21 Coping with Colorectal Cancer
Introduction
Hearing the words “you have cancer” can be devastating for anyone. The good news about colorectal cancer is that 80% to 90% of those diagnosed at stage I or stage II survive more than 5 years. However, when the cancer is diagnosed at stage III, only about 60% to 70% survive more than 5 years. Unfortunately, when cancer is diagnosed at stage IV, only 8.5% reach the 5-year survival milestone. Thanks to advances in the treatment of advanced colorectal cancer and better management of complications associated with disease and therapy, though, patients with this diagnosis are living longer and better, which creates a realistic sense of hope for the future among this patient population.1
Physical and Psychosocial Aspects of Colorectal Cancer
Colorectal cancer is one of the most common invasive cancers. It is responsible for considerable physical and psychosocial morbidity.2 As part of the study entitled Dimensions of Quality of Life and Psychosocial Variables Most Salient to Colorectal Cancer Patients, a number of focus group participants spoke at length about how they had coped with the experience of colorectal cancer. Some participants said they had made themselves determined to recover and felt that having a positive attitude had been helpful.2 Patients who had coped with previous traumatic events were able to draw on the strength and coping abilities learned earlier through their experience with cancer.2 Participants also found that talking openly about their disease and the treatment they had undergone had been helpful. Learning to live with cancer seems to involve both accepting the situation and finding the inner resources to cope.
Another study, Reducing the Unmet Needs of Patients with Colorectal Cancer: A Feasibility Study of The Pathfinder Volunteer Program, discovered that the most common needs of patients concerned the fear of cancer’s spreading or returning, the worries of others, changes in weight, changes in bowel habits or bowel movements, and bowel problems such as diarrhea, constipation, and pain.3
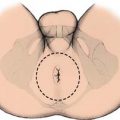
Patients who are facing life with a colostomy or ileostomy after surgery have serious concerns about how to deal with this situation—both physically and emotionally. It is important to remind such patients that their ostomy is allowing them to survive colorectal cancer and to be able to resume their lives.4 Whether a patient needs an ostomy depends on the extent of the surgery. This discussion should occur with the patient before surgery, and the patient should meet with an ostomy nurse before surgery to familiarize him- or herself with the stoma and with living with an ostomy. Furthermore, the patient should become familiar with the appearance and location of the stoma, the various ostomy appliances and supplies, two-piece pouch versus one-piece pouch or pouch plate, how to care for the ostomy, how to clean the stoma as well as the skin, the different skin barriers and seals, how to empty the pouch, how to discard the waste, how to attach and reattach the pouch, how to handle the odor as well as the noises and other sensations, and finally how to resume activities.4 This orientation, for the care of the stoma, may be better handled in the postoperative period once the patient has an ostomy and can really perform the daily care. Patients often find that living with a stoma is easier than they had imagined; reassurance and practical advice are key to a patient’s comfort and acceptance of the situation.
Supportive Strategies
The following tips help patients reduce stress:
 Be assertive rather than aggressive. “Assert” your feelings, opinions, or beliefs rather than becoming angry, combative, or passive.
Be assertive rather than aggressive. “Assert” your feelings, opinions, or beliefs rather than becoming angry, combative, or passive. Two-minute relaxation. Concentrate your thoughts on yourself and your breathing. Take a few deep breaths, exhaling slowly. Mentally scan your body, noticing areas that feel tense or cramped. Loosen up these areas, letting go of as much tension as possible. Rotate your head in a smooth, circular motion once or twice. (If any movement causes pain, stop immediately.) Roll your shoulders forward and backward several times. Relax all your muscles. Recall a pleasant thought for a few seconds. Take another deep breath and exhale slowly. You should now feel relaxed.
Two-minute relaxation. Concentrate your thoughts on yourself and your breathing. Take a few deep breaths, exhaling slowly. Mentally scan your body, noticing areas that feel tense or cramped. Loosen up these areas, letting go of as much tension as possible. Rotate your head in a smooth, circular motion once or twice. (If any movement causes pain, stop immediately.) Roll your shoulders forward and backward several times. Relax all your muscles. Recall a pleasant thought for a few seconds. Take another deep breath and exhale slowly. You should now feel relaxed. Mind relaxation. Close your eyes. Breathe normally through your nose. As you exhale, silently, say to yourself the word “one,” a short word such as “peaceful,” or a short phrase such as “I feel quiet.” Continue for 10 minutes. If your mind wanders, gently remind yourself to think about your breathing and your chosen word or phrase. Let your breathing become slow and steady.
Mind relaxation. Close your eyes. Breathe normally through your nose. As you exhale, silently, say to yourself the word “one,” a short word such as “peaceful,” or a short phrase such as “I feel quiet.” Continue for 10 minutes. If your mind wanders, gently remind yourself to think about your breathing and your chosen word or phrase. Let your breathing become slow and steady. Deep-breathing relaxation. Imagine a spot just below your navel. Breathe into that spot and fill your stomach with air. Let the air fill from the stomach up, then let it out, like deflating a balloon. With every long, slow exhalation, you should feel more relaxed.
Deep-breathing relaxation. Imagine a spot just below your navel. Breathe into that spot and fill your stomach with air. Let the air fill from the stomach up, then let it out, like deflating a balloon. With every long, slow exhalation, you should feel more relaxed.Perspective and Concerns of the Patient
Sexuality-related Issues
A study entitled Colorectal Cancer Patients’ Informational Needs about Sexuality-Related Issues identified and described the importance of providing patients with information about sexuality-related issues during hospitalization.5 Of the 87 patients who completed the structural questionnaire, 71% reported that their disease or its treatment had affected their sexuality. Effects on sexuality were reported by 77% of men and 64% of women with colorectal cancer. In addition, 75% of respondents younger than 40 and 67% of respondents older than 50 complained about the effect that colorectal cancer has had on their sexuality.5 Of the total surveyed, 72% stated that it is necessary to discuss the effect of the disease and its treatment on sexuality during hospitalization,5 and 87% of the patients felt that health care personnel should take the initiative in discussing sexuality-related issues. Only 12% said the initiative should come from the patient.
It is important for health care professionals to provide colorectal cancer patients with an opportunity to discuss issues related to sexuality. The clinician should develop, introduce, and evaluate action models to facilitate open discussion for these sensitive issues.5
Age-related Issues
The PAIS-SR (Psychosocial Adjustment to Illness Scale—Self-Report) measurement tool looked at the patient’s vocational environment, domestic environment, sexual relationship, extended family environment, social environment, and psychological distress for two groups: seniors (older than 65 years) and non-seniors (younger than 65 years).6 Psychosocial adjustment was found to differ by life stage only for “psychological distress.” However, analysis of background factors related to psychosocial adjustment revealed distinct patterns in each life stage. This study suggests that life stage should be considered when attempts are made to improve the psychosocial adjustment among cancer patients.6
Gender-related Issues
According to a study conducted in Israel—Gender and Psychological Distress among Middle- and Older-Aged Colorectal Cancer Patients and Their Spouses: An Unexpected Outcome—male patients reported higher distress scores than their healthy female partners, whereas healthy male spouses had higher distress scores than their sick wives.7 Psychological distress is a common and shared symptom among cancer patients and their spouses, and it persists for years in up to 30% of cancer survivors.7 Psychological interventions involve accurate clinical diagnoses and recognition of and communication of symptomatology by caregivers and patients according to the DSM-IV categorical diagnoses of depression and appropriate pharmacologic recommendations.7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree