Diabetes and Pregnancy
Florence M. Brown
Allison B. Goldfine
Pregnancy may be complicated by diabetes in two distinct forms: gestational and pregestational diabetes. Gestational diabetes typically is diagnosed during the second half of pregnancy and occurs when the β-cell reserve is unable to counterbalance the insulin resistance caused by placental hormones. Although gestational diabetes mellitus usually is asymptomatic, the consequences may be substantial. Fetal complications include stillbirth, macrosomia, increased risk of birth trauma, and neonatal hyperbilirubinemia and/or hypoglycemia. In the United States, the definition of gestational diabetes is based on the results of the 3-hour 100-g oral glucose tolerance test. The interpretation of this test remains controversial, in part because the diagnostic thresholds define future risk of type 2 diabetes rather than fetal outcomes and because laboratory techniques for measuring glucose have changed over time (1). At this time, the American College of Obstetrics and Gynecology (ACOG) accepts two different diagnostic criteria for gestational diabetes (2), one of which is recommended by the American Diabetes Association (ADA) (3) (Table 61.1). To complicate matters, the World Health Organization (WHO) defines gestational diabetes on the basis of the 2-hour 75-g glucose tolerance test (4). The use of multiple diagnostic criteria used in the United States and worldwide underscores the lack of outcome data from randomized clinical trials.
TABLE 61.1. Two Diagnostic Criteria for Gestational Diabetes | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
Diabetes that antedates pregnancy is called pregestational diabetes. Because of differences in the age-specific incidence rates of the two diseases in relation to the childbearing years, most of the patients in the population at the Joslin Clinic with pregestational diabetes have type 1 rather than type 2 diabetes. However, the prevalence of obesity in childhood and adulthood has resulted in a higher prevalence of type 2 diabetes and its onset at younger ages. Many centers are seeing increasing rates of pregestational type 2 diabetes, especially in Hispanic and Native American communities (5). In addition, as women delay childbearing into their fourth and fifth decades, type 2 diabetes is seen during pregnancy with increasing frequency in these women. Often women do not seek medical attention until they become pregnant, so it may rest with the obstetrician to make the diagnosis of diabetes and determine the type of process underlying the diagnosis. The importance of the ADA recommendation to screen the population at high risk for “gestational diabetes” as soon as feasible during pregnancy cannot be overemphasized. In fact, the purpose of early screening in high-risk patients is to identify undiagnosed pregestational type 2 diabetes (6). Features that identify patients at high risk are discussed in the specific section on gestational diabetes.
Pregnancies complicated by pregestational diabetes, either type 1 or type 2, carry additional risks to both the mother and the fetus beyond the effects on fetal growth and development in midpregnancy and late pregnancy that occur with gestational diabetes. Metabolic derangements present at the time of conception and during blastogenesis and organogenesis increase the risk of spontaneous abortions and congenital malformations. Placental vasculopathy in patients with diabetic complications may adversely affect the necessary flow of oxygen and nutrients to the fetus later in pregnancy.
This chapter discusses these two categories of diabetes and pregnancy: gestational diabetes and pregestational diabetes. Discussion of the management of pregestational diabetes focuses on defining and reducing fetal and maternal risks. The pathogenesis, diagnosis, and treatment of gestational diabetes are reviewed. We first will consider the management of women with pregestational diabetes.
PREGESTATIONAL DIABETES
Most women with diabetes hope and expect to be able to bear children, and for only a few of them is pregnancy absolutely contraindicated. Yet there is a broad range of risk to both the mother
and the fetus within this group of women. Concurrent conditions or complications, including retinopathy, nephropathy, neuropathy, hypoglycemia unawareness, hypertension, hypercholesterolemia, maternal age, obesity, and behaviors such as smoking and poor glycemic control, may impact risk. Thus, an assessment of risk should be made for every woman prior to pregnancy, and her individual risk should be discussed with her and with her spouse or partner. All attempts should be made to optimize any modifiable risk factors. To accomplish this, during their reproductive years, all women should be educated by their primary care physicians and/or diabetes healthcare provider on the importance of pregnancy planning to ensure the most successful pregnancy possible. The infants of patients who receive preconception counseling incur fewer congenital malformations and lower healthcare costs (7).
and the fetus within this group of women. Concurrent conditions or complications, including retinopathy, nephropathy, neuropathy, hypoglycemia unawareness, hypertension, hypercholesterolemia, maternal age, obesity, and behaviors such as smoking and poor glycemic control, may impact risk. Thus, an assessment of risk should be made for every woman prior to pregnancy, and her individual risk should be discussed with her and with her spouse or partner. All attempts should be made to optimize any modifiable risk factors. To accomplish this, during their reproductive years, all women should be educated by their primary care physicians and/or diabetes healthcare provider on the importance of pregnancy planning to ensure the most successful pregnancy possible. The infants of patients who receive preconception counseling incur fewer congenital malformations and lower healthcare costs (7).
More than 50 years ago at the Joslin Clinic, Priscilla White devised a classification system to stratify fetal and maternal risk in pregnant women with diabetes (8). The White classification of diabetes during pregnancy was defined by duration of diabetes, age of onset, and concurrent complications. The premise of the White classification was that younger age at diagnosis and longer duration of diabetes increase the risk of microvascular and macrovascular complications and that these complications affect maternal and fetal outcomes. An updated version of the White classification is shown in Table 61.2 (9).
TABLE 61.2. White Classification of Diabetes During Pregnancy (Revised) | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
In current medical practice, almost all women with preexisting diet-controlled diabetes will require insulin during their pregnancies because the goals for fasting and postprandial glucose levels have been lowered since the original classification system was first devised. Thus, the women who would previously have been in “class A,” defined by preexisting diet-controlled diabetes at any age of onset or duration, would now be assigned to class B or below, defined as age of onset at 20 years of age or younger and a duration of less than 10 years. Class C is defined by age of onset at 10 to 19 years of age or duration of 10 to 19 years. Class D includes women with age of onset at less than 10 years of age or duration of 20 years or more or women with a shorter duration of diabetes or with older age of onset who also have background retinopathy or hypertension. Hypertension caused by preeclampsia is not included in class D diabetes. Class F indicates the presence of diabetic nephropathy as defined by proteinuria of greater than 500 mg per day or albuminuria of greater than 300 mg per day. A normal spot urine microalbumin value of less than 20 μg per milligram of creatinine has increased both the sensitivity and the specificity of ruling out diabetic nephropathy and eliminated the need for a baseline 24-hour urine (10). Class R includes women who have proliferative retinopathy or vitreous hemorrhage. Class RF patients meet criteria for both R and F. Class T includes patients with prior renal transplantation. Patients in class H have clinically apparent coronary artery disease.
Studies from the Joslin Clinic (11,12) and other institutions demonstrate very little difference in outcomes in classes B, C, and D, whereas class F diabetes increases the risk of maternal hypertensive complications and fetal intrauterine growth retardation and prematurity (12,13,14,15,16,17,18,19,20,21), with reduced perinatal survival ranging from 89% to 100% but averaging approximately 95% in a series of 10 different studies compiled by Reece and colleagues (21). Microalbuminuria has been shown to be a risk factor for preeclampsia. Of 158 normotensive women with microalbuminuria as defined by urinary excretion of 190 to 499 mg of protein per 24 hours, 31% developed preeclampsia. In patients with hypertension plus microalbuminuria, the incidence of preeclampsia was 50% (22,23,24). A lower-case “f” could be used to distinguish this additional risk in classes B, C, D, and R. For example, a 30-year-old woman who has had diabetes for 8 years and has microalbuminuria would be defined as “Bf.” If this woman also has hypertension, she would be classified as “Df” (although additional studies are needed to evaluate the risk from lower levels of microalbuminuria). Changes in the classification system would require consensus but could provide additional useful clinical information.
Fetal Risk
CONGENITAL MALFORMATIONS AND SPONTANEOUS ABORTIONS
In the 1940s, just 20 years after the discovery of insulin, congenital malformations accounted for about 15% of the 20% to 30% perinatal mortality rate among infants of mothers with diabetes (25). Advances in medical and obstetric care, including home blood glucose monitoring, fetal monitoring to detect fetal distress, and the ability to assess fetal lung maturity, have reduced the incidence of stillbirth and respiratory distress syndrome due
to prematurity. More recently, the perinatal mortality rate for infants of diabetic women remains elevated, at approximately 3%, compared with 1.5% in the general population. However, 50% of perinatal deaths in infants of diabetic women are due to lethal fetal anomalies, which now account for most of the excess perinatal mortality.
to prematurity. More recently, the perinatal mortality rate for infants of diabetic women remains elevated, at approximately 3%, compared with 1.5% in the general population. However, 50% of perinatal deaths in infants of diabetic women are due to lethal fetal anomalies, which now account for most of the excess perinatal mortality.
An increased incidence of congenital malformations in diabetic pregnancies was first suggested in the 1940s by Priscilla White and others (8,18,26). In 1971, Kucera pooled data from 47 reports published between 1945 and 1965 that included different geographic areas and ethnic populations. Of 7,101 infants born to diabetic mothers, 4.8% had congenital malformations compared with 0.65% of 431,764 reported in the general population by WHO (27). More recent studies report incidences of 5% to 9% in clinics treating women with pregestational diabetes (28) as compared with approximately 2% in the general population. Ten malformations have been identified with a higher frequency in infants of diabetic women than in infants of the general population (27) (Table 61.3). The malformations most commonly associated with diabetes, including neural tube, renal, and cardiac defects, occur before the 7th week after conception (29). The finding of multiple associated anomalies suggests a “hit” during blastogenesis that occurs during the first 4 weeks of fetal development. Anomalies during blastogenesis tend to be more severe than those that occur during organogenesis (weeks 4 to 5 after conception) and may increase the risk of spontaneous abortions (30). Thus, interventions to control glycemia and reduce the risk of malformations must begin before conception and continue through the first 7 weeks after conception.
TABLE 61.3. Congenital Malformations in Infants of Diabetic Mothers | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
The suggestion that maternal hyperglycemia was associated with anomalies was made by Leslie et al. (31), who reported three affected infants among a total of five infants of diabetic mothers with poor metabolic control as defined by levels of hemoglobin A1c (HbAlc). Miller et al. (32) reported that for patients with HbA1c levels of 8.5% of less, the incidence of malformations was 3.4% as compared with an incidence of 22.4% in patients with HbA1c levels greater than 8.5%. Although one study suggested a threshold for increased malformations as 12 standard deviations (SD) above the mean (33), a continuum of risk may be present with more modest elevations (34) (Table 61.4). Furthermore, an increased incidence
of spontaneous abortions also has been reported in patients with elevated HbAlc levels (28).
of spontaneous abortions also has been reported in patients with elevated HbAlc levels (28).
TABLE 61.4. Association of Major Malformations in Infants of Mothers with Established Diabetes with Initial Maternal Glycohemoglobin Level | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Because congenital malformations occur early in the first trimester of pregnancy, studies have been focused on improving glycemic control beginning before conception. For ethical reasons, these studies are not randomized, and patients who present for preconception counseling tend to be a self-motivated group. These studies reveal a 2% to 3% risk of malformations in infants of the subjects who receive preconception counseling, compared with a 6% to 10% risk in infants of patients who present for diabetes management after conception (40,41,42,43,44,45,46,47,48). These findings are consistent with the belief that optimization of blood glucose levels before conception can reduce this risk of malformations to a level near that of the general population. Despite the potential benefit of preconception counseling, fewer than 50% of diabetic pregnancies are planned. Women who plan their pregnancies tend to be married, nonsmokers, and white; have higher income and education levels; and report supportive relationships with their healthcare providers. Of note, women whose doctors discourage pregnancy are more likely to have unplanned pregnancies than are women who are encouraged and supported (49).
MACROSOMA AND CESAREAN SECTION
Large-for-gestational age infants are defined as those greater than the 90th percentile weight for gestational age. The incidence of macrosomia has been reported to be 28.5% among infants of patients with type 1 diabetes as compared with 13.1% among infants of controls without diabetes (50). Macrosomic infants experience increased rates of birth trauma, neonatal hypoglycemia, hyperbilirubinemia, respiratory distress, eryth-rocytosis, and hypertrophic cardiomyopathy. A relationship between maternal glycemic control in one or more trimesters of pregnancy and macrosomia has been noted in many (50,51,52,53,54) but not all (55,56) studies. Fasting glucose level appears to have less effect than nonfasting glucose level on macrosomia. Greater maternal weight gain during pregnancy has also been associated with higher infant birth weight. Factors inversely related to infant birth weight include maternal blood pressure higher than 140/90 mm Hg at any time during pregnancy and class F or RF diabetes.
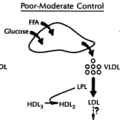
A likely mechanism underlying the relationship between maternal hyperglycemia and infant birth weight was first proposed by Pederson et al. (57) in the 1950s. Maternal transfer of glucose and other substrates across the placenta causes fetal pancreatic hyperplasia and hypersecretion of insulin by fetal β-cells. This results in fetal anabolism and increased fetal adiposity. Hypersecretion of insulin by hyperplastic β-cells after delivery may result in neonatal hypoglycemia (defined as plasma glucose <40 mg/dL) and occurs when the maternal source of glucose to the fetus has been eliminated and relative fetal hyperinsulinemia persists.
NEONATAL HYPOGLYCEMIA
The incidence of neonatal hypoglycemia was approximately 30% in one large study, ranging from 25% in infants of class B mothers to 38% in infants of class D and R mothers (58). Neonates of women who achieve mean preprandial capillary glucose levels of less than 110 mg/dL during the second and third trimesters may have a lower incidence of moderate-to-severe hypoglycemia (<30 mg/dL) than neonates whose mothers have mean capillary glucose levels higher than 110 mg/dL (18.6% vs. 40.6%, respectively) (59). Achieving mean intrapartum glucose levels of less than 100 mg/dL can also decrease the incidence of neonatal hypoglycemia (60).
PREMATURITY AND PERINATAL SURVIVAL
Prematurity occurs with greater frequency in infants of diabetic mothers, especially when diabetes is complicated by renal disease. In most cases, preeclampsia or fetal distress with or without intrauterine growth retardation is present. The incidence of prematurity depends on the definition. Delivery before the 34th week of gestation occurs in approximately 25% of class F or RF pregnancies and before the 37th week of gestation in 50% of pregnancies. Morbidities, including predelivery intrauterine growth retardation and postdelivery respiratory distress syndrome of varying severity, occur in approximately 20% of pregnancies (61).
Variations in the incidence of preeclampsia at different centers arise in part because of the difficulty in distinguishing preeclampsia from the worsening proteinuria and hypertension typical of the late second trimester and the third trimester of pregnancy in patients with chronic diabetic nephropathy. Clinical signs that suggest preeclampsia, such as hemolysis, thrombocytopenia, and transaminase elevations, may not always be present. On the basis of this indistinct clinical picture, the obstetrician is in the difficult position of balancing a poorly defined maternal risk with potential neonatal risks from early delivery.
Most infants of class F and RF pregnancies and many infants of class B through D pregnancies require monitoring in a neonatal intensive care unit. Therefore, these infants should be delivered in tertiary care hospitals where such services are available. Monitoring in neonatal intensive care units is expensive, particularly when infants require lengthy stays, but may be critical to ensure good outcomes for the newborn. Despite the high incidence of short-term morbidity, the overall perinatal survival in class F and RF infants is greater than 95% (21). There are fewer data regarding long-term outcomes for these infants. Pooled data from three separate studies involving 80 children evaluated, on average, at 38 months of age (range, 8 to 78 months) demonstrated psychomotor impairment in 6% (range, 3.7% to 9%) (62).
Maternal Risk
HYPOGLYCEMIA
Hypoglycemia is the most pervasive risk that women with uncomplicated diabetes face during their pregnancies. Severe hypoglycemia occurs in up to 40% of these pregnancies (63). The most severe hypoglycemia occurs during the first half of pregnancy and may be the result of several factors, including emphasis on strict blood glucose control, inconsistent dietary intake associated with morning sickness, and relative insulin sensitivity as compared with that during the second half of pregnancy (64).
Although rats that sustain severe, prolonged hypoglycemia during organogenesis have an increased incidence of congenital malformations, severe hypoglycemia does not seem to be teratogenic in humans. The difference between animal models and humans is not clear but may be related to a dose or duration effect relative to the duration of gestation.
Women whose only symptoms of hypoglycemia are related to neuroglycopenia are at increased risk of severe hypoglycemia. To reduce the risk of severe hypoglycemia, they should assess their blood glucose levels more frequently, including before and after meals, before and after exercise, and before driving. Newer techniques providing continuous glucose sensing may prove to be protective. Hypoglycemia should be treated immediately with 15 g of fast-acting carbohydrate. The finger-stick blood glucose level should be rechecked in 15 minutes and an additional 15 g of carbohydrate given until symptoms have resolved or the blood glucose level is greater than 80 mg/dL. Treating
hypoglycemia with unrestricted carbohydrate may result in rebound hyperglycemia. Family and friends should be ready to assist in the case of severe hypoglycemia. Designated family members and friends should be taught how to use the Glucagon Emergency Kit®.
hypoglycemia with unrestricted carbohydrate may result in rebound hyperglycemia. Family and friends should be ready to assist in the case of severe hypoglycemia. Designated family members and friends should be taught how to use the Glucagon Emergency Kit®.
To improve glycemic control and to ensure the appropriate temporal relationship between caloric ingestion and insulin pharmacokinetics, meals and snack times should be consistent. Many patients use carbohydrate counting in association with short-acting insulin given before meals, with the insulin dose based on a predetermined insulin/carbohydrate ratio and the amount of carbohydrate ingested at a particular meal. This approach allows for flexibility with dietary intake. In the nonpregnant population with diabetes, two insulin analogues, insulin lispro and insulin aspart, have been shown to effectively reduce postprandial hyperglycemia (65,66,67,68,69,70). Given the shortened duration of action of these insulin analogues, they cause less premeal and nocturnal hypoglycemia than does regular human insulin. Data regarding the use of short-acting insulin analogues in pregnancy are limited, but there are no clear adverse effects (71,72). Because pregnancy is a physiologic state associated with exaggerated postmeal hyperglycemia and premeal hypoglycemia, short-acting insulin analogues may be useful therapeutic agents. The new basal insulin analogue insulin glargine, with its long duration of action, has not been studied in pregnancy. The potential effects on the fetus of its binding to the insulin-like growth factor (IGF) receptor with 6.5 times the avidity of human insulin have not been evaluated (73). Insulin lispro has a Food and Drug Administration pregnancy safety rating of B, whereas insulin aspart and insulin glargine have ratings of C.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree