than age 45 years are 11.5 times more likely to have cardiovascular disease than are people without diabetes. The relative risk of having cardiovascular disease, as well as other comorbidities, which decreases with increasing age, still remains substantially elevated for people with diabetes older than age 65 years (4).
The most common cause of death in people with type 1 or type 2 diabetes is cardiovascular disease, which is the cause of more than 50% of deaths. The acute complications of diabetes, such as ketoacidosis, hyperosmolar coma, and hypoglycemia, are the next most common cause of death, representing about 13%. As individuals with diabetes age, the relative contribution of cardiovascular disease to mortality increases and the contribution of acute complications decreases (18). In the Multiple Risk Factor Intervention Trial, the absolute risk of death related to cardiovascular disease in men with diabetes was substantially increased compared with that in men without diabetes for every age group, ethnic background, and number of additional cardiovascular risk factors (19). The mortality rates for men with diabetes increased steeply as the number of risk factors increased. When patients with diabetes are followed up for 6 years after a myocardial infarction (MI), their mortality risk is increased by 40%, compared with the risk following MI in patients without diabetes (20). The increased risk of post-MI mortality is even more pronounced in women with diabetes than in men with diabetes. Although there has been a substantial decline in mortality due to coronary heart disease in the United States over the past 30 years, this has not been seen in patients with diabetes. In fact, age-adjusted mortality due to heart disease has increased 23% for women with diabetes (21). It is thought that the general decrease in cardiovascular mortality in the general U.S. population is due to a reduction in cardiovascular risk factors and improved methods of treatment of coronary artery disease. These measures have been less effective for patients with diabetes, especially women.
The morbidity associated with the chronic complications of diabetes also represents a significant public health problem. Diabetes is the leading cause of new blindness in adults aged 20 to 74 years (4), accounting for 20% of all new cases of blindness in persons aged 45 to 85 years caused in large part by diabetic retinopathy (22). It is estimated that approximately 90% of these cases can be prevented with improved glycemic control, annual ophthalmologic examinations, and the use of laser treatment if necessary. The prevalence of cataracts is twofold to fourfold higher in patients with type 2 diabetes than in the population without diabetes. Cataracts are a common cause of visual impairment, but not permanent blindness, in older individuals.
Diabetes is also the leading cause of ESRD (4), accounting for 43% of new cases—substantially more than either hypertension or glomerulonephritis. In the United States, the number of new cases of ESRD due to diabetes increased fivefold to sixfold between 1984 and 2001 (23), and the percentage of all cases of ESRD due to diabetes has increased from 28% to 43% (24). A high percentage of these cases could be prevented or substantially delayed with measures aimed at improving glycemic control, more aggressive treatment of hypertension, and early treatment of microalbuminuria with angiotensin-converting enzyme inhibitors.
The risk for amputation in individuals with diabetes is substantially greater than that in people without diabetes; diabetes accounts for greater than 60% of nontraumatic lower-limb amputations in the United States (25). This is due in large part to either peripheral vascular disease or peripheral neuropathy, which occurs in approximately 50% of individuals who have had diabetes 20 years or longer (26). Many of these cases could be prevented by regular foot examinations and treatment, appropriate education in foot self-care, improved control of blood glucose and cholesterol, and smoking cessation.
In the United States, diabetes costs are more than $132 billion annually, with $92 billion related to direct medical costs. In 1992 the cost was $85 billion, and the numbers are increasing each year (27). There is currently no healthcare policy agenda focused on arresting the increase of this chronic disease, which involves 18 million Americans and is the second most expensive disease in the United States. In this country, diabetes is the leading cause of blindness, amputations, ESRD, kidney dialysis, and kidney transplantation (18). The mortality due to type 1 diabetes is 30% higher in the United States than in Europe, and in the United States serious renal disease in all types of diabetes is more than quadruple the rate in Europe (28,29).
GLYCEMIC CONTROL AND MORBIDITY
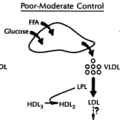
Poor glycemic control is a major reason for the high incidence of microvascular complications involving the eyes, kidneys, and nerves of people with diabetes. The Diabetes Control and Complications Trial (DCCT) clearly demonstrated the benefits of improved glycemic control in reducing both the incidence and the progression of retinopathy and nephropathy in people with type 1 diabetes (30). Substantial clinical and epidemiologic evidence, especially from the United Kingdom Prospective Diabetes Study (31), the Kumamoto Study (32), and the Wisconsin Epidemiological Study (33), indicates that the same principle applies to patients with type 2 diabetes.
The diagnosis of diabetic ketoacidosis involved approximately 100,000 hospitalizations in the United States between 1989 and 1991 and represented almost 5% of all patients with diabetes admitted to hospitals. Most of these admissions are preventable. Severe hypoglycemia is also a major cause of increased emergency department visits and hospitalizations.
DISABILITY, ABSENTEEISM, AND EMPLOYMENT ISSUES ASSOCIATED WITH DIABETES
Disability affects many persons with diabetes in the United States, with estimates ranging from 20% to 50% of the diabetic population. Individuals with diabetes report rates of disability that are substantially higher than those reported by the general U.S. population. Reported activity limitations were two to three times higher among persons with diabetes than among those without diabetes (34). Patients with type 1 diabetes from the Children’s Hospital of Pittsburgh IDDM (insulin-dependent diabetes mellitus) registry were seven times more likely to report work disability than were their nondiabetic siblings.
Impairments for persons with either type 1 or type 2 diabetes increase with age. Disability is more common in minority groups. Disability is proportionately more common in persons with type 2 diabetes than among those with type 1 diabetes (63.5% versus 42.9% report activity limitations), possibly because of the older average age of patients with type 2 diabetes. The major determinant for disability appears to be the presence of the late complications of diabetes.
Impairments for persons with either type 1 or type 2 diabetes increase with age. Disability is more common in minority groups. Disability is proportionately more common in persons with type 2 diabetes than among those with type 1 diabetes (63.5% versus 42.9% report activity limitations), possibly because of the older average age of patients with type 2 diabetes. The major determinant for disability appears to be the presence of the late complications of diabetes.
The effects of disability on the population of persons with diabetes are very extensive. Patients with type 1 diabetes who are disabled have dramatically lower rates of employment than do individuals with diabetes who are not disabled (49% not working versus 12%) and higher rates of absenteeism (13.8 days per year versus 3.0 per year). Disabled individuals with diabetes use healthcare services more frequently, with greater than twice the hospitalization rates and average number of physician visits and a decreased quality of life.
Rates of absenteeism among employees with diabetes are reported as elevated in some studies but not others (35,36,37). Although there is controversy regarding the importance of absenteeism in persons with diabetes, it is clear that significant rates of absenteeism tend to be limited to a small subset of the population of individuals with diabetes—not more than 30%. Most employees with diabetes have normal work attendance records. There is a suggestion that many of the persons who have high rates of absenteeism may be disabled (34). Disabled people with diabetes tend to be absent more frequently and have longer absences than do people with diabetes who are not disabled.
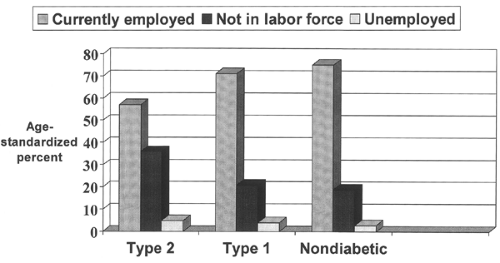
If the impact of disability in persons with diabetes is similar to that in the general population, disability will have significant effects on their employability. A lower proportion of persons with diabetes than persons without diabetes are currently employed, even after adjustments are made for age (Fig. 46.2), but the proportion of those not employed who are disabled is similar to that in the general population (34).
With a higher degree of unemployment and absenteeism, there is concern that persons with diabetes may face discrimination in the workplace. This has been reported in several studies (38,39). The 1990 Americans with Disabilities Act, however, expanded the opportunities of disabled persons with diabetes. This legislation provides standards in employee hiring and allows for work-rule and work-environment changes to meet the needs of individuals with disabilities. It applies to all employers with at least 15 employees, and diabetes is specifically listed as a disability under the Act. The concept that diabetes is in and of itself a disability is a controversial one, but the legislation makes it illegal to discriminate against an individual just because he or she has diabetes.
Nevertheless, there are specific areas of employment where employment of persons with diabetes continues to be restricted. Persons with diabetes taking insulin have been restricted from being airline pilots, drivers in interstate commerce, drivers of local mass transit, and, until recently, air-traffic controllers. The major concern has been the risk of developing hypoglycemia during situations in which alterations in judgment or consciousness could put the pilot or driver in danger or at risk to others. The availability of self-monitoring of blood glucose, along with a greater variety of insulin regimens in recent years, the ability to adjust doses, and count carbohydrates, has ameliorated this problem somewhat, but the DCCT established that intensified insulin treatment can be associated with an increased risk for severe hypoglycemia (30). Since 1984, the American Diabetes Association has taken the position that “Any person with diabetes, whether insulin dependent or non-insulin dependent, should be eligible for any employment for which he/she is otherwise qualified” (40). It is understood, however, that a small minority of patients with diabetes lack or are unable to recognize the warning signs of hypoglycemia and are at greater risk for alterations in mental function that might lead to confusion or alteration in consciousness. Those individuals who have recurrent episodes of severe hypoglycemia should be individually evaluated and, in some situations, be considered for modification of their employment responsibilities.
OTHER SOCIAL ISSUES IN DIABETES
Driving
It has long been claimed that diabetes is associated with an increased risk of automobile accidents and crashes. Three studies, of drivers in California, Oklahoma, and Washington state, identified increased rates of crashes in drivers with diabetes (41,42,43). However, it is possible that the drivers with diabetes in these studies were selected because they had more severe disease. In addition, selection bias may have played a role in some of these studies because the drivers with chronic disease were under review for driving offenses. Another study (44) linked the diagnosis of diabetes to an increased risk of hospitalization for driving-related road trauma, but only among younger drivers.
A study of truck-permit holders and commercial drivers in Quebec found an increased relative risk of crashes for drivers with non-insulin-treated diabetes without complications but not for those treated with insulin or with complications (45). Other studies, however, have failed to find an association between driving accidents and diabetes (46,47,48,49).
A study of truck-permit holders and commercial drivers in Quebec found an increased relative risk of crashes for drivers with non-insulin-treated diabetes without complications but not for those treated with insulin or with complications (45). Other studies, however, have failed to find an association between driving accidents and diabetes (46,47,48,49).
Driving requires complex psychomotor skills, processing of information, and accurate judgment. It is impaired by acute hypoglycemia. Repeated episodes of mild hypoglycemia can be associated with a decreased ability to recognize its symptoms and an increased risk of cognitive impairment. A study of the performance of individuals with diabetes in a driving simulator during induced episodes of mild and moderate hypoglycemia showed that driving performance can be significantly disrupted during relatively mild hypoglycemia, and many individuals fail to take corrective action to treat the hypoglycemia (50). Another study, however, reported that most drivers with hypoglycemia who were cognitively impaired recognized this and reported the perception that they could not drive safely at hypoglycemic levels, but men and middle-aged patients were more likely than women and men under 25 years of age to judge that it was safe for them to drive during hypoglycemia (51). It is important for those with diabetes to have educational reinforcement of safe driving habits and to be encouraged to check glucose levels before driving. Persons whose glucose levels are below 70 mg/dL should be treated before driving. Blood glucose awareness training (BGAT), an 8-week training program that uses behavioral techniques to increase awareness of fluctuations in blood glucose levels, has been associated with fewer and less extreme hypoglycemic events (52) and in follow-up studies has been found to be associated with a reduction in motor vehicle crashes and violations (53).
Because hypoglycemia may be a factor in motor vehicle accidents, most regulatory authorities put restrictions on applicants who have insulin-treated diabetes, whether they have type 1 or type 2 diabetes. However, only individuals with type 1 diabetes appear to be at greater risk for driving mishaps (54). For many years, the U.S. Federal Highway Administration prohibited individuals using insulin from obtaining commercial vehicle driving licenses. However, it had temporarily permitted waivers for some insulin-using drivers (55) but is currently not giving them. Many states are allowing some individuals with insulin-treated diabetes to drive commercial vehicles within state boundaries. The American Diabetes Association has argued for repeal of federal restrictions on commercial drivers with insulin-treated diabetes because of the claim that it is discriminatory and contrary to the Americans with Disabilities Act (56). This remains a complex and contentious issue, in which the justified advocacy for the rights of people with diabetes must be balanced with careful analysis of the risks to public safety.
Travel
The successful management of diabetes requires careful attention to the synchronization of insulin or oral hypoglycemic agents to meals and physical activity. The changes in meals, activity, and time zones that occur with air flight can create unique problems for individuals with diabetes, especially those injecting insulin or using subcutaneous insulin infusion pumps. In addition, travelers to distant countries have to carry syringes and vials of insulin, and the increased security needs of air travel pose special problems. This has become acutely evident since the events of September 11, 2001. Many airlines and countries now require air-travel passengers to carry written documentation of their medical condition and the need to carry syringes, needles, and vials of insulin for injection. Despite these inconveniences, there is no reason why most individuals with diabetes, whether or not they require insulin, should not be able to travel extensively by air across long distances or time zones. Travelers with diabetes should observe the following guidelines, which are modified from the previous edition of this text (57).
The patient should review travel plans with his or her care provider and adjust the timing of meals and insulin dosages to the schedule of travel. How this is accomplished is highly individualized for each patient and travel plan. Good communication between patient and care provider is essential.
The patient should be supplied with a note from the physician outlining the diagnosis, listing the generic and proprietary names of medications, giving the physician’s name and telephone number, and, if possible, listing physicians at the destination who can be consulted in an emergency. Most countries have diabetes associations that can assist international travelers. If the patient carries syringes, lancets, or needles for injection, the note should document the medical necessity for their use.
The patient should carry adequate supplies of medications and materials to treat hypoglycemia. He or she should not depend upon the local availability of these materials. These supplies should never be checked in baggage that is not accessible or that might reach a different destination. On some trips, it may be appropriate to carry extra prescriptions for insulin, syringes, and other essential supplies in case of loss or theft.
It is important for the insulin-requiring patient to have on his or her person easy identification of diabetes in case of emergency. These individuals should wear medical-alert bracelets or necklaces whether or not they are traveling, but it is especially important for them to wear them during travel to distant places or foreign countries.
The patient should conduct frequent glucose monitoring throughout the trip, especially when traveling across time zones and when meal schedules are altered.
The patient should take special precautions to avoid motion sickness or travelers’ diarrhea, both of which may contribute to hypoglycemia, dehydration, or ketoacidosis, and must be especially careful to have the proper immunizations when traveling abroad.
COSTS OF MEDICAL CARE OF DIABETES
The economic costs of diabetes were reported as $11.6 billion in direct medical costs in 1986 for people with type 2 diabetes (58) and $45.2 billion in direct medical costs in 1992 for all people with a diagnosis of diabetes (59). A study comparing the costs of treatment of patients with and without diabetes in 1992 showed that, on average, the annual per capita health expenditures for patients with diabetes were approximately three and a half times the costs for patients without diabetes. From this it could be calculated that the costs of care of patients with diabetes represented almost 15% of total healthcare expenditures in the United States.
The American Diabetes Association published more extensive analyses of the economic costs of diabetes, calculating that direct medical and indirect expenditures attributable to diabetes totaled $98 billion in 1997 (60) and $132 billion in 2002 (61). Direct costs are those associated with hospitalization, ambulatory care, and medication. Indirect costs represent lost productivity due to morbidity and premature mortality. To this must
also be added intangible costs, such as reduced life expectancy and quality of life, for which the assignment of a monetary value is difficult (62,63). The per capita mean costs for persons with diabetes, $13,243 per year, were found to be five times those for persons without diabetes, but this ratio overstates the impact of diabetes because these patients tend to be older, on average (61). The ratio of per capita expenditures between people with and without diabetes was substantially greater for nonwhite patients (4.5:1) than for white patients (3.6:1). Expenditures for outpatient medications were 3.2 times greater for patients with diabetes. The ratio of expenditures between persons with diabetes and persons without diabetes was nearly identical in patients who were younger than 45 years of age (3.2:1) and in those 45 to 64 years of age (3.3:1). This ratio dropped to 1.6:1 for patients 65 years of age and older, as the increased medical costs for nondiabetic elderly patients narrowed the gap.
also be added intangible costs, such as reduced life expectancy and quality of life, for which the assignment of a monetary value is difficult (62,63). The per capita mean costs for persons with diabetes, $13,243 per year, were found to be five times those for persons without diabetes, but this ratio overstates the impact of diabetes because these patients tend to be older, on average (61). The ratio of per capita expenditures between people with and without diabetes was substantially greater for nonwhite patients (4.5:1) than for white patients (3.6:1). Expenditures for outpatient medications were 3.2 times greater for patients with diabetes. The ratio of expenditures between persons with diabetes and persons without diabetes was nearly identical in patients who were younger than 45 years of age (3.2:1) and in those 45 to 64 years of age (3.3:1). This ratio dropped to 1.6:1 for patients 65 years of age and older, as the increased medical costs for nondiabetic elderly patients narrowed the gap.
Direct medical expenditures associated with diabetes totaled $91.8 billion, of which $23.2 billion was related to control of diabetes and blood glucose, $24.6 billion to excess prevalence of the chronic complications of diabetes, and $44.1 billion to excess prevalence of general medical conditions. As expected, the largest proportion of expenditures attributable to diabetes was for inpatient care (43.9%), then for nursing-home care (15.1%), and then for outpatient care (10.9%). Two thirds of the costs for medical care for diabetes are due to care of the elderly. Indirect costs related to diabetes were calculated to be $39.8 billion, of which $7.5 billion was attributed to disability.
The payment for medical services for diabetes is in significant flux. In 1987, 15% of patients were self-paying, whereas in 1991, the number increased to 20%. In 1991, health maintenance organizations (HMOs) became a significant payer group, accounting for 12% of payments for patients with diabetes nationally. This number is now increasing steadily. For some HMOs, diabetes accounts for 15% to 20% of the medical costs, although patients with diabetes account for only 2% of the persons cared for. All patients with diabetes are acutely aware that there is less support for this disease, with regard to education, supplies, and healthcare access.
In 1992, the direct costs of hospitalizations related to diabetes were $37 billion. There has been a decrease in the absolute number of admissions of patients with diabetes—probably approximately 15% during the decade of 1980 to 1990—and a decrease in the primary diagnoses of diabetes by 38% between 1983 and 1990 (64). These data reflect more stringent criteria for hospital admissions. Although the absolute number of admissions of patients with diabetes has decreased, the percentage of diagnoses of diabetes among all discharged patients increased by 27% between 1983 and 1990. These data reflect a relative enrichment of inpatient cases of individuals with diabetes, explaining the increases in hospitalization costs. Diabetes accounted for 8.4% of all hospital admissions during 1989 through 1991, and female patients represented 57% of these admissions. Patients with diabetes are hospitalized 2.4 to 3 times more frequently than are individuals without diabetes. In addition, the duration of their hospital stay is 30% longer on average, exceeding that of patients without diabetes by 1.7 days (65,66). Diseases of the circulatory system were the most frequently listed primary diagnosis: 33% of cases. The proportion of cases in which diabetes was listed as the primary diagnosis declined significantly from 29% in 1980 to 15% in 1990, as treatment of hyperglycemia has shifted from the inpatient to the outpatient setting under managed care in the United States. That trend should be expected to continue. Although hospitalizations for control of glycemia have decreased, the age-adjusted number of hospitalizations per 100 people with diabetes increased 11.7% during 1980 through 1990 (64). It has been estimated that costs associated with the hospitalization of individuals with diabetes in the United States were $37 billion in 1992 and that between 64% and 80% of direct expenditures for people with confirmed diabetes were incurred in the inpatient setting (34,67) (Fig. 46.3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree