Cardiovascular Syndromes
Inflammatory processes involving the heart are usually classified as pericarditis, myocarditis, or endocarditis, including valvulitis. When all three of these processes are present, the inflammation is called “pancarditis.” Infections of the heart or blood vessels are uncommon in children, in whom they are usually secondary to underlying anatomic defects.
Inflammatory diseases involving the blood vessels can be classified as arteritis or phlebitis. These diseases, too, are rare in children except as a complication of indwelling catheters, as discussed in Chapter 10.
Acute Myocarditis
The clinical findings of acute myocarditis may differ considerably depending upon the age of the patient. In infants, it is often found in association with a severe systemic illness resembling sepsis. Enteroviruses, in particular, may cause infants to suffer a severe and rather acute myocarditis in addition to signs of systemic inflammatory response syndrome. This condition, often called “enteroviral sepsis,” is a serious illness with a high mortality rate. In older children and adolescents, myocarditis is usually best defined by the following findings: presumed acute onset, usually over a week or so; congestive heart failure, conduction abnormalities, or arrhythmias; fever or history of recent fever; and no alternate explanation for the cardiac findings, such as congenital heart disease. Often, the time of onset is difficult to determine in retrospect, so that subacute and chronic myocarditis are diagnosed based on the course rather than the history. The usual clinical findings include gallop rhythm, enlarged heart, and other signs of congestive heart failure (CHF). Distant or soft heart sounds are unusual unless there is severe CHF or pericarditis. Possible electrocardiographic (ECG) abnormalities include low voltage, prolonged conduction time, depressed ST segments and inverted T waves, widened QRS complex, and multifocal extrasystoles.1,2,3,4,5 In older adolescents and adults, the presentation of myocarditis may mimic acute myocardial infarction.6 In one large prospective study of over 672,000 military recruits, 98 (92%) of 107 subjects who developed myocarditis had signs and symptoms suggestive of myocardial infarction.7 In ten (9%) patients, myocarditis caused dilated cardiomyopathy or sudden death.
Classification
There are three general types of myocarditis:
Primary. Here, myocarditis is the chief clinical problem.
Complicating. Examples of this type include myocarditis complicating severe influenza, meningococcemia, or diphtheria.
Causes of Primary Myocarditis
Primary Viral Myocarditis
The enteroviruses, especially coxsackievirus B are the most common causes of primary viral myocarditis.1 The simultaneous occurrence in the community of aseptic meningitis, pleurodynia, or fever without localizing signs supports coxsackievirus B as the cause. Studies utilizing PCR have also shown enteroviruses in heart biopsy samples of patients suffering from myocarditis.
Coxsackievirus A may be an important, but often unproved, cause of primary myocarditis. Unlike coxsackieviruses B, coxsackieviruses A are not readily grown in tissue culture. They do, however, produce skeletal necrosis in mice. Therefore, in the past, mouse inoculation was used to prove a suspected diagnosis of coxsackieviruses A infection. Most laboratories no longer have this capability.
This group of viruses should be suspected when there is herpangina in the community (see Chapter 2).
This group of viruses should be suspected when there is herpangina in the community (see Chapter 2).
Molecular techniques have shown that adenoviruses may be one of the most common causes of myocarditis in childhood. In one study utilizing PCR of myocardial tissue to establish the etiologic diagnosis, adenovirus was even more common than Coxsackie B virus,12 although this has not been the case in other studies.13
Other viruses that have been established as a cause of myocarditis by recovery from the myocardial tissue include poliovirus, influenza, mumps virus, and echovirus. During the 1998–1999 influenza epidemic, a single hospital reported nine cases of myocarditis that developed 4–7 days into a course of typical influenza.14 Echoviruses can be considered less-virulent enterovirus relatives of the coxsackieviruses A and B. A 5-month-old with serologically confirmed roseola who developed a rapidly fatal case of acute myocarditis suggests that HHV-6 can cause myocarditis.15
Acute Rheumatic Fever
This has been the most common cause of clinically apparent myocarditis in childhood and is discussed in detail in the following section. The myocarditis in this disease is often associated with a prolonged PR interval on the ECG and with findings of valvulitis, most frequently manifested by the murmurs of mitral or aortic insufficiency.
Other Infectious Causes
Many other microorganisms or parasites that have the capacity to invade skeletal muscle may also involve cardiac muscle. These include trichinosis, toxoplasmosis, and visceral larval migrans.16 Mycoplasma pneumoniae infection and Lyme disease can also produce myocarditis.17,18 Chlamydia trachomatis is a rare but treatable cause of myocarditis. Several cases have occurred during acute bacterial enteritis due to Shigella sonnei19 and Campylobacter jejuni.20
Hypersensitivity Vasculitis
Idiopathic Primary Myocarditis
In many cases an etiologic diagnosis cannot be established. Perhaps many or most of these cases are caused by a virus, but laboratory evidence does not usually confirm a concurrent infection with a virus known to be capable of producing myocarditis.
Myocarditis Complicating Other Diseases
Myocarditis Complicating Common Childhood Infections
The ECG changes of myocarditis are no more common in children with acute respiratory infections than in a normal control group.23 However, mild myocarditis can complicate measles and mumps.2,24 Rarely, cases associated with varicella25 or with Epstein-Barr virus infection have been reported.26 In these latter cases, direct proof of causation is lacking. Cytomegalovirus has been known to cause myocarditis in immune-suppressed patients after organ transplantation.27
Myocarditis Secondary to Severe Bacterial Infection
In severe bacterial infections, particularly sepsis and meningitis, myocarditis may occur. It is rarely the primary cause of death except in diphtheria, however. In fatal cases of meningococcemia, histologic evidence of myocarditis is frequently found. In nonfatal cases of septicemia with Staphylococcus aureus, clinical evidence of myocarditis may be present. Staphylococcal toxic shock syndrome is occasionally complicated by myocarditis.
Myocarditis Complicating Vasculitis
Juvenile rheumatoid arthritis of systemic onset can include myocarditis (Chapter 10). Dermatomyositis, systemic lupus erythematosus, and scleroderma are rarely complicated by myocarditis. The early stages of Kawasaki disease (Chapter 11) are associated with myocarditis in greater than 50% of cases.28
Human Immunodeficiency Virus Infection (HIV)
Patients with HIV infection often develop myocarditis or cardiomyopathy. It may be caused by the viruses implicated above or may be related to the
underlying disease process. In one autopsy study, histologic evidence of myocarditis was found in 11 (34%) of 32 patients with HIV infection, and borderline myocarditis was seen in another 13 (41%). Adenovirus and CMV were the principal pathogens. No myocarditis was found in 32 age-matched controls (patients with structural heart disease).29 The onset may be insidious, and patients may be asymptomatic or marginally symptomatic for long periods of time. The situation may be further complicated by lymphocytic interstitial pneumonitis, which provides the clinician with another suspect for the gradual loss of cardiovascular vigor. Alternatively, patients with HIV may rapidly develop myocarditis and profound loss of function, especially in late stages of HIV disease or in cases where the myocarditis is due to the mitrochondrial toxicity of nucleoside analogue antiretroviral agents (see Chapter 20).
underlying disease process. In one autopsy study, histologic evidence of myocarditis was found in 11 (34%) of 32 patients with HIV infection, and borderline myocarditis was seen in another 13 (41%). Adenovirus and CMV were the principal pathogens. No myocarditis was found in 32 age-matched controls (patients with structural heart disease).29 The onset may be insidious, and patients may be asymptomatic or marginally symptomatic for long periods of time. The situation may be further complicated by lymphocytic interstitial pneumonitis, which provides the clinician with another suspect for the gradual loss of cardiovascular vigor. Alternatively, patients with HIV may rapidly develop myocarditis and profound loss of function, especially in late stages of HIV disease or in cases where the myocarditis is due to the mitrochondrial toxicity of nucleoside analogue antiretroviral agents (see Chapter 20).
Diagnostic Approach
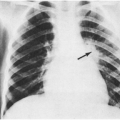
Perhaps the most difficult task is establishing the diagnosis of myocarditis, because signs and symptoms can be nonspecific. In relatively sick children with fever, vomiting, and even mild shock, myocarditis should be on the clinician’s “pessimist list” (see Chapter 1), and a chest x-ray and an ECG should be ordered.
If carried out early in the disease process, cultures (or PCR testing) of the nasopharynx and/or rectum may yield coxsackievirus or adenovirus. Acute and convalescent antibody titers to coxsackieviruses A and B, adenovirus, and EBV may be obtained. Serologic studies should also include antistreptococcal antibody titer measurement, as described in the following section on acute rheumatic fever (ARF). If respiratory symptoms are prominent, and influenza virus is known to be circulating, rapid testing for influenza virus should also be done.30 Because metabolic disturbances may cause similar symptoms, blood glucose and serum calcium levels should be sent. If the patient is highly febrile, blood cultures are reasonable. Complete blood count, erythrocyte sedimentation rate, C-reactive protein, troponin T, LDH, and CPK round out the nonspecific studies. Studies to evaluate heart size and function include the ECG, chest roentgenogram, and echocardiogram. Magnetic resonance imaging (MRI) offers a good picture of acute myocarditis because it can clearly image all parts of the heart, including the apex of the right ventricle.31 Some investigators have used contrast media-enhanced MRI to follow the progress of the disease from focal to diffuse inflammatory changes over the first 2 weeks of illness.32 Endomyocardial biopsy may be helpful in some cases, but its yield in patients who have only dysrhythmias is very low.33
Complications
Arrhythmia or complete heart block can occur in acute myocarditis.34,35 Acute CHF with acute pulmonary edema can occur.
In children, chronic myocardial failure (cardiomyopathy) sometimes occurs without preceding fever or other evidence of an acute infection.34 Cardiomyopathies are usually idiopathic but are occasionally related to infiltrative diseases, toxins, primary muscle or neurologic diseases, nutritional deficiencies, or hypersensitivity reactions. A previous attack of subclinical viral myocarditis has been postulated as a cause of idiopathic cardiomyopathy. In some cases, biopsy of heart muscle will yield the offending virus by PCR testing. In animal models, chronic myocarditis has been linked to ongoing virus replication, but in humans the situation is not entirely clear. Chronic myocarditis is a serious disease with a high mortality rate.34
Treatment
Bed Rest
The emphasis on bed rest, which is recommended for 2 weeks or so, depending on the clinical course, is based in part on the evidence obtained from the experimental model of coxsackievirus B myocarditis in mice, in which exercise worsens disease.36 There is also some evidence in humans that strenuous exercise, in particular, may lead to worsened outcome.37
Digitalization
Digoxin is often helpful, especially in those with signs and symptoms of congestive heart failure, but it should be administered with caution because the inflamed myocardium is exceedingly sensitive to this drug.
Immunosuppressive Agents
Treatment of acute myocarditis with steroids, azathioprine, or other immunosuppressive agents is controversial. In a mouse model of experimental myocarditis, steroids given during the acute phase
of the illness worsened the degree of inflammation and reduced survival.38 Small, retrospective or uncontrolled studies in humans, on the other hand, have suggested some benefit. In one prospective trial 84 patients with dilated cardiomyopathy and increased HLA expression were randomized to receive immunosuppressive therapy or placebo. Short-term improvement was noted, but by 2 years there were no significant differences in the primary end points of death, cardiac transplant, or hospital readmission.39
of the illness worsened the degree of inflammation and reduced survival.38 Small, retrospective or uncontrolled studies in humans, on the other hand, have suggested some benefit. In one prospective trial 84 patients with dilated cardiomyopathy and increased HLA expression were randomized to receive immunosuppressive therapy or placebo. Short-term improvement was noted, but by 2 years there were no significant differences in the primary end points of death, cardiac transplant, or hospital readmission.39
Intravenous Immunoglobulin (IVIG)
Isolated case reports of patients with severe myocarditis who survived after receiving high-dose IVIG in addition to conventional supportive measures have been published.40 The authors of one prospective study gave IVIG in conventional 2 g/kg dosages to twenty-one consecutive children with signs and symptoms of acute myocarditis. No contemporaneous controls were used, but left ventricular function and survival in treated subjects was compared with that of historic controls.41 In this analysis, the group given IVIG was more likely to achieve normal left ventricular function by 1 year after diagnosis (P=0.03). There was a trend toward improved survival. No adverse events of IVIG administration were noted.
Consultation
A cardiologist should be consulted about children with myocarditis because of the complications outlined above. Inotropic agents, diuretics, vasodilators, antiarrhythmia drugs, and regulation of intravascular volume all need careful consideration, usually in an intensive care setting.
Prognosis
Myocarditis has a 1-year case-fatality rate of 15–20%.42 A small but significant percentage of survivors will require cardiac transplantation at a later stage. McCarthy and colleagues have demonstrated that patients who present with fulminant myocarditis have a better long-term prognosis than those who are less severely ill at the time of presentation.42 Of 15 patients with fulminant myocarditis, 14 (93%) were alive without having received a transplant 11 years after presentation as compared to only 59 (45%) of 132 patients with nonfulminant myocarditis. Thus, an aggressive approach, including the use of mechanical circulatory assistance, is warranted in patients with severe fulminant myocarditis.
Acute Rheumatic Fever
Acute rheumatic fever (ARF) is an acute, active disease that should be distinguished from rheumatic heart disease (RHD), which is a permanent valvular deformity usually manifested by a heart murmur. In most cases, the diagnosis of ARF is suspected when a patient has carditis, polyarthritis, or both in temporal proximity to an episode of pharyngitis. Occasionally, chorea is a late sole manifestation of the disease. However, the definition of ARF is complex and is based on a combination of findings called the “Jones criteria,” described later.
In the past, ARF was overdiagnosed, and at present, accurate diagnosis is essential because of the possibility of long-term consequences and the need for antibiotic prophylaxis. Consultation with a cardiologist who will use modern technologic aids is strongly advised.43
Frequency
Once the leading cause of death among children in the United States, the frequency of ARF has been decreasing since the 1940s, when sulfonamide prophylaxis was shown to prevent recurrences in patients with previous rheumatic fever, and penicillin therapy of streptococcal pharyngitis was shown to prevent first attacks.
After 30 years of a steadily decreasing frequency of ARF, in the 1980s there was a resurgence, for reasons that are not entirely clear. Within a period of 5 years, the tone of article titles changed from describing “a vanishing disease” to “the comeback of a disappearing disease.”44,45,46,47,48 Rheumatic heart disease is a frequent cause of death in developing countries, and the decrease in the United States had been attributed to “higher standards of living.”48 The outbreaks in the 1980s and 1990s often occurred in middle-class children, a category of children not usually thought to be at high risk for the disease.44
The resurgence of ARF was localized to several areas and has not been sustained. One theory to explain the fluctuating incidence in the United States points to virulence factors or cofactors that are not yet adequately defined.46,47,48 Certain M-types of GAS are more rheumatogenic than others,
and the M-types that circulate in the United States change over time.49
and the M-types that circulate in the United States change over time.49
In addition, there are probably other factors that determine susceptibility to ARF that are yet to be described. For example, the Aboriginal population of Australia has rates of ARF and RHD that are among the highest in the world. However, Group A streptococcus (GAS) throat colonization is uncommon, and symptomatic Streptococcal pharyngitis is rare.50
Etiology
ARF is a late nonsuppurative sequela of Group A β-hemolytic streptococcal pharyngitis (Chapter 2), often called the preceding or antecedent illness. The pharyngitis is not recognized as an illness by the patient or by the parents in 10–33% of cases, although 50–60% of this subset of patients do remember having had a sore throat.55,56,57 This illness is followed by a latent period ranging from 1 to 5 weeks (average 19 days) before the symptoms of ARF appear.58
About 0.5–2% of children with nonepidemic, untreated exudative pharyngitis and a culture positive for group A streptococci develop ARF.59 The frequency is even less, if the patient group taken as the denominator includes those with less severe or less precisely diagnosed streptococcal infections. This variation in frequency of ARF according to the denominator is an important concept and is clearly demonstrated in the one controlled study done in children59 (Table 18-1). The suggestion is that the development of ARF is likely to follow only infection with rheumatogenic strains of S. pyogenes.60 The types of GAS that usually cause skin infection (impetigo), for example, may precede glomerulonephritis but do not cause ARF. The relatively avirulent phenotypes that are frequently carried in the throats of schoolchildren, also, are not associated with ARF.61 The incidence of ARF following GAS pharyngitis that is treated with appropriate antibiotics is exceedingly low (<0.05%).62
TABLE 18-1. THE FREQUENCY OF ACUTE RHEUMATIC FEVER FOLLOWIG UNTREATED STREPTOCOCCAL PHARYNGITIS* | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||
It is probably a combination of pathogen and host factors that allow this small percentage of patients to develop ARF. Rheumatogenic strains of GAS are rich in M protein and thickly encapsulated with hyaluronic acid.63 No specific host factors that predispose to the development of ARF have been clearly identified; however, in some studies HLA-DR7 was found with greater frequency in patients with ARF than in controls.64 In developing countries, malnutrition and failure to thrive have been associated with the development of ARF.65
Both the arthritis and the carditis are thought to be autoimmune. The arthritis is mediated by antigen-antibody complexes, but the carditis is caused by cytotoxic T lymphocytes.66 There may be antigens in GAS that are closely related to heart antigens, which causes the host to produce heart-directed
immune responses. The current medical practice is to treat all episodes of streptococcal pharyngitis in order to prevent ARF (Chapter 2).
immune responses. The current medical practice is to treat all episodes of streptococcal pharyngitis in order to prevent ARF (Chapter 2).
Age Factors
First attacks of rheumatic fever usually occur in children over 5 years of age and in young adults, presumably because previous streptococcal infections are necessary to sensitize the patient. First attacks of ARF rarely occur in patients less than 3 years of age.67
Jones Criteria
As modified in 1992,68 the Jones criteria are applicable only to the initial attack of ARF. Although designed as an epidemiologic tool, the Jones criteria are now often used as a guide in diagnosis. The criteria require either two major manifestations or one major and two minor manifestations plus, in either case, evidence of a preceding streptococcal infection (Box 18-1).69 The diagnosis should always state the major manifestations present (e.g., ARF with carditis and polyarthritis).69
Major Manifestations
The usual major manifestations are polyarthritis (not polyarthralgia) and carditis (defined by murmurs, pericarditis, cardiomegaly, or CHF). The three murmurs that suggest rheumatic carditis are described in the Jones Criteria:69
BOX 18-1 Jones Criteria (Modified) for the Diagnosis of ARF
| Two major OR One major and two minor manifestations PLUS Preceding Group A streptococcal infection (recent scarlet fever, throat culture positive for Group A streptococci, high or rising antistreptococcal antibody titer [ASO or anti-DNAse B]) |
| Major Manifestations Polyarthritis Carditis Chorea Erythema marginatum Subcutaneous nodules |
| Minor Manifestations Arthralgia Prolonged PR interval Fever Elevated erythrocyte sedimentation rate or C-reactive protein |
Apical systolic murmur. This long, blowing, high-pitched murmur is best heard at the apex and has variable loudness. It is transmitted toward the axilla and suggests mitral regurgitation.
Apical mid-diastolic (Carey-Coombs) murmur. This is best heard with the bell of the stethoscope with the patient lying on the left side with the breath held in expiration. This murmur is a result of rapid ventricular filling, as in left ventricular dilatation and may occur in conditions other than acute carditis.
Basal diastolic murmur. This high-pitched blowing murmur is best heard with the diaphragm of the stethoscope at the right upper or the left midsternal border with the patient sitting and leaning forward with the breath held after deep expiration. It suggests aortic regurgitation.
Many patients who do not have physical examination evidence of carditis have been shown to have mitral insufficiency and/or aortic insufficiency by Doppler echocardiography.70 The importance of this so-called silent carditis, and whether echocardiographic evidence of carditis should be counted as fulfilling the diagnostic criteria for ARF, are topics of some debate.66,70 Most of these clinically silent valvular abnormalities are transient but a small percentage may persist.70,71
The arthritis of ARF is a characteristic migratory polyarthritis. It typically involves the large joints (knees, ankles, wrists, and elbows) and is manifested by swelling, warmth, and exquisite tenderness. Joint inflammation usually lasts for only a few days and then another joint becomes affected. The arthritis is so responsive to aspirin and other NSAIDS that a trial of these agents is sometimes used as a “diagnostic test.” The arthritis of ARF is not deforming, and unlike the cardiac manifestations, there are no long-term sequelae of joint involvement. This led to the description of ARF as a disease that “licks the joints but bites the heart.”72
The other major manifestations are much less common and consist of chorea,73 subcutaneous nodules, and erythema marginatum. The nodules are better seen than felt. They may occur with other diseases, and it has been recommended by some observers that they be dropped from the list of major manifestations of ARF.74 Erythema marginatum is an evanescent, usually rapidly migratory,
nonpruritic pink rash with serpiginous raised borders. The rash resembles smoke rings, expanding and leaving a clearing center. Adequate pictures of this rash are rare, and it is seldom seen now.75 In the largest of the 1980s outbreaks (107 confirmed cases), no erythema marginatum was seen.76 Sydenham’s chorea (St. Vitus’ dance) is more common than subcutaneous nodules or erythema marginatum, occurring in 15–20% of patients. It has a longer latent period than arthritis or carditis, with symptoms starting several months after an episode of GAS pharyngitis. Importantly, it may occur as the sole manifestation of the disease (“pure chorea”). In one study of 22 children with pure chorea, however, 14 (63%) were demonstrated to have valvulitis by echocardiography, the long-term consequences of which are unclear.77 Chorea is manifested by erratic jerky movements of the extremities and facial grimacing, as well as emotional lability. Physical findings suggestive of chorea include spooning (hyperextension of the fingers and wrists when the arms are held in extension) and tongue fasciculations.
nonpruritic pink rash with serpiginous raised borders. The rash resembles smoke rings, expanding and leaving a clearing center. Adequate pictures of this rash are rare, and it is seldom seen now.75 In the largest of the 1980s outbreaks (107 confirmed cases), no erythema marginatum was seen.76 Sydenham’s chorea (St. Vitus’ dance) is more common than subcutaneous nodules or erythema marginatum, occurring in 15–20% of patients. It has a longer latent period than arthritis or carditis, with symptoms starting several months after an episode of GAS pharyngitis. Importantly, it may occur as the sole manifestation of the disease (“pure chorea”). In one study of 22 children with pure chorea, however, 14 (63%) were demonstrated to have valvulitis by echocardiography, the long-term consequences of which are unclear.77 Chorea is manifested by erratic jerky movements of the extremities and facial grimacing, as well as emotional lability. Physical findings suggestive of chorea include spooning (hyperextension of the fingers and wrists when the arms are held in extension) and tongue fasciculations.
Minor Manifestations
The minor manifestations are arthralgia (not counted as a minor manifestation if polyarthritis is used as a major), fever in excess of 100.4°F (38.0°C) rectally, abnormal acute-phase reactants (erythrocyte sedimentation rate or C-reactive protein), and conduction changes detected by ECG, primarily prolonged PR interval (not counted as a minor manifestation if carditis is used as a major). Rarely, ARF presents as Stokes-Adams attacks, complete heart block,78 or torsade de pointes.79
Differential Diagnosis
The differential diagnosis of ARF includes a number of other diagnoses or syndromes, which are discussed in the sections on myocarditis and pericarditis, rheumatoid arthritis, septic arthritis, gonococcal arthritis, reactive arthritis (Chapter 16), and infective endocarditis. Common errors include making the diagnosis of ARF when a single joint is involved, when an innocent murmur is present, when a nonspecific rash (especially an urticarial or an erythema multiforme rash) is erroneously called erythema marginatum, and when other causes of chorea are overlooked.80
Acute rheumatic fever can produce a tenosynovitis resembling that of disseminated gonococcemia, and the two diseases may be very difficult to distinguish.81
Misdiagnosis of ARF is not unusual, and in one series, only 68 of 100 children originally thought to have ARF had illnesses clearly meeting the modified Jones criteria.82 Of the 32 with illnesses not meeting these criteria, 14 had a different diagnosis (such as congenital heart disease, rheumatoid arthritis, and undiagnosed fever), 9 had suspected ARF without heart disease, and 9 had evidence of RHD (mitral or aortic valvular disease) without a history of ARF.82 The difficulties of “delabeling” patients with an uncertain diagnosis make it essential that all patients with suspected ARF receive diagnostic evaluations that are as thorough as possible at the time of the initial episode. If the diagnosis of ARF is made, the reasoning behind the diagnosis should be carefully documented in the medical record.
The flip side of the coin is that ARF can sometimes be a difficult diagnosis to establish. The arthritis may be short-lived83 or even monoarticular.84 The carditis may be silent. Physicians who see patients in areas where ARF is uncommon may not have ever seen a case. Therefore, the thought that a particular set of symptoms may represent ARF may never enter the mind. When one case occurs, the physician should be on the lookout for others, because it tends to come in groups as a rheumatogenic strain is passed around the community.
Post-Streptococcal Reactive Arthritis (PSRA)
This entity has now been well-described and can be distinguished from the arthritis of ARF on the basis of several characteristics.85
The latent period from the onset of GAS pharyngitis to onset of arthritis is shorter in PSRA than in ARF and is usually less than 2 weeks. In contrast to the arthritis of ARF, PSRA is nonmigratory and affects small joints as well as large ones. The arthritis of ARF usually lasts only a few weeks and is very responsive to salicylates. PSRA has a more protracted course and responds poorly to aspirin and other NSAIDs. A small subset of children (about 6%) who seemingly have PSRA will develop carditis over time, primarily manifested by subtle mitral valve disease.86,87 Finally, patients with PSRA do not meet the modified Jones Criteria for the diagnosis of ARF. Criteria for the diagnosis of PSRA have recently been proposed and include the distinguishing features discussed previously.88
A survey of rheumatologists and infectious disease
specialists in Canada showed that there is no consensus on the utility or the duration of prophylactic therapy for PSRA.89 The American Heart Association recommends that patients with PSRA receive penicillin prophylaxis for 1 year. If, at that time, there is no evidence of carditis, prophylaxis is discontinued.90 This seems to be a reasonable approach and one that we have adopted, although others have argued for longer prophylaxis in these patients.91 Longer prophylaxis (i.e., as for ARF) should probably be prescribed for patients with post-streptococcal arthritis whose symptoms are more typical of ARF than PRSA (e.g., large joints, migratory, responsive to aspirin).
specialists in Canada showed that there is no consensus on the utility or the duration of prophylactic therapy for PSRA.89 The American Heart Association recommends that patients with PSRA receive penicillin prophylaxis for 1 year. If, at that time, there is no evidence of carditis, prophylaxis is discontinued.90 This seems to be a reasonable approach and one that we have adopted, although others have argued for longer prophylaxis in these patients.91 Longer prophylaxis (i.e., as for ARF) should probably be prescribed for patients with post-streptococcal arthritis whose symptoms are more typical of ARF than PRSA (e.g., large joints, migratory, responsive to aspirin).
Chorea
Sydenham’s chorea (the chorea of ARF) can be mimicked by chorea induced by oral contraceptives, that following infectious mononucleosis,92,93 that associated with systemic lupus erythematosis,94 or paroxysmal choreoathetosis, which is usually familial.95 Chorea may also be a complication of surgery for congenital heart disease.96
Treatment
Bed Rest
As soon as the diagnosis is made, bed rest is advisable for a minimum of 2–3 weeks until it is certain no carditis is present. If carditis is present, bed rest for 1 to 3 months may be advisable. When the heart rate and sedimentation rate are normal and the arthritis is over, gradual resumption of normal activities can begin. Every patient in whom this diagnosis is considered should be thoroughly evaluated, ideally by a cardiologist, in terms of the Jones criteria, before being put on bed rest.
Salicylates and Other Nonsteroidal Anti-Inflammatory Agents
Patients with arthritis or carditis in the absence of cardiomegaly are generally treated with anti-inflammatory agents. Aspirin at a starting dose of 100 mg/kg per day for 1 week up to 10 g per day and then 60 mg/kg per day for 3–4 weeks has been used. In the past, salicylate levels of 15–25 mg/dL were sought and levels followed. Most experts now believe that obtaining levels is unnecessary unless signs of salicylate toxicity occur or the therapy is not producing the desired result.
Because of the small risk of Reye syndrome in patients on aspirin therapy, alternate anti-inflammatory therapy has been evaluated. A small, noncomparative group of patients had rapid resolution of fever and arthritis on naproxen sodium.99
For patients with frank cardiomyopathy or signs of congestive heart failure, corticosteroids are generally used in place of aspirin (see later).
Whenever applicable, vaccination against influenza and varicella should be considered for patients who may require long-term aspirin therapy.
Treatment of Congestive Heart Failure
Corticosteroids
The value of steroids for treatment of acute rheumatic carditis is controversial.103 Most authorities agree that steroids are not necessary if there are no significant murmurs and that these agents probably should be used in very ill patients with severe carditis manifested by congestive failure or pericarditis. In patients with significant murmurs but without congestive failure, the superiority of steroid therapy to aspirin therapy is not proved. If steroids are used, the recommended dose is 2 mg/kg per day of prednisone, up to 60 mg/day, until clinical improvement (about 2–4 weeks), followed by a gradual taper in the dose (reduce by 5 mg every 2–3 days). Salicylates are begun at the time the prednisone taper is started and continued for 6–12 weeks.80 No adequately randomized and controlled trials have demonstrated the utility of corticosteroids in the treatment of ARF.
Intravenous Immunoglobulin (IVIG)
Because of potent immunomodulatory effects, it has been thought by some physicians that IVIG might be beneficial in severe cases of ARF. Very small case series in which IVIG was thought to have been beneficial have appeared.104 However, a randomized,
prospective, double-blinded trial in 59 patients with ARF showed no detectable benefit from the administration of large, repeated dosages of IVIG.105
prospective, double-blinded trial in 59 patients with ARF showed no detectable benefit from the administration of large, repeated dosages of IVIG.105
Prognosis
A rebound (transient worsening) occurs in about one-third of children within 4 weeks of stopping steroid or salicylate therapy and presumably represents the original suppressed disease.106 Recurrences tend to have the same manifestations as the original attack.107 Death caused directly by ARF is now rare in the United States.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree