Surveillance for Sexually Transmitted Diseases
1 Centers for Disease Control and Prevention, Atlanta, GA, USA
2 San Francisco Department of Public Health, San Francisco, CA, USA
Introduction
When describing the challenges clinicians face when treating syphilis, which is a notoriously complex and challenging infection, Sir William Osler, the father of modern medicine, said “Know syphilis in all its manifestations and relations, and all other things clinical will be added unto you” [1]. Often shortened to “to know syphilis is to know medicine,” this phrase could be adapted to capture the complexities and challenges of sexually transmitted disease (STD) surveillance, data collection, and interpretation: “To know STD surveillance is to know public health surveillance.”
This chapter begins with a brief review of the importance and objectives of STD surveillance; then describes STD surveillance strategies, including case-based, sentinel, opportunistic surveillance, as well as population-based surveys; and concludes with case studies highlighting examples of challenging STD surveillance issues, as well as practical uses of STD surveillance data to improve and evaluate STD prevention and control activities.
Health Impact of STDs
STDs are important health conditions from both public health and societal perspectives for a variety of reasons, including excessive burden, health disparities, and the high costs associated with STD-related sequelae and their role in facilitating HIV transmission and acquisition. Among all nationally notifiable diseases, three STDs (chlamydia, gonorrhea, and syphilis) are consistently in the top five most commonly reported diseases annually. These three STDs made up more than 86% of all reported diseases in the United States in 2010 [2]. In 2011, over 1.4 million cases of chlamydial infection were reported, the largest number of cases of any disease ever reported to the Centers for Disease Control and Prevention (CDC) [3]. The true burden of STDs is likely to be higher, as most infections are asymptomatic [4] and are never diagnosed or reported. A synthesis of a variety of data sources estimated that in 2008 there were over 100 million prevalent STDs and nearly 20 million incident STDs in the United States [5].
Several populations are disproportionately affected by STDs, and the magnitude of the inequities are some of the largest known in public health [6]. Adolescents are significantly more impacted by STDs [3,5]. Nationally, 72% of all reported STDs are among persons aged 15–24 years [3], and it is estimated that 1 in 4 females aged 14–19 has an STD [7]. More striking are the racial and ethnic disparities. In 2011, the rates of chlamydia, gonorrhea, and primary and secondary syphilis among African-Americans were, respectively, 7.5, 16.9, and 6.7 times the rates among whites [3]. Additionally, men who have sex with men (MSM) are disproportionately infected with STDs. Although population estimates of the number of at-risk MSM are often sparse [8], several analyses have shown risk ratios above 100 for the associations between being an MSM and having syphilis or HIV [9,10].
In addition to acute symptoms such as genital ulcers, dysuria (painful urination), and discharge, STDs can cause long-term adverse reproductive sequelae including ectopic pregnancy and infertility [11]. Some STDs, such as syphilis, can cause organ damage and lead to cardiovascular and neurological problems and even death. Many STDs can be transmitted congenitally during pregnancy or birth. In 2008, over 400,000 neonatal deaths and stillbirths were associated with syphilis worldwide [12]. Additionally, untreated chlamydia and gonorrhea can cause ophthalmia neonatorum in newborns, which can result in blindness [13]. The medical and societal costs for STDs are high. An analysis in 2005 of the annual costs for STDs among adolescents in the state of California exceeded $1 billion in direct medical costs alone [14]. One estimate in 2008 put national costs at $15.6 billion [15].
Finally, STDs can increase both susceptibility to and transmissibility of HIV [16]. Inflammation of genital tissue or ulcerations caused by STDs can increase the probability of infection if exposed to HIV. Additionally, HIV-infected persons who contract an STD may be more likely to transmit HIV to their partners because of increased HIV viral loads as a result of the concurrent infections. Although a wide range of observational studies have demonstrated an association between a bacterial STD and risk of subsequent HIV transmission or acquisition [17,18], causality is difficult to demonstrate because of lack of randomized trials. Despite this, prevention and treatment of STDs remain an important part of HIV control efforts.
Objectives of STD Surveillance
Objectives of STD surveillance include assessing incidence and prevalence of infections and STD-related sequelae and monitoring STD-related health services use. Surveillance data are used to describe trends in emerging and existing epidemics, to identify outbreaks and high-risk populations, and to monitor the impact of control programs. STD surveillance can be used to target health services (e.g., identify populations not accessing or delaying care) as well as to understand the impact of health policies. Additionally surveillance data are often used to develop evidence-based screening and treatment recommendations [19,20] and to monitor adherence to screening recommendations [21–23]. Surveillance can also monitor sentinel health events. For example, any infant born to a mother with syphilis who was not treated within 30 days of delivery should be reported as a congenital syphilis case. Although the infant may not actually have the disease, a case report is a marker of an important gap in service delivery, namely inadequate prenatal care.
Challenges in STD Surveillance
A significant challenge in STD surveillance is that the term “STD” encompasses a variety of infections. Currently, there are over 35 pathogens that can be transmitted sexually, including bacteria (e.g., Chlamydia trachomatis), protozoa (e.g., Trichomonas vaginalis), viruses (e.g., herpes simplex virus [HSV]), and ectoparasites (e.g., Sarcoptes scabiei) [11]. Some infections can cause clinical syndromes shortly after exposure, whereas others result in no symptoms or have a long latency period. Some STDs can be easily diagnosed using self-collected swabs, while others require a sample of blood or a physical examination by a clinician. Consequently, no one particular surveillance strategy works for all STDs.
The pathophysiology of STDs presents additional challenges. The asymptomatic nature of most STDs limits inferences from case-based surveillance, since in order to be counted in this system an infection must be diagnosed and reported. Additionally, many infections never result in disease. For example, an estimated 90% of human papillomavirus (HPV) infections resolve on their own without sequelae [24]. As such, simply counting infections may not be appropriate, and sequelae must also be monitored. Finally, some STDs are curable (e.g., gonorrhea), and persons can be infected multiple times in their lifetime, with each diagnosis indicating a new infection. For viral STDs with no cure (e.g., HSV-2), serologic markers can monitor lifetime exposure but may not represent incident disease.
Many populations at highest risk for STDs are “hidden” and may not be fully captured in surveillance data. For example, MSM may be reluctant to disclose their sexual behavior to clinicians and public health workers for fear of judgment or discrimination. This may prevent MSM from seeking appropriate sexual health care (e.g., they may not be screened for rectal infections) or may result in their being inaccurately categorized as heterosexual on case reports. Sex workers may also fear that disclosure would result in criminal prosecution. Transgender persons may not identify as such, or the surveillance system may only accept gender values of male, female, or missing. Effectively using surveillance data in decision making is contingent on understanding what information may be missing because of systemic bias in the available data.
Strategies for STD Surveillance
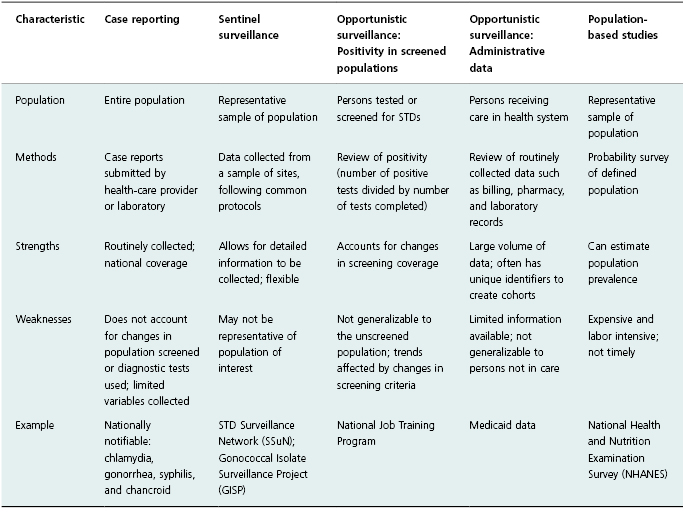
Strategies for STD surveillance include case reporting; sentinel surveillance; opportunistic surveillance, including use of administrative data and positivity in screened populations; and population-based studies (Table 12.1). Given the multiple challenges in effectively conducting surveillance for STDs, the choice of strategy depends on the type of STD and the population of interest. Inference involving multiple data sources and strategies is often necessary to monitor prevalence and incidence of STDs.
Table 12.1 Examples of strategies for STD surveillance.
Case Reporting
State and local laws require that healthcare providers or laboratories report communicable diseases to public health authorities by submitting case reports. Four STDs are reportable conditions in all 50 states: chlamydia, gonorrhea, syphilis, and chancroid [3]. Other STDs, such as neonatal herpes, nongonococcal urethritis, and Lymphogranuloma venereum, are reportable in some states [25]. Although case reporting has relied historically on individual providers to complete case reports, the use of laboratory reporting for reportable STDs has increased in the last 2 decades. Increasing use of electronic lab reports has likely improved the timeliness and completeness of case reporting [26]. Additionally expanded use of electronic medical records to aid in reporting should further improve the completeness of case reports, particularly for common STDs such as chlamydia [27].
Case reports are the foundation of STD surveillance as they are collected annually, national in scope, available in every locality, and provide important (albeit limited) demographic information such as age, race/ethnicity, and gender to monitor epidemiologic trends and describe health inequities. Additionally, case-report data can aid in prevention and control programs. For example, when a syphilis infection is reported, public health staff contacts the patient to ensure treatment is completed (secondary prevention) and to provide risk reduction counselling and partner notification services (primary and secondary prevention).
Case reports can also provide a sampling frame for probability samples for sentinel surveillance. For example, in the STD Surveillance Network (SSuN) a sample of all reported cases of gonorrhea in participating areas are selected for enhanced interviews to collect additional information not reported on the case-report form, such as sexual behaviors and clinical signs and symptoms [28].
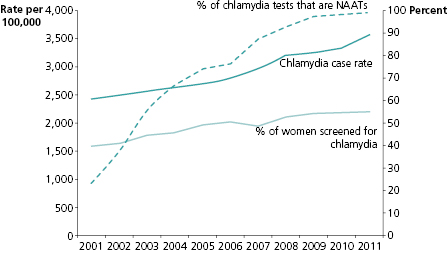
Trends in case-report data must be carefully interpreted. Case-report data are heavily influenced by advances in diagnostic test technology and, for STDs that are usually asymptomatic, by changes in screening coverage. A prominent example of this is found in chlamydia reporting. From 2001 to 2011 reported case rates of chlamydial infection have steadily increased, and rates are considerably higher among females than males [3]. However, this does not necessarily mean that chlamydia incidence is increasing or that incidence is higher in females, however, as these trends must be considered in the context of the U.S. chlamydia control program (Figure 12.1). As untreated chlamydia can lead to infertility, the CDC recommends that all sexually active young females be screened annually for chlamydia [20]. In the United States, screening coverage has increased steadily since 2001 [29]. During the same time period, an increasing number of tests were completed using nucleic acid amplification tests (NAATs), which are more sensitive than previously used chlamydia tests [3]. Consequently increasing rates in females likely reflect an expanding control program. More infections were identified because more women were screened and they were screened using more sensitive tests. Thus, chlamydia case-report data must be interpreted in the context of trends in testing and diagnostic technology.
Sentinel Surveillance
When it is not feasible to conduct surveillance on the entire population, sentinel surveillance strategies may be used. For STDs, sentinel surveillance is often used for monitoring trends in infections that are not nationally reportable or for obtaining information that is not routinely collected on case reports (e.g., individual sexual behavior information or antimicrobial resistance of isolates). The sentinel system may be based on a representative sample of geographic locations, clinics, providers, or patients. For example, the SSuN, in addition to collecting enhanced interview data on a sample of patients diagnosed with gonorrhea, also monitors STDs, STD-related sequelae, and STD-service utilization in a national sample of STD clinics. Findings from SSuN have furthered the understanding of the epidemiology of genital warts by monitoring prevalence by sex and by the sex of the sex partner [3] and by adhering to HIV testing recommendations among patients infected with gonorrhea [30].
Because a limited number of sites are involved, sentinel surveillance allows collection of detailed information. Additionally, sentinel surveillance systems are often flexible and can allow additional data to be collected as epidemics emerge or change. For example, little was known about antimicrobial resistance to Trichomonas vaginalis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


