PROLACTIN-SECRETING ADENOMAS
Prolactin-secreting adenomas comprise the largest group of pituitary tumors. The behavior and relatively benign clinical manifestations of small prolactinomas distinguish them from the tumors that produce Cushing disease and acromegaly, two distinct endocrinopathies that are usually life-threatening. Whereas the clinical necessity of treating patients with either Cushing disease or acromegaly is clear, the indications for immediate treatment of patients harboring a small prolactin-secreting adenoma are less so (see Chap. 13 and Chap. 21).
CLINICAL MANIFESTATIONS
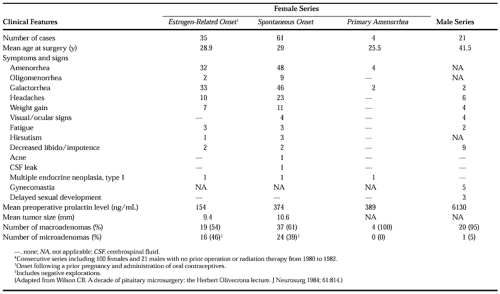
In 1954, Forbes and colleagues9 first reported that pituitary adenomas could produce amenorrhea and galactorrhea. However, only recently have these tumors been recognized as a frequent cause of secondary amenorrhea and galactorrhea. Among the women in one surgical series5 (Table 23-2), 80% presented with secondary amenorrhea or galactorrhea, 10% with primary amenorrhea, and 10% with either oligomenorrhea and galactorrhea, secondary amenorrhea without galactorrhea, or secondary amenorrhea only. Among men, prolactinomas usually remain undetected until a large tumor produces either significant panhypopituitarism or compression and invasion of the parasellar structures. In the previously mentioned series,5 only seven men had symptomatic hyperprolactinemia without abnormalities of additional pituitary hormones; either thyroid, adrenal, or gonadotropic function, or a combination of the three, was usually impaired as well. Many of these patients experience impotence early in the course of their disease, but this problem often does not lead to an investigation of the prolactin level. The author can recall seeing in his practice a 35-year-old man who received electroshock therapy for 10 years as “treatment” for his impotence; the patient presented with a prolactin level of >1000 ng/mL.
Hyperprolactinemia secondary to a pituitary adenoma has extragonadal manifestations. Recent rapid weight gain is a frequent complaint of hyperprolactinemic women and occurs with a frequency that suggests a correlation. Correction of hyperprolactinemia, either by surgery or by medical therapy, has been followed by impressive weight loss in many cases, despite no apparent change in dietary habits. Equally impressive is the incidence of emotional lability, which is often dramatically reversed after the correction of hyperprolactinemia. Studies demonstrate that the estrogen deficiency secondary to hyperprolactinemia causes bone demineralization, sometimes producing secondary complications.10
LABORATORY EVALUATION
The first step in the evaluation of a patient with suspected hyperprolactinemia is to obtain a fasting serum prolactin level. The administration of thyrotropin-releasing hormone (TRH) does not consistently distinguish between functional hyperpro-lactinemia and actual prolactinoma11 (see Chap. 13). In men whose basal prolactin values exceed 100 ng/mL, establishing a prolactinoma as the cause of the hyperprolactinemia is not difficult. In women, hyperprolactinemia (>200 ng/mL) almost invariably indicates a tumor. Caution must be exercised, because prolactin levels as high as 662 ng/mL have been observed to occur in nonsecreting tumors, presumably due to pronounced pressure on the pituitary stalk, which inhibits the transport of prolactin inhibitory factor to the pituitary gland.12
In the author’s experience, the diagnosis of prolactinoma in a patient with basal prolactin levels <200 ng/mL requires radiographic identification of an intrasellar lesion. Even with unequivocal radiographic demonstration of such a lesion, transsphenoidal exploration occasionally reveals either a diffusely enlarged anterior lobe (pituitary hyperplasia) or a nonneoplastic intrasellar cyst, most often involving the pars intermedia. In such cases, the presence of the radiographic abnormality is usually not related to the elevated prolactin level. Patients must, therefore, be cautioned about this possibility, particularly now that the resolution of MRI imaging has become so good.
SURGICAL DECISION MAKING
As experience with the use of the dopamine agonists (i.e., bromocriptine and cabergoline) accumulates, the indications for surgery in patients with prolactin-secreting tumors are changing. Currently, most patients who are referred for surgery have large and invasive tumors. Although a role exists for surgery in these patients, they are rarely cured by an operation
alone, and usually require supplemental drug therapy, radiation therapy, or both.
alone, and usually require supplemental drug therapy, radiation therapy, or both.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree