Global Surveillance for Emerging Infectious Diseases
UPMC Center for Health Security, Baltimore, MD, USA
Introduction
By the middle of the twentieth century, sharp declines in mortality associated with infectious diseases in the United States prompted optimistic views about conquest of infectious agents among medical and public health leaders [1,2]. This short-lived optimism was replaced by new threats, including emergence of human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) and reemergence of drug-resistant tuberculosis [3].
During the last 15 years, several high profile outbreaks have led to calls for enhanced surveillance for infectious diseases. These incidents included the deliberate dissemination of anthrax in the United States during 2001, the rapid spread of severe acute respiratory syndrome (SARS) caused by a novel coronavirus in 2003, the emergence and ongoing zoonotic transmission of highly pathogenic H5N1 avian influenza, and the global pandemic of influenza A/H1N1 in 2009. Each of these events demonstrated the ongoing health risks posed by infectious diseases. Each of these events was associated with significant social and economic consequences felt on a global scale. As a result, there have been increasing efforts to improve infectious disease surveillance around the world.
This chapter focuses on approaches to global surveillance including attributes for indicator-based and event-based systems, outbreak response systems, and key developments including the new International Health Regulations. The increased contributions of nontraditional sectors in surveillance (e.g., the agencies responsible for security are discussed) and current challenges, including insufficient capacity to detect diseases, are highlighted.
Overview of Surveillance
Definition of Terms
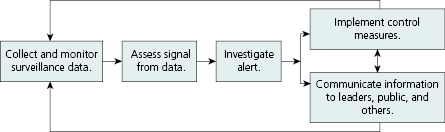
Historically, the term “disease surveillance” has been used to refer to the systematic collection and evaluation of data pertaining distribution and trends of incidence of morbidity and mortality within a population [4]. Disease surveillance is not a single act, but rather a series of actions in a multistep process. The general phases of action that occur in the process disease surveillance are illustrated in Figure 16.1.
Traditionally, surveillance has been the purview of governmental public health agencies and has focused on a predefined list of diseases or conditions, referred to as indicator-based surveillance. The continued emergence of new infectious disease threats, including the potential deliberate use of biological agents as weapons, has led to changes in the practice of infectious disease surveillance. Event-based surveillance is generally used to detect or monitor rare, new, or otherwise unusual events. These systems are not usually tied to a specific disease, and may use strategies like news media scans for reports of undiagnosed outbreaks in rural villages. Events identified via these types of surveillance systems may require an epidemiological investigation to determine whether an event should be of concern to public health authorities. Guidelines from the World Health Organization (WHO) state that event-based surveillance is useful in areas where there are weak traditional indicator-based disease surveillance capacities. A more detailed comparison of indicator- and event-based surveillance is shown in Table 16.1.
Table 16.1 Comparison of key attributes and components of event-based and indicator-based surveillance.
Source: Adapted from A Guide to Establishing Event-based Surveillance. Available at http://www.wpro.who.int/emerging_diseases/documents/docs/eventbasedsurv.pdf. Reprinted with permission of WHO.
| Event-based surveillance | Indicator-based surveillance | |
|---|---|---|
| Case definitions |
|
|
| Timeliness |
|
|
| Data/Information |
|
|
| Reporting structure |
|
|
| Reporting units |
|
|
| Trigger for initial action |
|
|
| Analysis |
|
|
| Response |
|
|
In recent years, a new term, biosurveillance, has been adopted, particularly among those in the U.S. policy community, to describe the broad set of activities involved in monitoring data that may be directly or indirectly related to the health status of plants, animals, or humans in order to improve the abilities to detect, recognize, report, and respond to disease threats [5]. Biosurveillance may include traditional indicator-based disease surveillance approaches and may also include systems that monitor nonhuman or nondisease endpoints. In the United States, for example, the BioWatch program uses air sensors to monitor for the presence of pathogens that may be associated with bioterrorism.
Architecture of Systems for Global Surveillance and Outbreak Response
The primary responsibility for global surveillance belongs to individual countries. Within countries, the entities responsible for carrying out surveillance vary. For example, the United States has a federated system of disease surveillance, in that individual states have primary responsibility for conducting disease surveillance. States report disease surveillance data to the Centers for Disease Control and Prevention (CDC) on a voluntary basis, as discussed in detail in Chapter 3. In other countries, disease surveillance activities are more centralized [6]. For example, in many countries that have national healthcare systems, a national health agency receives disease reports directly from healthcare facilities.
Typically, surveillance activities are indicator-based, organized around specific diseases or conditions, such as HIV or tuberculosis. Increased interest in detecting emerging infectious disease outbreaks and other “unknown” events has prompted increased adoption of event-based surveillance systems. Once a new disease emerges and is recognized, countries may implement dedicated indicator-based surveillance activities. For example, some countries now maintain dedicated surveillance systems for West Nile virus and H5N1 (avian) influenza.
The recognition of outbreaks typically begins with the recognition and reporting of an unusual case or cases of disease or an unusual pattern of illness within a community (e.g., a rare pathogen, unusual frequency or severity of known disease). Reports are often received from astute clinicians or laboratories. Public health authorities may decide to investigate reports to determine whether they are credible or whether they warrant further action. Outbreaks that appear to be credible and that may have international public health significance must be reported to the WHO (see section on International Health Regulations). Countries may then decide to take action or request assistance from the WHO or other countries.
The increasing frequency of disease outbreaks that have spread across national borders has led to the development of multicountry surveillance networks. Some countries have formed agreements and partnerships with their geographic neighbors for the purposes of improving their individual and collective abilities to detect, investigate, and respond to disease outbreaks and epidemics. Countries that participate in surveillance networks typically agree to share disease outbreak information and to collaborate in efforts to control disease spread. They may also share technical methods and other resources that can enhance disease surveillance practices in countries within the network. In some cases, the sharing and joint analysis of surveillance data across a network have contributed to a more complete understanding of the nature of the outbreak [7,8].
Multicountry disease surveillance networks now exist in many parts of the world, such as the Middle East, Southeast Asia, Southern Africa, Southeastern Europe, and East Africa. Examples include the following [9]:
- The Mekong Basin Disease Surveillance (MBDS) network, which includes Cambodia, Southern China, Lao PDR, Myanmar, Thailand, and Vietnam, works to improve surveillance and response to outbreaks of H5N1, cholera, and Dengue hemorrhagic fever. MBDS members have worked together to provide post-disaster relief, for example, during the aftermath of Cyclone Nargis in Myanmar in May 2008.
- The Middle East Consortium on Infectious Disease Surveillance (MECIDS) includes public health experts and ministry of health officials from Israel, the Palestinian Authority, and Jordan. The network has worked to improve regional surveillance for foodborne disease by providing training and by developing standard procedures and a common platform for data sharing and analysis. The network is significant in that its members have had success in finding common ground across borders of countries in conflict.
- The Southern African Centre for Disease Surveillance (SACIDS) includes disease experts from Tanzania, Mozambique, Zambia, the Democratic Republic of Congo, and South Africa. Network members work to improve their capacity to detect, identify, and monitor infectious diseases affecting humans and animals. The network has also partnered with a number of nongovernmental institutions, including Sokoine University of Agriculture (SUA), the Royal Veterinary College, and the London School of Hygiene and Tropical Medicine, to promote sharing of knowledge and resources such as diagnostic equipment and laboratories equipped for biocontainment. The East African Integrated Disease Surveillance Network (EAIDSNet) is a regional, intergovernmental collaborative initiative of the national health and agriculture ministries and the national health research and academic institutions within East Community partner states (Kenya, Uganda, Tanzania, Rwanda, Burundi). The network activities are aimed at enhancing surveillance and response to diseases in humans and animals with the East African partner states.
Key Developments in Approaches to Global Surveillance
2005 Revision to International Health Regulations
Countries have a long had an obligation to conduct surveillance for infectious diseases and to share information about outbreaks with the international community. The International Health Regulations (IHR) codify the measures that countries must take to limit the international spread of disease while ensuring minimum interference with trade and travel. Formally adopted by the 22nd World Health Assembly in 1969, the history of the IHR dates back to discussions in an international sanitary conference in 1851 [10]. For much of their existence, the focus of the IHR has been to require countries to report to the WHO the occurrence of any cases of a short, defined list of diseases, such as cholera or plague.
In 2005, the IHR were significantly revised, in part because of experience during the 2003 SARS outbreak. Global perception that SARS was worsened by China’s lack of communication about the outbreak raised questions about the effectiveness of the existing IHR and prompted calls for the regulations to be updated and strengthened.
The current IHR contain several provisions aimed at strengthening global surveillance. For example, states that are party to IHR are obligated:
- to strengthen and maintain surveillance to detect and assess whether events that may constitute a public health emergency of international concern (PHEIC);
- to notify WHO within 24 hours of all events that qualify as PHEIC, and after notification, submit pertinent data (e.g., laboratory results); and
- to the extent possible, to collaborate with other countries in detection and response to events covered under IHR.
Additionally, IHR grants WHO the authority to consider unofficial reports of disease outbreaks. The rationale for this provision is based on the observation that unofficial reports that an outbreak was occurring in China circulated for months before SARS was officially recognized by any government. At the time, WHO was not able to publicly comment or respond to the reports until it received official notice from the affected country [11]. Under the revised IHR, WHO and other countries can now take better advantage of newer event-based surveillance systems, such as the Public Health Agency of Canada’s Global Public Health Intelligence Network (GPHIN) [12] and the U.S. government’s Project Argus [13], both of which scan news sources worldwide looking for reports of potential disease outbreaks.
Increasing Interest in Surveillance for Security Purposes
Concerns about biological terrorism have raised the profile of infectious disease surveillance in the United States and around the globe [14]. Following the terrorist attacks on the World Trade Center in New York City, the CDC issued a recommendation that healthcare providers and public health practitioners maintain heightened surveillance for any patterns of illness that may be associated with a deliberate release of a biological agent [15]. In October and November of that same year, 22 people were infected and five people died when letters containing powdered anthrax spores were mailed to individuals in Florida, New York, and Washington, D.C. [11]. These events emphasized the connection between global surveillance and security. The conduct of public health surveillance to detect any deliberate release of biological agents is not new: In 1951, the CDC founded the Epidemic Intelligence Service because of concerns about biological warfare arising from the Korean War [12]. Public health practitioners were also instrumental in investigating an outbreak of salmonellosis that was caused when a religious group in The Dalles, Oregon, deliberately contaminated salad bars in the hope of influencing local elections by incapacitating voting members of the community [13].
Security communities recognized the relevance of global surveillance to their goals of protecting the political, economic, and military well-being of nations [16]. Improving global surveillance for biological terrorism and emerging infectious diseases is now a major focus of the U.S. Department of Defense’s (DoD) threat reduction programs [17]. DoD spends more on global health surveillance than any other U.S. governmental agency [18].
Increased Adoption of Syndromic Surveillance Systems
Interest in improving the detection and monitoring of biological attacks and other infectious disease outbreaks has led to increased adoption of new approaches to disease surveillance, such as syndromic surveillance [19]. The initial objective of syndromic surveillance was to increase the speed with which outbreaks or clusters of diseases were detected by examining different types of data that may be associated with changes in health status and are likely to be available sooner than data from traditional reporting sources . Data sources that have been tapped for syndromic surveillance range from volume-of-sales data on over-the-counter medicines to workplace or school absenteeism. New York City, which was among the first to adopt syndromic surveillance methods, implemented a “drop-in” surveillance system in 2001 that monitors data on visits to emergency departments [20].
According to a 2008 survey of U.S. health departments, 88% of respondents reported that they employ syndromic-based approaches as part of routine surveillance [21]. As health departments have gained experience with syndromic surveillance, the way in which these approaches are used has evolved. Whereas the initial objective of syndromic surveillance was to obtain earlier detection of outbreaks than was possible with traditional public health surveillance methods, the focus of these efforts has largely shifted to monitoring the pace and progress of infectious disease outbreaks and other events that may impact public health [22].
Increased Availability of Electronic Health Information
The expansion of the Internet and mobile communication technologies has also had considerable impact on the practice of surveillance. For example, the diffusion of mobile phones into remote areas of the world has also created possibilities for enhanced disease reporting and outbreak detection. As of 2011, close to 6 billion cellular phones were active worldwide, which corresponds to a penetration of 86% of the world’s population [23]. Mobile phones have been used to expedite the reporting of diseases among members of Peru’s Navy [24] and to increase the detection of animal disease outbreaks in Sri Lanka [25].
In addition to helping to improve communication with existing public health surveillance systems, mobile communications and Internet-based tools are making new types of health data available. One of the earliest examples of Internet-based surveillance is ProMED, which was founded in 1993 to provide early warning of emerging infectious disease outbreaks [26]. ProMED scans, translates, and reviews global news reports for evidence of potential outbreaks. It has grown over time to include more than 60,000 subscribers in over 185 countries [27]. ProMED is credited with having provided some of the earliest indications of the start of the 2003 global SARS outbreak [28,29].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


