Fig. 11.1
Theater organization
Transabdominal Approach
The surgeon works from the patient’s right with the camera assistant on the surgeon’s left side and the first assistant on the patient’s left. To create a more comfortable working position, there should be a monitor on each side of the patient. Pneumoperitoneum is made by a Veress needle insertion on the left upper quadrant, and the abdomen is insufflated with CO2 to a pressure of 12 mmHg. A 12-mm port is introduced next to the umbilicus for a 30°-angled scope (e.g., 3D EndoEye 10-mm videolaparoscope; Olympus KeyMed, Europe), and two 5-mm trocars are introduced through the ileostomy or colostomy sites, being cautious to avoid the inferior epigastric vessels. Finally, a 5-mm trocar is introduced in the right lower abdominal region (Fig. 11.2). Additional trocars can be introduced as needed.
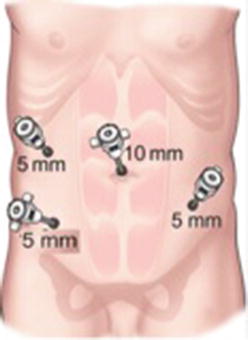
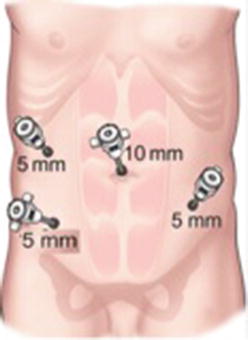
Fig. 11.2
Trocar position in abdominal approach
Firstly, a complete laparoscopic exploration of the abdominal cavity should be performed to identify tumoral implants or occult liver lesions. The patient is placed in Trendelenburg (head down) and right side down positions, and the small bowel is retracted to the upper right quadrant of the abdominal cavity. To perform the procedure, we use a 5-mm LigaSure device (Covidien, Ireland) as hemostatic device and monopolar energy, mainly with the hook. A laparoscopic sigmoidectomy is performed in a medial-to-lateral fashion (Fig. 11.3). The assistant makes a gentle skyward traction of the sigmoid colon, holding the mesentery or an epiploic appendage with a grasping forceps, so the inferior mesenteric vessels are retracted. The surgeon incises the anterior layer of the mesentery, and a blunt dissection is performed between the vessels and the retroperitoneum, until the left ureter is localized well down into the pelvis over the common iliac artery and gonadal vessels, before cutting the mesenteric vessels. The inferior mesenteric artery and the vein are dissected separately. The inferior mesenteric artery is divided 1 cm from its origin with a white 35-mm Endo GIA stapler or with the LigaSure device after applying two clips on the proximal side. The inferior mesenteric vein is found next to the pancreas, and it is divided with the LigaSure device with two clips proximally when necessary. All of the mesosigmoid is released up to the left side of the colon and cephalad to the left colonic artery. Care should be taken to avoid injuries to the mesenteric arcades to guarantee an intact blood supply to the descending colon. Gauze could be used for the hemostasis to protect the ureter and gonadal vessels and as a reference to complete the dissection from the left side. The first assistant draws the sigmoid colon medially to expose the left lateral peritoneal gutter. Toldt’s fascia is incised down to up as far as splenic flexure.
Fig. 11.3
Sigmoidectomy scheme. (a) Development of the medal-to-lateral dissection. Division of the IMA after identification of the ureter and gonadal vessels. (b) Incision of Toldt’s fascia until splenic flexure is mobilized
After sigmoid liberation , we can begin the pelvic dissection, combining our surgery with the one that the transanal team is making from below. With an upward retraction, the surgeon begins to delineate the mesorectum. Thanks to traction-countertraction and the pneumoperitoneum, the proper presacral plane in entered. At this point, the surgeon can bluntly separate the mesorectum (fascia propria of the rectum) from the fascia propria of the sacrum by pushing it anteriorly to the retrorectal space. This way, we can identify the hypogastric nerve trunks and more distally the pelvic nerve plexus avoiding potential injury. After that, the dissection is continued, first along the right side and then along the left, down to the peritoneal reflection in the cul-de-sac through the lateral ligaments. The position of both ureters and hypogastric nerves should be checked at this point and preserved. Meticulous dissection permits identification of the sacral venous plexus. Finally, the peritoneum of the rectovesical pouch or the rectouterine pouch in female patients is incised to expose Denonvilliers’ fascia. By continuing with this dissection plane, the surgical team can rendezvous the team from the transanal approach. This way we can avoid dissection to the levator ani muscle in a narrow pelvis. Once the dissection is completed, the CO2 pressure of the abdominal cavity is reduced to allow repressurization from the CO2 that is coming from the transanal approach. We can complete now the surgery with both approaches at the same time.
Transanal Approach
The perineal team initiates transanal approach , while the abdominal team proceeds with the anterior resection. For this approach, we use a flexible single incision platform (GelPoint Advanced Access Platform, Applied Medical), noting an excellent maneuverability and triangulation of instruments, and a 10-mm 3D flexible endoscope (3D EndoEye 10-mm flexible tip videolaparoscope; Olympus KeyMed, Europe) to minimize the movement inside the rectum. The 3D laparoscopy system allows us to perceive depth within the pelvis. On the other side, the innovative use of GelPoint for transanal access is a perfect alternative, from our point of view, to rigid transanal endoscopic platforms (Atallah), being that the device is universally available and its learning curve is shorter according to its similarity to laparoscopic manipulation.
First, the GelSeal cap (GelPoint Path Transanal Access Platform, Applied Medical, European Union) is prepared and upon it is introduced three 10-mm sleeves making a triangle, with a distance of 2 cm between them. This cap is connected to the CO2 infuser and to a piston valve to exteriorize the smoke. The surgery is begun with a low pressure of 8–10 mmHg that is slowly increased to 12 mmHg in the middle rectum up to 14 mmHg when we perform the rendezvous with the abdominal approach.
The patient is placed in a Lloyd-Davies position with the surgeon and the assistant between the legs. Digital examination is performed to confirm the location of the tumor and the LoneStar Retractor System (CooperSurgical, USA) is applied on the anal verge to expose the anal canal. Depending on the height of the tumor from the anal verge, we can begin the surgery without or with the single port device to develop an intersphincteric resection (ISR) in very low cancers (for tumors located 1–1.5 cm from the anorectal ring) or a higher resection for medium or high rectal tumors in each case. To develop an ISR, the mucosa and the internal sphincter muscle are dissected circumferentially starting at least 1 cm below the distal margin of the tumor and proximately for 1–2 cm until a purse-string suture can be performed to occlude the rectum. This partial or complete excision of internal sphincter extends the distal resection margin and expands the possibility of restorative surgery. To apply the GelPort, the Alexis wound retractor is first introduced and the cap connected on it after removing the LoneStar device. The device is seated just above the anorectal ring, and then it is sutured to the skin to keep in place during the TAMIS-TME procedure. The camera is introduced initially through the 10-mm lower trocar; the left 10 mm is used for an exposure grasper and the right one is used for the dissection instrument (bipolar, monopolar electrocautery, LigaSure, etc.) changing the position as needed, with the help of the pneumorectum to find the correct plane. This device allows us to take the cap out quickly and introduce gauze to clean mucus or bleed as many times as needed. Impregnate the gauze with atropine could help us in the hemostasia for a better visualization.
The first step in the transanal dissection is to place a purse-string 2/0 prolene suture to occlude the proximal lumen of the rectum, at least 1 cm below the lower tumor margin (Fig. 11.4). Small marks are made with monopolar diathermy circumferentially into the mucosa, just distal to the purse string, to delineate the distal resection line not to lose the references. We can now incise all the layers of the rectum radially to obtain a full-thickness transection, and the mesorectum is dissected up to the presacral fascia until identification of the correct plane of dissection (mesorectal plane), using a monopolar cautery hook and bipolar dissecting instruments, in accordance with total mesorectal excision (TME) principles . The dissection is continued sharply down to up within the pelvis along the proper mesorectal fascial and the visceral pelvic fascial plane until an increase of the abdominal pressure is detected, which indicates that rendezvous with the abdominal approach has (Fig. 11.5). The dissection is carried out posteriorly along the presacral avascular plane to mobilize the mesorectum and then anteriorly along the plane posterior to the vagina or prostate until the peritoneal reflection is divided. After this dissection, it is easier to incise the lateral attachments of the colon, alternatively along the right and left sides until the specimen is completely freed, taking care to preserve the lateral pelvic nerve bundles. Once the peritoneal cavity is entered, the CO2 is equalized to 15 mmHg from both insufflation sites. At this moment, we can continue the surgery with two teams simultaneously, using a combined transanal and laparoscopic approach, until the whole specimen is dissected and the specimen is removed transanally (Fig. 11.6). In our experience, it is really helpful to develop the combined surgery with two teams simultaneously, for example, the assistance with retraction that a team is making in its side results in a great advantage for the one who is on the other side; it permits also retraction of a bulking uterus or redundant sigmoid colon and can significantly reduce the operative time.
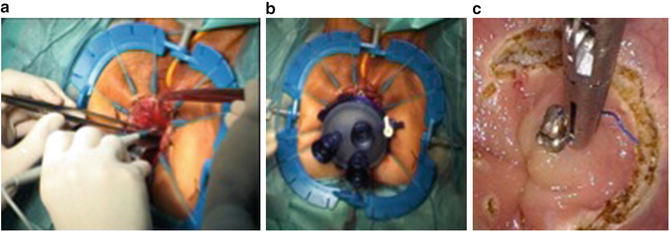
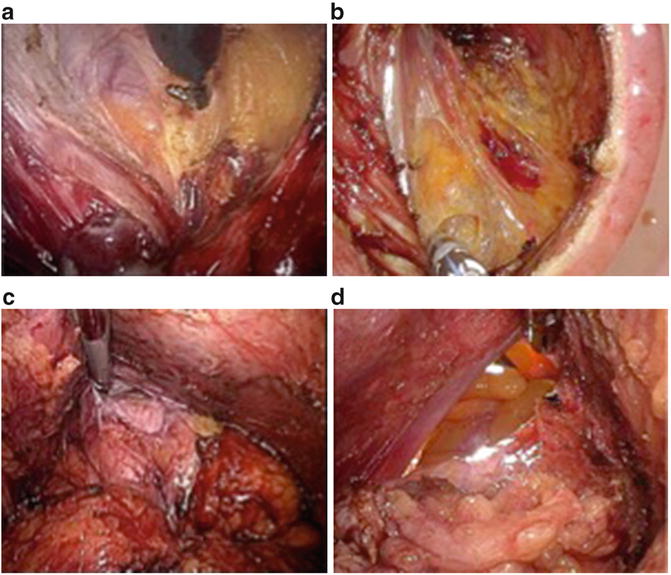

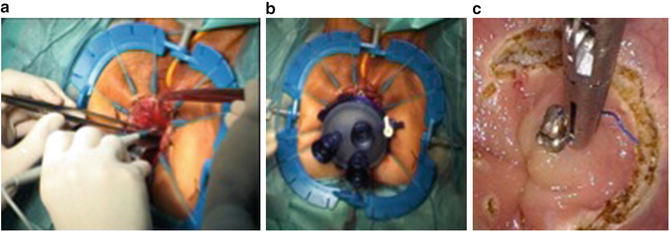
Fig. 11.4
Transrectal dissection. (a) LoneStar Retractor positioned to explore the tumor and begin transanal dissection in ISR. (b) View of GelPoint device to get access to the lumen and develop transanal TMR surgery. (c) Full-thickness rectal transaction below the purse string
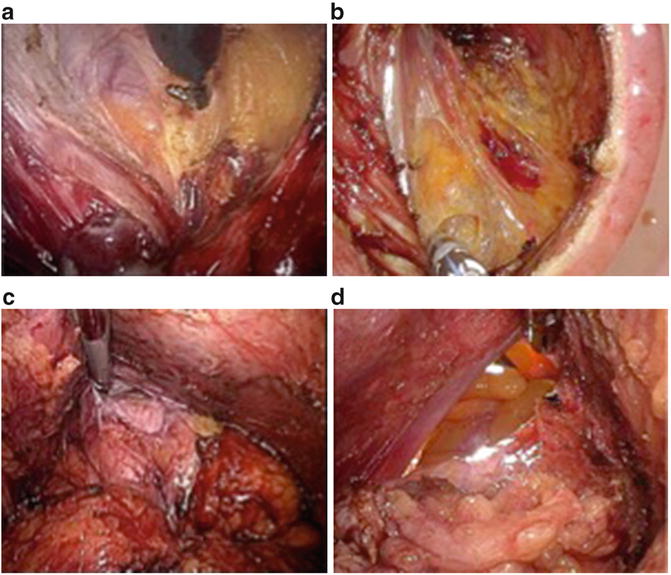
Fig. 11.5
Circumferential view of TME transanal dissection. (a) Posterior view, (b) lateral view, (c) anterior view, (d) peritoneal reflection

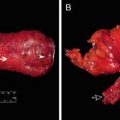
Fig. 11.6
Specimen with intact mesorectum
The most important principle for the management of complications during surgery is anticipation of the possible difficult steps of the surgery in order to prevent these complications. Here we describe some potential complication and how to deal with them:
Presacral hemorrhage and prostatic bleeding. Usually can be stopped with local pressure using a gauze sponge.
Anastomotic bleeding. The transanal approach permits achievement of hemostasis with bipolar cautery or Vicryl sutures.
Trauma to rectal stump during presacral resection. In our experience, with a transanal approach, we minimize the traction over the rectum comparing with conventional laparoscopy or open technique so the potential risk for rectal perforation is reduced. In case this complication does occur, it can be repaired with single sutures or by including this area within the specimen.
Ureteral damage that precise catheterization and primary suture when it is possible or a reimplantation of the ureter in the bladder.
Iliac vessels damage that should be repaired with conversion to open surgery and a prolene suture of 4–5/0.
Anastomotic Technique
Depending on patient and tumor characteristics, we can complete the surgery intra-abdominally or with a Pfannenstiel incision with a mechanical or hand-sewn anastomosis (Fig. 11.7). It is important to note that the target of this procedure is not only to avoid the skin incisions but to improve the quality of the surgery thanks to a better retraction and better visualization of the surrounding structures. With this idea in mind, we describe in the following different techniques for anastomosis.
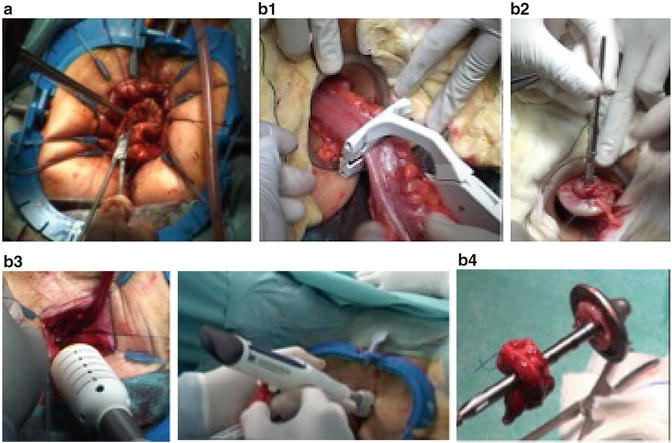
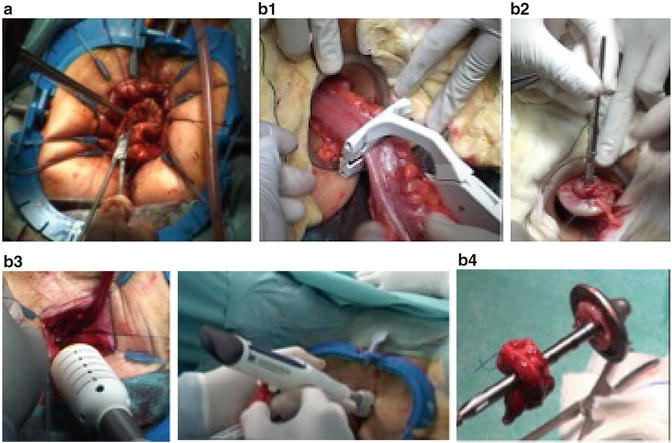
Fig. 11.7




Anastomosis. (a) Hand-sewn coloanal anastomosis, (b) Mechanical anastomosis. (b1) Transanal specimen extraction view with placement of purse-string suture; (b2) anvil positioned; (b3) transanal position of circular stapler (EEA hemorrhoid and prolapse stapler DST series; Covidien, AutoSuture); (b4) rectal donuts
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree