Abstract
This chapter reviews the most commonly used imaging modalities in the screening and diagnosis of breast diseases. Topics discussed include characteristic benign and malignant imaging findings on mammography, breast ultrasound, and breast magnetic resonance imaging, as well as common image-guided breast interventional procedures, including core needle biopsy and preoperative needle localization.
Keywords
screening mammography, diagnostic mammography, breast ultrasound, breast magnetic resonance imaging, core needle biopsy, preoperative needle localization
Breast imaging includes all of the imaging modalities used to detect and diagnose breast diseases. The most common breast imaging modality is mammography, which is a radiographic examination of the breasts. Since the first report on mammography in the United States in the 1930s, mammography has undergone striking technological improvements and quality assurance procedures that have improved its sensitivity and accuracy ( Fig. 26.1 ). In addition, standardized reporting has been developed to improve the communication of mammography results and management recommendations.
The two major types of mammography are screening mammography and diagnostic mammography. Screening mammography is used to detect unexpected breast cancer in asymptomatic women. Diagnostic mammography is used to evaluate the breasts of patients with symptoms, such as a palpable lump or nipple discharge. Mammography is also used to guide interventional procedures of the breast, including core needle biopsy (CNB) and preoperative needle localization.
Digital mammography is currently the standard screening and diagnostic mammography examination ; approximately 95% of mammography units are now digital. Digital mammography stores images electronically in a digital format and displays them on computers. The main advantages of digital mammography are unlimited contrast resolution, computer-aided diagnosis (CAD), and teleradiology. CAD refers to supplementary computer scanning of images to assist in detection of potential imaging abnormalities. Teleradiology enables digital images to be transmitted electronically, with the potential to increase access to mammograms.
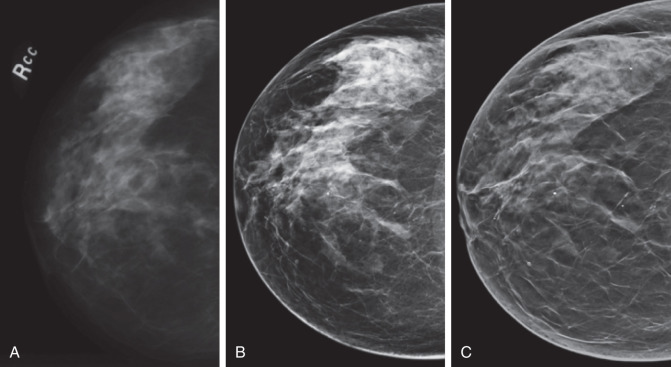
Digital breast tomosynthesis (DBT) or three-dimensional (3D) mammography is an emerging digital technology that consists of a series of low dose x-rays taken at different angles in a small arc over the breast. DBT can either be performed with or without conventional two-dimensional (2D) digital mammography. When performed without conventional 2D digital mammography, 2D digital views are computer-generated from source images using software. Studies have shown that DBT decreases false-positive interpretation rates and increases cancer detection rates compared with conventional 2D digital mammography.
Breast ultrasound, the use of sonar energy to produce an image of the breast, is used for both screening and diagnostic purposes, as well as for guiding interventional procedures.
Magnetic resonance imaging (MRI) is used for screening high-risk women and for diagnostic indications, such as evaluation of extent of disease in newly diagnosed breast cancer.
Other imaging modalities used for the diagnosis of breast diseases include ductography.
Mammography
Screening Mammography
Breast cancer is the most common noncutaneous malignancy in women. Each year, approximately 231,840 new cases of breast cancer are diagnosed, and about 40,290 women die of this disease in the United States. Large randomized controlled screening trials have shown that screening mammography reduces breast cancer mortality by approximately 30%.
For screening mammography, two views of each breast are performed: mediolateral oblique (MLO) and craniocaudal (CC). The MLO view includes the greatest amount of breast tissue and is the only view that includes all of the upper outer quadrant and axillary tail ( Figs. 26.2 and 26.3 ). The CC view provides better image detail because greater compression of the breast is usually possible, as well as better visualization of the inner aspect of the breast ( Figs. 26.4 and 26.5 ).


The importance of proper breast compression during mammography cannot be overemphasized. The compression device helps to (1) immobilize the breast and prevent motion unsharpness, (2) separate overlapping tissues that might obscure underlying lesions, (3) bring the breast closer to the image detector and reduce geometric blur, and (4) decrease the radiation dose by decreasing breast thickness.
Diagnostic Mammography
For diagnostic mammography, imaging is supervised directly by the interpreting physician and is tailored to the specific indication for the examination, such as abnormal screening mammography, findings that require additional imaging, or abnormal clinical findings, including a palpable lump.
In the setting of abnormal screening mammography findings, the diagnostic examination may begin with repeating the view(s) on which the original abnormal finding was visualized to see if it persists. A number of additional mammographic views may be performed to help define the nature of and localize an abnormal finding, the most common of which are the 90-degree lateral and spot compression views.
The 90-degree lateral view is used along with the MLO and CC views to triangulate the location of an abnormal finding. Spot compression involves the use of a small compression device placed directly over the abnormal finding and can be performed in any projection ( Fig. 26.6 ). The smaller compression device allows for greater compression over the area of interest and displaces overlying tissues that could obscure the finding. Magnification technique is often combined with spot compression to better resolve both the margins of masses as well as the character of calcifications. Other projections include rolled, cleavage, and axillary tail views. All of these mammographic views may be performed with either 2D or 3D tomosynthesis technology. Ultrasound targeted to the area of interest is commonly used in conjunction with diagnostic mammography ( Fig. 26.6E ).
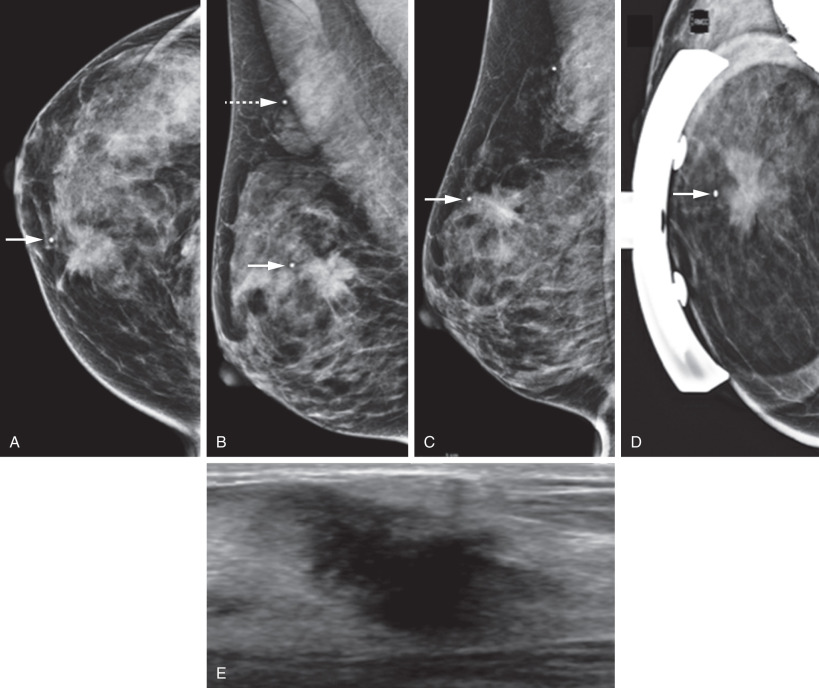
For abnormal clinical findings such as a palpable lump felt on physical examination by a referring health care provider, communication of its location in terms of laterality, clock face, and distance from the nipple is helpful for directing the diagnostic examination, especially when it is not felt by the patient. The mammography technologist palpates the indicated area of palpable abnormality and places a radio-opaque lead marker directly over the area before image acquisition, such that the lead marker indicates the area of concern (see Fig. 26.6 ). Similarly, the sonographer or physician supervising the examination palpates the indicated area of palpable abnormality before scanning to enable a directed ultrasound examination in the area of concern.
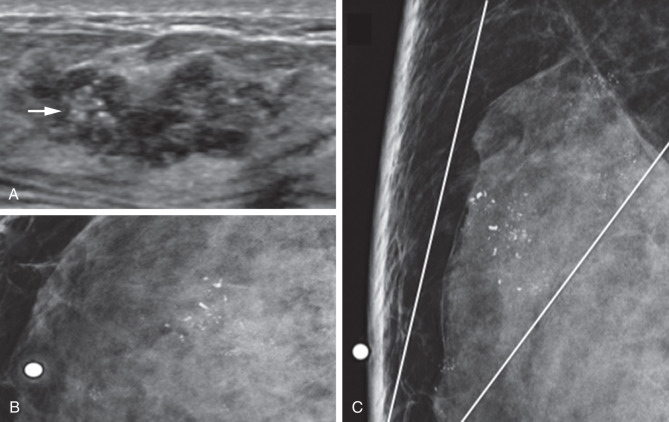
For women 30 years of age and older, both mammography and ultrasound should be performed to better define the nature of the palpable abnormality, to detect concurrent lesions in the ipsilateral or contralateral breast that are clinically occult, and to identify any associated calcifications indicating an intraductal component of a palpable cancer ( Fig. 26.7 ). For women under 30 years of age, ultrasound is the first choice examination, with mammography reserved for cases in which calcifications are suspected ( Fig. 26.8 ).

Standardized Terminology for Mammography Reports
The American College of Radiology (ACR) Breast Imaging Reporting and Data System (BI-RADS) was devised to facilitate uniform reporting of mammographic findings, assessments, and recommendations from different imaging centers, as well as to facilitate outcome monitoring. Every mammography report is required by the federal Mammography Quality Standards Act to include an assessment category, such that management recommendations are as clear as possible. There are seven assessment categories, each associated with a management recommendation. BI-RADS category 0 (incomplete) identifies cases in which additional imaging and/or comparison to prior imaging is needed before a final assessment can be made. Once additional imaging or comparison to prior imaging is accomplished, such cases are assigned one of the six “Final Assessment” categories. Screening mammograms are assigned BI-RADS categories 0, 1, or 2, whereas diagnostic mammograms are assigned BI-RADS categories 1 through 6.
Normal Mammographic Findings
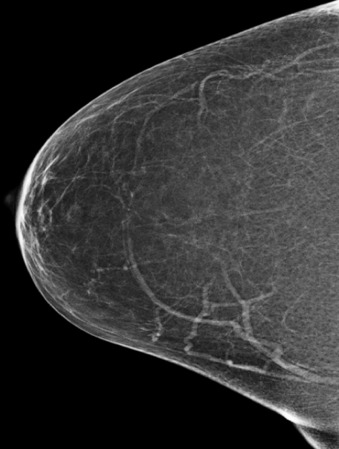
The normal breast has a wide range of mammographic appearances in terms of size, shape, density, and fibroglandular tissue pattern. Breast density ranges from almost entirely fatty to extremely dense ( Fig. 26.9 ). In the BI-RADS lexicon, breast density is characterized by four categories, with progressively decreased mammographic sensitivity for cancer detection: (1) almost entirely fatty, (2) scattered areas of fibroglandular density, (3) heterogeneously dense, and (4) extremely dense. Because breast cancers are radio-opaque (white on mammograms), they are more easily seen in an almost entirely fatty breast (black on mammograms) compared with an extremely dense breast (white on mammograms).
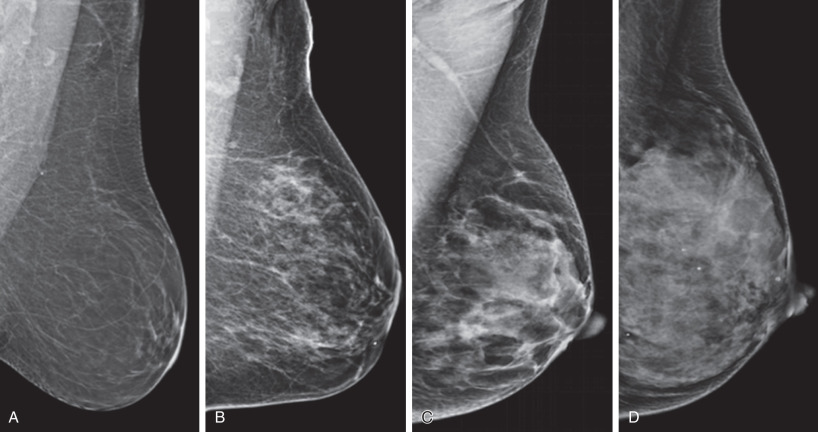
Increased breast density can be seen in younger women, during pregnancy and lactation ( Fig. 26.10 ), and in response to exogenous hormone therapy due to a higher proportion of fibroglandular tissue.
Abnormal Mammographic Findings
Masses and calcifications are among the most common abnormal findings on mammograms. The BI-RADS lexicon used to describe masses and calcifications indicate their likelihood of malignancy. Other abnormal findings include architectural distortions, asymmetries, and axillary lymphadenopathy.
Masses
A mass is a 3D, space-occupying lesion with convex outward borders that is seen on at least two mammographic projections.
Masses are described by their shape, margin, and density in the BI-RADS lexicon. Shapes are round (spherical), oval (elliptical), or irregular (neither round nor oval) ( Fig. 26.11 ). Round and oval shapes favor benignity.

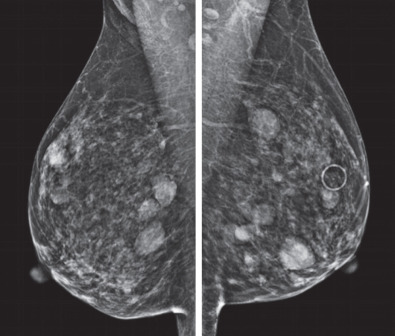
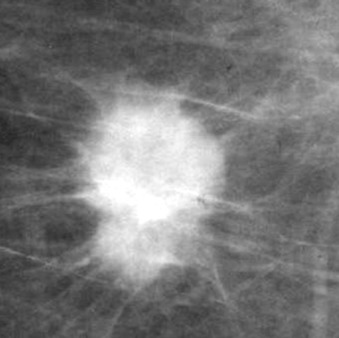
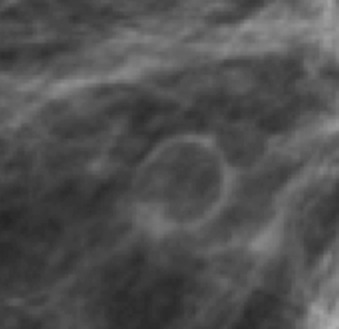
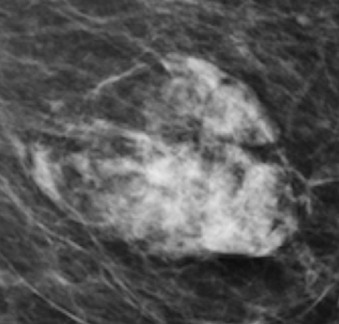
Margins are circumscribed (with a clear demarcation from surrounding tissue), obscured (hidden by superimposed or adjacent fibroglandular tissue), microlobulated (characterized by short cycle undulations), indistinct (without a clear demarcation from surrounding tissue), or spiculated (characterized by radiating lines) ( Fig. 26.12 ). Circumscribed margins favor benignity. The presence of multiple, bilateral, round or oval, circumscribed masses ( Fig. 26.13 ) is especially suggestive of benign masses such as multiple cysts, fibroadenomas, or intramammary lymph nodes. Microlobulated, indistinct, and spiculated margins ( Fig. 26.14 ) are suspicious for malignancy.

Density is determined relative to normal fibroglandular tissue and is described as fat-containing, low, equal, or high. Fat-containing or low densities favor benignity, whereas high density is suspicious for malignancy. Examples of fat-containing masses include oil cysts ( Fig. 26.15 ), lipomas, galactoceles, and hamartomas ( Fig. 26.16 ).
Masses may be associated with other findings, such as microcalcifications (see Fig. 26.7 ), skin thickening, skin retraction, and nipple retraction, which increase suspicion for malignancy.
Benign Masses.
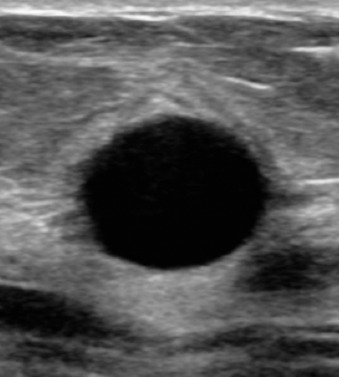
Cysts are solitary or multiple, round or oval, circumscribed, usually equal density masses. They are most commonly seen in women between the ages of 40 and 50 years. Cysts tend to vary in size over serial examinations, usually decreasing in size over time. Targeted ultrasound can be performed in the area of mammographic mass to confirm the presence of a simple cyst ( Fig. 26.17 ). If the characteristic features of a simple cyst are present, diagnostic accuracy approaches 100%, thus obviating the need for aspiration or biopsy.
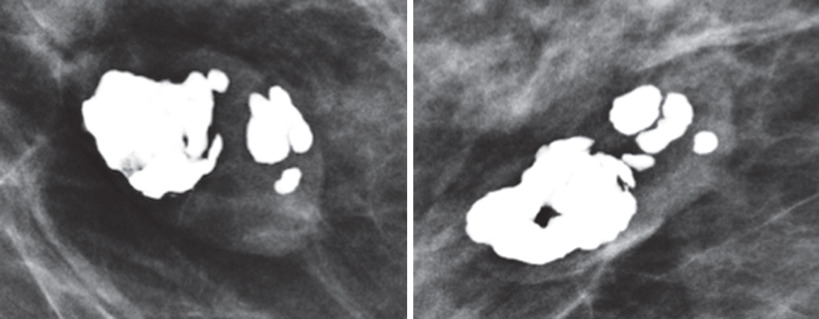
Fibroadenomas are common masses, appearing as solitary or multiple, round or oval, circumscribed masses. As they involute over time, they tend to develop characteristic coarse, “popcorn-like” calcifications ( Fig. 26.18 ).
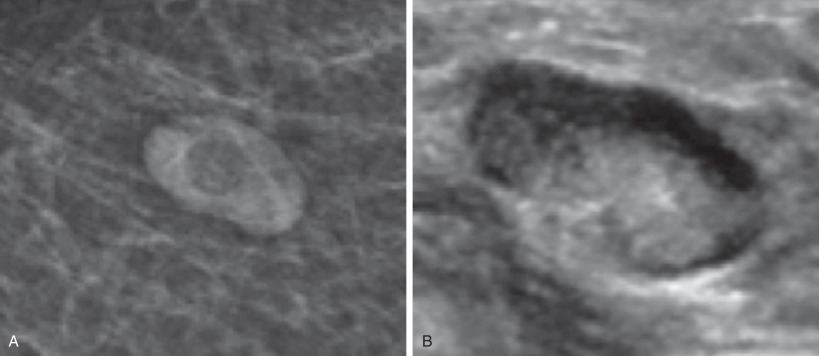
Intramammary lymph nodes are normal anatomic structures that are most commonly found in the upper outer quadrant of the breast. They have a characteristic reniform shape and central radiolucency representing the fatty hilum. Correlative ultrasound may show central echogenicity representing the fatty hilum and a hilar blood vessel ( Fig. 26.19 ).
Oil cysts result from fat necrosis in the setting of prior trauma or surgery and typically appear as round or oval, fat-containing masses with or without a thin rim of calcification ( Fig. 26.20 ).
Lipomas may be detected incidentally on mammography or present as palpable abnormalities, appearing as oval, fat-containing masses with a thin fibrous capsule in the subcutaneous soft tissue. Lipomas are more difficult to distinguish in a fatty breast; however, their capsules are more easily seen on DBT.
Galactoceles are usually seen in lactating women and are thought to originate from clogged ducts, consisting of milk products including fat. They are variable in density depending on proportion of internal fat contents. When present, a fat-fluid level is pathognomonic.
Hamartomas are round or oval masses with fibrous capsules, variable in density depending on proportions of internal fat and soft tissue components (see Fig. 26.16 ).
Malignant Masses.
The most common malignant breast mass is invasive breast cancer. Several subtypes of invasive cancer exist, with varying prognoses.
Invasive Ductal Carcinoma of No Special Type.
The most common subtype, invasive ductal carcinoma (IDC) of no special type (NST), usually presents as an irregular mass with indistinct or spiculated margins and high density. Occasionally, this subtype appears to have partially circumscribed margins, which on further diagnostic imaging with spot compression views may reveal partially indistinct margins. Approximately 40% of cases are associated with suspicious microcalcifications, such as fine pleomorphic calcifications (see Fig. 26.7 ).
Invasive Lobular Carcinoma.
Invasive lobular carcinoma (ILC) may appear as an irregular, equal density mass with indistinct or spiculated margins (see Fig. 26.6 ), as a subtle architectural distortion, or as an asymmetry. However, ILC is often occult on mammography. Because ILC may be unappreciable on clinical palpation or mammography, even when relatively large in size, it may be difficult to diagnose.
Tubular Carcinoma.
Tubular carcinomas grow relatively slowly and are usually small when detected on mammography. Other than a characteristically small size, they have the mammographic features of IDC of NST: irregular shape, spiculated margins, and high density ( Fig. 26.21 ). They have an excellent prognosis relative to IDC of NST.
Medullary Carcinoma.
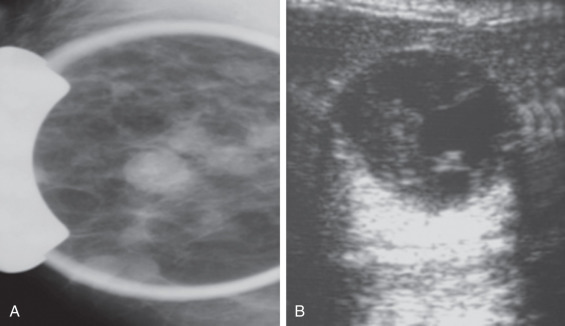
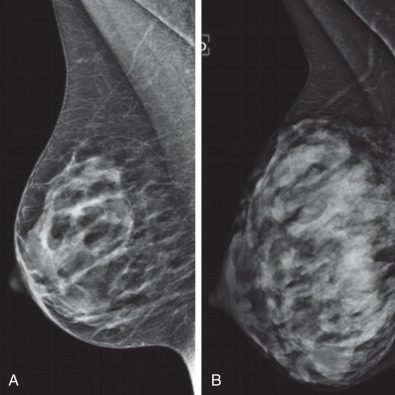
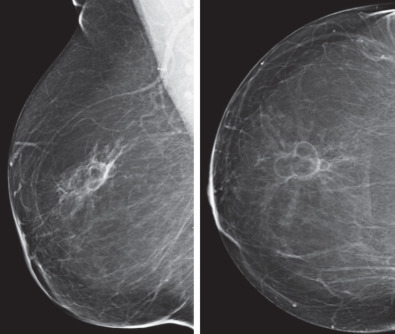
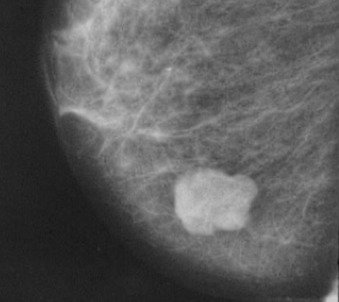
Medullary carcinomas are more commonly seen in younger women and tend to have benign mammographic features of oval shape and circumscribed margins ( Fig. 26.22 ). Correlative ultrasound may show internal fluid contents. This combination of apparently benign features may result in delayed diagnosis.
Mucinous Carcinoma (Colloid Carcinoma).
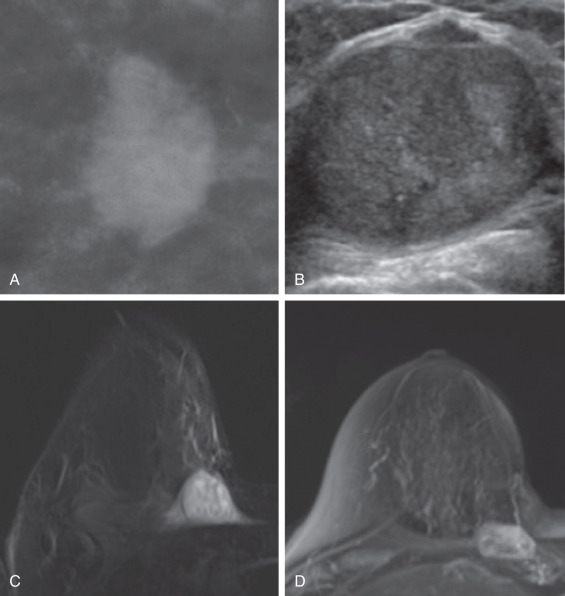
Mucinous carcinomas are more commonly seen in older women and tend to have benign imaging features, including oval shape and circumscribed margins on mammogram, posterior acoustic enhancement on ultrasound and T2 hyperintensity on MRI ( Fig. 26.23 ). Mucinous carcinomas usually coexist with other subtypes. Although uncommon, pure mucinous carcinomas have a better prognosis compared with IDC of NST.
Intracystic Papillary Carcinoma/Invasive Papillary Carcinoma.
Adenocarcinoma arising from a cyst wall is uncommon and is usually of the papillary subtype. The conglomerate mass is often large and circumscribed on mammography with both cystic and solid components on ultrasound. The solid portions may project centrally from the cyst wall ( Fig. 26.24 ). If the tumor is entirely intracystic, the cancer is noninvasive, and prognosis is excellent. Invasive papillary carcinoma appears similar to intracystic papillary carcinoma on imaging but shows invasion on histology, with worse prognosis compared with intracystic papillary carcinoma.