Gestational trophoblastic disease (GTD) includes a spectrum of interrelated tumors, including complete and partial hydatidiform mole, invasive mole, choriocarcinoma, placental site trophoblastic tumor (PSTT) and epithelioid trophoblastic tumor (ETT) that have varying propensities for local invasion and metastasis (1–3). Persistent GTD, also called gestational trophoblastic neoplasia (GTN), is among the rare human malignancies that can be cured in the presence of widespread metastases (1–3). With the exception of PSTT and ETT, all GTN arises from the cytotrophoblast and syncytial cells of the villous trophoblast, and produces abundant amounts of human chorionic gonadotropin (hCG). Measurement of hCG levels serves as a reliable tumor marker for diagnosis, monitoring of treatment response, and follow-up to detect recurrence.
Placental site and epithelioid trophoblastic tumors originate from the intermediate cells of extravillous trophoblast and produce hCG sparsely, making its use as a tumor marker less reliable. Although GTN most commonly ensues after a molar pregnancy, it may follow any gestational event, including therapeutic or spontaneous abortion and ectopic or term pregnancy.
Prior to the development of effective chemotherapy in 1956, the majority of patients with disease localized to the uterus were cured with hysterectomy, and metastatic disease was almost always fatal. Most women can now be cured and their reproductive function preserved if they are managed according to the well-established guidelines summarized in this chapter.
Hydatidiform Mole
Complete Versus Partial Hydatidiform Mole
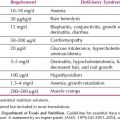
Hydatidiform moles may be categorized as either complete or partial moles on the basis of gross morphology, histopathology, and karyotype (Table 15.1).
Complete Hydatidiform Mole
Pathology
Complete hydatidiform moles lack identifiable embryonic or fetal tissues, and the chorionic villi exhibit generalized hydatidiform swelling and diffuse trophoblastic hyperplasia.
Table 15.1 Features of Complete and Partial Hydatidiform Moles
Chromosomes
Cytogenetic studies have demonstrated that complete moles usually have a 46XX karyotype and the molar chromosomes are entirely of paternal origin (androgenetic) (4). Complete moles appear to arise from an ovum in which the nucleus is either absent or inactivated that has been fertilized by a haploid sperm, which duplicates its own chromosomes (5). Although most complete moles have a 46XX chromosomal pattern, approximately 10% have a 46XY karyotype (6). Chromosomes in a 46XY complete mole appear to be entirely of paternal origin, when an apparently empty egg is fertilized by two sperm (dispermy).
Partial Hydatidiform Mole
Pathology
Partial hydatidiform moles are characterized by the following pathologic features (7):
1. Chorionic villi of varying size with focal hydatidiform swelling and cavitation
2. Marked villous scalloping
3. Focal trophoblastic hyperplasia with or without atypia
4. Prominent stromal trophoblastic inclusions
5. Identifiable embryonic or fetal tissues
Chromosomes
Partial moles usually have a triploid karyotype (69 chromosomes), with the extra haploid set of chromosomes derived from the father (8). When a fetus is present in conjunction with a partial mole, it usually exhibits the stigmata of triploidy, including growth retardation and multiple congenital malformations. In a careful review of our pathologic material, Genest et al. (9) concluded that nontriploid partial moles probably do not exist.
Clinical Features
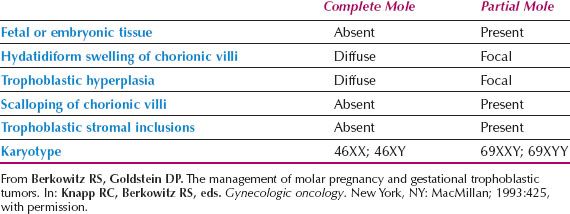
The classical presenting symptoms and signs of patients with complete and partial molar pregnancy are presented in Table 15.2 (10–12). These symptoms have been modified significantly by earlier diagnosis over the past 25 years, with more widespread use of routine ultrasound early in the pregnancy.
Complete Hydatidiform Mole
Vaginal Bleeding
Vaginal bleeding is the most common presenting symptom and occurs in almost all cases. Molar tissues may separate from the decidua and disrupt maternal vessels, and large volumes of retained blood may distend the endometrial cavity. As intrauterine clots undergo oxidation and liquefaction, “prune juice”–like fluid may leak into the vagina. Because vaginal bleeding may be considerable and prolonged, half of these patients present with anemia (hemoglobin <10 g/100 mL).
Table 15.2 Presenting Symptoms and Signs in Patients with Complete and Partial Molar Pregnancy
Excessive Uterine Size
Excessive uterine enlargement relative to gestational age is one of the classic signs of a complete mole, although it was present in only approximately half of our patients. The endometrial cavity may be expanded by both chorionic tissue and retained blood. Excessive uterine size is usually associated with markedly elevated levels of hCG, because uterine enlargement results in part from exuberant trophoblastic growth.
Toxemia
Preeclampsia was observed in approximately 27% of our patients. Although preeclampsia is often associated with hypertension, proteinuria, and hyperreflexia, eclamptic convulsions rarely occur. Toxemia develops almost exclusively in patients with excessive uterine size and markedly elevated hCG levels. The diagnosis of hydatidiform mole should be considered whenever preeclampsia develops early in pregnancy.
Hyperemesis Gravidarum
Hyperemesis requiring antiemetic and/or intravenous replacement therapy occurred in one-fourth of our patients, particularly those with excessive uterine size and markedly elevated hCG levels. Severe disturbances of electrolytes may develop and require treatment with parenteral fluids.
Hyperthyroidism
Clinically evident hyperthyroidism was observed in approximately 7% of our patients. These patients may present with tachycardia, warm skin, and tremor. The diagnosis can be confirmed by detection of elevated serum levels of free thyroxine (T4) and triiodothyronine (T3).
Laboratory evidence of hyperthyroidism is commonly detected in asymptomatic patients with hydatidiform moles. Galton et al. (13) reported 11 patients in whom thyroid function tests were elevated before molar evacuation, but returned rapidly to normal after evacuation.
When hyperthyroidism is suspected, it is important to administer β-adrenergic blocking agents before the induction of anesthesia for molar evacuation, because anesthesia or surgery may precipitate a thyroid storm. The latter may be manifested by hyperthermia, delirium, convulsions, atrial fibrillation, high-output heart failure, or cardiovascular collapse. Administration of β-adrenergic blocking agents prevents or rapidly reverses many of the metabolic and cardiovascular complications of a thyroid storm.
The identity of a thyrotropic factor in hydatidiform moles has not been delineated. Amir et al. measured thyroid function in 47 patients with a complete mole, and reported no correlation between serum hCG levels and the serum free T4 index or free T3 index (14). Thus, although some investigators have speculated about a separate chorionic thyrotropin, this substance has not been isolated.
Trophoblastic Embolization
Respiratory distress developed in approximately 2% of our patients with a complete mole. These patients may experience chest pain, dyspnea, tachypnea, tachycardia, and severe respiratory distress after molar evacuation. Auscultation of the chest usually reveals diffuse rales, and the chest radiograph may demonstrate bilateral pulmonary infiltrates. The signs and symptoms of respiratory distress usually resolve within 72 hours of evacuation with cardiopulmonary support. Respiratory insufficiency may result from trophoblastic embolization, as well as from the cardiopulmonary complications of thyroid storm, toxemia, and massive fluid replacement.
Theca Lutein Ovarian Cysts
Prominent theca lutein ovarian cysts (>6 cm in diameter) developed in approximately half of our patients. These cysts contain amber-colored or serosanguineous fluid, and are usually bilateral and multilocular. Their formation may be related to increased serum levels of hCG and prolactin (15). Ovarian enlargement occurred almost exclusively in patients with markedly elevated hCG values. Because the uterus also may be excessively enlarged, theca lutein cysts may be difficult to palpate, but ultrasonography can accurately document their presence and size. After molar evacuation, theca lutein cysts normally regress spontaneously within 2 to 4 months.
Prominent theca lutein cysts frequently cause symptoms of marked pelvic pressure, which can be relieved by laparoscopic decompression or transabdominal aspiration. If acute pelvic pain develops, laparoscopy should be performed to assess and manage possible cystic torsion or rupture (16).
Prior to the early 1980s, complete moles were usually diagnosed in the second trimester, but the widespread use of ultrasound has shifted the diagnosis to the first trimester (17). With earlier diagnosis, excessive uterine size, hyperemesis, anemia, and preeclampsia were observed at presentation in only 28%, 8%, 5%, and 1% of our patients, respectively. In the 1990s, none of our 74 patients with a complete mole had respiratory distress or hyperthyroidism. However, patients continued to present with vaginal bleeding and markedly elevated hCG levels.
The histopathologic characteristics of complete mole are different in the first trimester (18). First trimester complete moles have less circumferential trophoblastic hyperplasia and smaller villi. These more subtle morphologic alterations may lead to misclassification as partial moles or nonmolar spontaneous abortions. Immunohistochemistry for p57 (paternally imprinted, maternally expressed gene products) may be used to confirm the diagnosis of a complete mole (19). Nuclei of decidual cells (maternally derived tissue) and extravillous trophoblast of all types of gestations stain positively for p57. Almost all complete moles have absent (or near absent) villous stromal and cytotrophoblastic nuclear activity for p57, while all other types of gestations (including partial moles) show nuclear reactivity in more than 25% of villous stromal and cytotrophoblastic nuclei. Fisher et al reported that maternal chromosome 11 was retained in the rare case of complete mole exhibiting p57 staining (20). This also helps to explain the rare occurrence of familial recurrent complete hydatidiform moles of biparental, rather than the usual androgenetic, origin. Familial recurrent molar pregnancy is reported to be strongly associated with a mutation in the NLRP7 gene (21).
Partial Hydatidiform Mole
Patients with a partial hydatidiform mole usually do not have the clinical features characteristic of complete molar pregnancy. In general, these patients present with the signs and symptoms of incomplete or missed abortion, and the diagnosis of partial mole may be made only after histologic review of the curettings (22).
The main presenting sign among 81 patients with a partial mole seen at the New England Trophoblastic Disease Center (NETDC) was vaginal bleeding, which occurred in 59 patients (72.8%) (10). There was absence of a fetal heart beat in 12 patients (14.8%), excessive uterine enlargement in three (3.7%), and preeclampsia in two (2.5%). No patient presented with theca lutein cysts, hyperemesis, or hyperthyroidism. The presenting clinical diagnosis was incomplete or missed abortion in 74 patients (91.4%) and hydatidiform mole in five patients (6.2%). Pre-evacuation hCG levels were measured in 30 patients and were greater than 100,000 milli-International Unit/mL in only two patients (6.7%) (10).
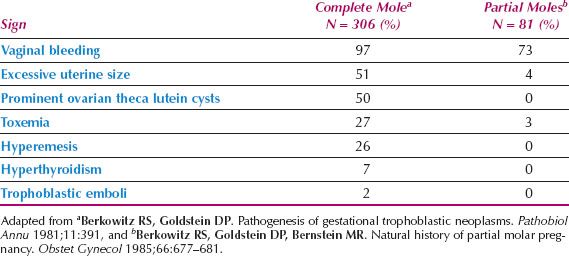
Table 15.3 Sequelae of Low- and High-risk Complete Hydatidiform Moles
Natural History
Complete Hydatidiform Mole
Complete moles have a potential for local invasion and distant spread. After molar evacuation, local uterine invasion occurs in 15% of patients and metastasis in 4% (11,12).
A review of 858 patients with complete hydatidiform mole revealed that two-fifths of the patients had the following signs of marked trophoblastic proliferation at the time of presentation:
1. hCG level greater than 100,000 milli-International Unit/mL
2. Excessive uterine enlargement
3. Theca lutein cysts larger than 6 cm in diameter
Patients with any of these signs are at high risk for postmolar persistent tumor. The sequelae of 858 patients with low- and high-risk complete hydatidiform moles are shown in Table 15.3. After molar evacuation, local uterine invasion occurred in 31%, and metastases in 8.8% of the 352 high-risk patients. For the 506 low-risk patients, local invasion occurred in only 3.4%, and metastases in only 0.6%.
Patients older than 40 years of age are also at increased risk of postmolar GTN. Elias et al. reported that persistent GTN developed in 53% of such women (23).
Partial Hydatidiform Mole
Approximately 2–4% of patients with a partial mole develop persistent postmolar tumor and require chemotherapy to achieve remission (24). Patients who develop persistent disease have no distinguishing clinical or pathologic characteristics.
Diagnosis
Ultrasonography is a reliable and sensitive technique for the diagnosis of complete molar pregnancy. Because the chorionic villi exhibit diffuse hydatidiform swelling, complete moles produce a characteristic vesicular sonographic pattern, usually referred to as a “swiss cheese” pattern. Ultrasonography continues to be useful in the detection of first trimester complete moles (25) (Fig. 15.1).
Ultrasonography may contribute to the diagnosis of partial molar pregnancy by demonstrating focal cystic spaces in the placental tissues and an increase in the transverse diameter of the gestational sac (26).
Treatment
After molar pregnancy is diagnosed, the patient should be evaluated carefully for the presence of associated medical complications, including preeclampsia, hyperthyroidism, electrolyte imbalance, and anemia. After the patient is stabilized, a decision must be made concerning the most appropriate method of evacuation.
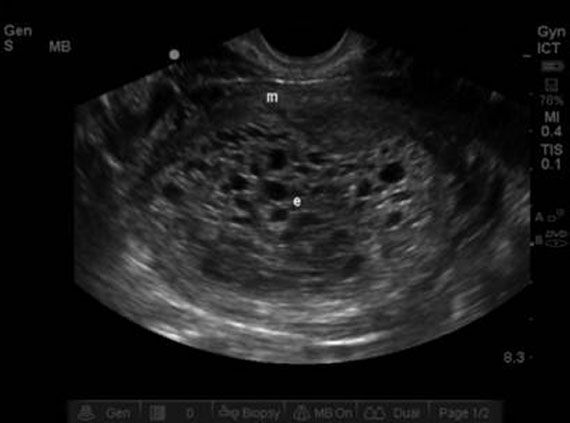
Figure 15.1 Ultrasound showing multiple vesicular endometrial structures consistent with a complete molar pregnancy. A 26-year-old presented at 10 weeks’ gestation with irregular vaginal bleeding. Serum hCG was 120,000 milli-International Unit/mL.
Hysterectomy
If the patient desires surgical sterilization, a hysterectomy may be performed with the mole in situ. The ovaries may be preserved at the time of surgery, even though theca lutein cysts are present. Prominent ovarian cysts may be decompressed by aspiration. Although hysterectomy eliminates the risks associated with local invasion, it does not prevent distant spread.
Suction Curettage
Suction curettage is the preferred method of evacuation in patients who desire to preserve fertility, regardless of uterine size. The procedure involves the following steps:
1. Oxytocin infusion—This is begun in the operating room before the induction of anesthesia.
2. Cervical dilatation—Laminaria or medical effacement agents are utilized by some clinicians to facilitate dilation. While the cervix is being dilated, the surgeon frequently encounters increased uterine bleeding. Retained blood in the endometrial cavity may be expelled during cervical dilatation. Active uterine bleeding should not deter the prompt completion of cervical dilatation.
3. Suction curettage—Evacuation can be facilitated with the use of a large bore cannula. Within a few minutes of commencing suction curettage, the uterus will decrease dramatically in size, and bleeding usually slows. If the uterus is more than 14 weeks in size, one hand may be placed on top of the fundus and the uterus massaged to stimulate uterine contraction and reduce the risk of perforation.
4. Sharp curettage—When suction is thought to be complete, a gentle sharp curettage may be performed to remove any residual molar tissue. Aggressive curettage may result in uterine synechiae, but ultrasonography may help to detect any residual tissue.
The specimens obtained on suction and sharp curettage should be submitted separately for pathologic review.
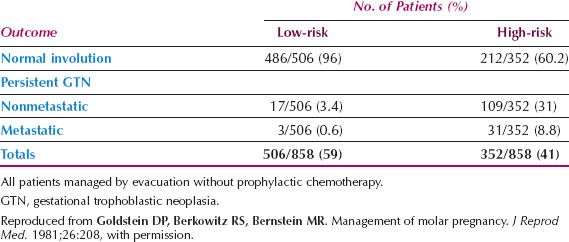
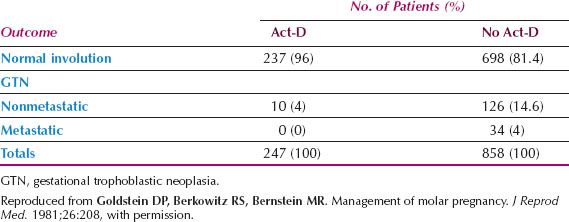
Table 15.4 Prophylactic Actinomycin D (Act-D) after Evacuation for Molar Pregnancy
Prophylactic Chemotherapy
The use of prophylactic chemotherapy at the time of evacuation of a complete mole is controversial. The debate concerns the wisdom of exposing all patients to potentially toxic treatment when only approximately 20% are at risk for development of GTN.
In a study of 247 patients with complete molar pregnancy who received a single course of actinomycin D (Act-D) prophylactically at the time of evacuation, local uterine invasion subsequently developed in only 10 patients (4%), and in no case did metastases occur (Table 15.4). All 10 patients with local invasion achieved remission after only one additional course of chemotherapy (27). Prophylactic chemotherapy prevented metastases and reduced the incidence and morbidity of local uterine invasion.
Kim et al. and Limpongsanurak performed prospective, randomized studies of prophylactic chemotherapy in patients with a complete mole and observed a significant decrease in GTN in patients with high-risk disease (28,29). Therefore, prophylaxis may be particularly useful in the management of a high-risk complete molar pregnancy, especially when hormonal follow-up is unavailable or unreliable.
Follow-up
Human Chorionic Gonadotropin
Human chorionic gonadotropin (hCG) is a predictable secretory product of the trophoblastic cell. Like the other glycoprotein hormones—luteinizing hormone (LH), follicle-stimulating hormone, and thyroid-stimulating hormone—hCG is composed of two polypeptide chains (α and β) attached to a carbohydrate moiety. There is considerable cross-reactivity between hCG and LH because they share indistinguishable α chains. Each of the β chains of these four glycoprotein hormones is biochemically unique and confers biologic and immunologic specificity. The β-subunit radioimmunoassay is the most reliable assay available for the management of patients with GTN and is particularly useful in quantitating low levels of hCG without substantial interference from physiologic levels of LH.
After molar evacuation or hysterectomy with the mole in situ, patients should be followed with weekly β-subunit hCG (B-hCG) levels until they have been undetectable (<5 milli-International Unit/mL) for 3 consecutive weeks, and then monthly levels until they have been undetectable for at least 3 consecutive months. The normal postmolar β-hCG regression curve is presented in Figure 15.2. When a patient with a partial or complete molar pregnancy achieves a nondetectable hCG level, the risk of developing tumor relapse is very low (30–33). Based on these findings, patients are allowed to undertake pregnancy after achieving 3 consecutive weeks of undetectable hCG levels followed by 3 consecutive months of undetectable hCG levels. This is particularly important for those older patients who feel that their window of opportunity for successful pregnancy is closing.
Contraception
Patients should be encouraged to use effective contraception during the entire interval of gonadotropin follow-up. Intrauterine devices should not be inserted until the patient achieves an undetectable hCG levels because of the potential risk of uterine perforation, infection, and bleeding. If the patient does not desire surgical sterilization, the choice is to use either hormonal contraception or barrier methods.
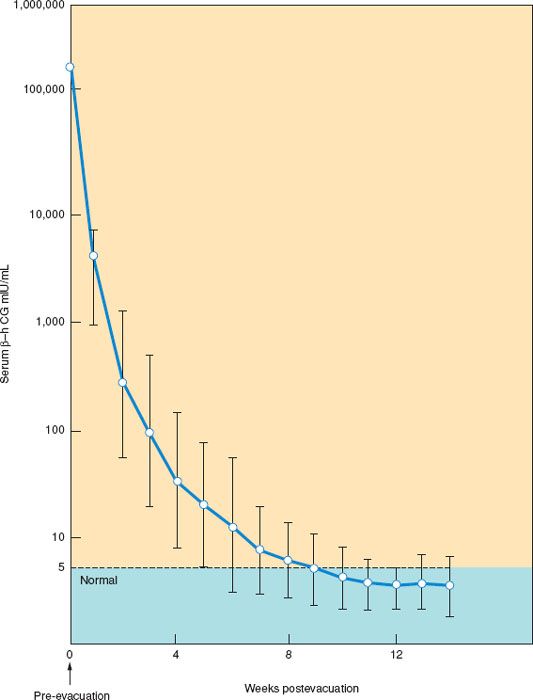
Figure 15.2 Normal regression curve of β-subunit human chorionic gonadotropin (β-hCG) after molar evacuation. (Reprinted from Morrow CP, Kletzky OA, DiSaia PJ, Townsend DE, Mishell DR, Nakamura RM. Clinical and laboratory correlates of molar pregnancy and trophoblastic disease. Am J Obstet Gynecol. 1977;128:424–430, with permission.)
The incidence of postmolar GTN has been reported to be increased among patients who used oral contraceptives before gonadotropin remission (34). Data from both the NETDC and the Gynecologic Oncology Group (GOG) indicate that these agents do not increase the risk of postmolar trophoblastic disease (35,36). In addition, the contraceptive method did not influence the mean hCG regression time. It appears that oral contraceptives may be prescribed safely after molar evacuation during the entire interval of hormonal follow-up.
Gestational Trophoblastic Neoplasia
Nonmetastatic Disease
Locally invasive GTN develops in 15% of patients after evacuation of a complete mole and infrequently after other gestations (11,12). These patients usually present clinically with one or more of the following:
1. Irregular vaginal bleeding
2. Theca lutein cysts
3. Uterine subinvolution or asymmetric enlargement
4. Persistently elevated serum hCG levels
The trophoblastic tumor may perforate through the myometrium causing intraperitoneal bleeding, or erode into uterine vessels causing vaginal hemorrhage (Fig. 15.3). Bulky, necrotic tumor may involve the uterine wall and serve as a nidus for infection. Patients with uterine sepsis present with a purulent vaginal discharge and acute pelvic pain.
After molar evacuation, GTN may exhibit the histologic features of hydatidiform mole, choriocarcinoma, placental site, or epithelioid trophoblastic tumor. After a nonmolar pregnancy, GTN always has the histologic pattern of choriocarcinoma, placental site, or epithelioid trophoblastic tumor. Histologically, choriocarcinoma is characterized by sheets of anaplastic syncytiotrophoblast and cytotrophoblast with no preserved chorionic villous structure.
Placental-Site and Epithelioid Trophoblastic Tumors
Placental-site and epithelioid trophoblastic tumors are uncommon but important variants of GTN that predominantly consist of intermediate trophoblast and a few syncytial elements (37,38). These tumors produce small amounts of hCG and human placental lactogen relative to their mass, and tend to remain confined to the uterus, metastasizing late in their course. In contrast to other trophoblastic tumors, placental-site and epithelioid tumors are relatively insensitive to chemotherapy. High cure rates can be achieved with early diagnosis and surgical resection. Intensive combination chemotherapy may achieve complete remission in patients with metastatic disease, particularly when the interval from the antecedent pregnancy is less than 4 years (39,40).
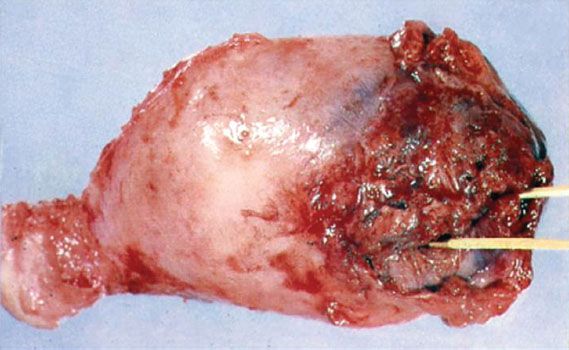
Figure 15.3 Uterus of a patient who presented with heavy vaginal bleeding and hypovolemic shock. A 45-year-old G2 P1 had a preoperative hCG of 510,000 milli-International Unit/mL and at surgery the uterus contained complete molar tissue perforating through the wall.
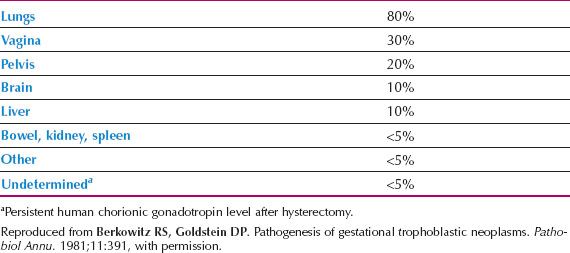
Table 15.5 Relative Incidence of Common Metastatic Sites
Metastatic Disease and Choriocarcinoma
Metastatic GTN occurs in 4% of patients after evacuation of a complete mole and is infrequent after other pregnancies (11,12). Although the precise histology is often not determined, metastasis is usually associated with choriocarcinoma. Diagnosis and treatment are based on rising hCG levels rather than a tissue diagnosis. Approximately one-half of choriocarcinomas follow a hydatidiform mole, and one-half follow nonmolar pregnancies, including term deliveries. Choriocarcinoma is characterized by early vascular invasion and widespread dissemination. Because trophoblastic tumors are quite vascular, metastases may present with symptoms of hemorrhage at the site of a metastasis. Sites of metastatic spread are shown in Table 15.5.
Pulmonary
At the time of presentation, 80% of the patients with metastatic GTN show lung involvement on chest radiographs. Patients with pulmonary metastases may have chest pain, cough, hemoptysis, dyspnea, or an asymptomatic lesion on chest radiographs. Respiratory symptoms may be of acute onset, or they may be protracted over many months.
Gestational trophoblastic neoplasia produces four principal radiographic patterns in the lungs (Fig. 15.4):
1. An alveolar or “snowstorm” pattern
2. Discrete, rounded densities
3. A pleural effusion, or
4. An embolic pattern caused by pulmonary arterial occlusion
Because respiratory symptoms and radiographic findings may be dramatic, the patient may be thought to have a primary pulmonary disease, particularly if the antecedent pregnancy was nonmolar. Gynecologic symptoms may be absent, because the reproductive organs may be free of tumor. The diagnosis of GTN may be confirmed only after thoracotomy, although an hCG level would be diagnostic if the possibility of metastatic trophoblastic disease had been considered.
Pulmonary hypertension may develop in patients with GTN secondary to pulmonary arterial occlusion by trophoblastic emboli. Although patients with pulmonary hypertension may be very symptomatic, the chest film may reveal only minimal changes.
Vaginal
Vaginal metastases are present in 30% of patients with metastatic disease. These lesions are usually highly vascular, and may appear reddened or violaceous. They can bleed vigorously if biopsied, so attempts at histologic confirmation should be resisted. Metastases to the vagina may occur in the fornices or suburethrally, and may produce irregular bleeding or a purulent discharge.
Hepatic
Liver metastases occur in 10% of patients with disseminated trophoblastic tumor. Hepatic involvement is encountered almost exclusively in patients with protracted delays in diagnosis and extensive tumor burdens. Epigastric or right upper quadrant pain may develop if metastases stretch the Glisson capsule. Hepatic lesions are hemorrhagic and friable and may rupture, causing exsanguinating intraperitoneal bleeding. Bakri et al. noted that only 5 of 19 patients (26%) with hepatic metastases presented with liver-related complaints such as jaundice, intra-abdominal bleeding, or epigastric pain (41).
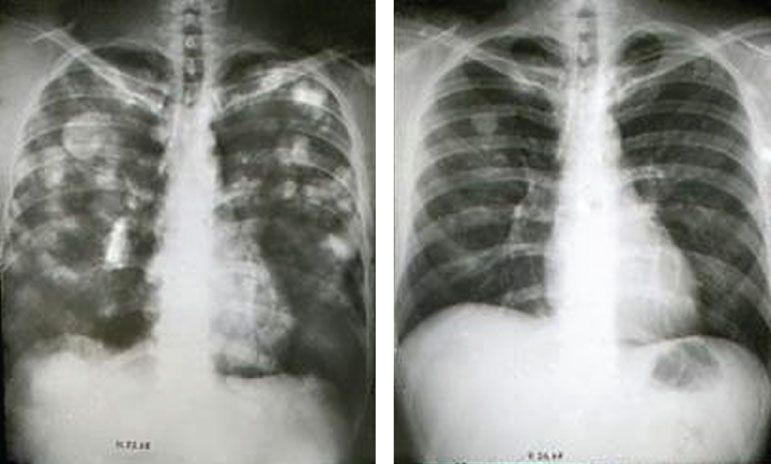
Figure 15.4 Chest x-ray showing multiple pulmonary metastases. A 27-year-old G3 P2 Tab1 presented 8 months after a therapeutic abortion with irregular vaginal bleeding and hemoptysis. Serum hCG was 710,000 milli-International Unit/mL. Following five courses of EMA-CO, the hCG declined to nondetectable levels and the chest x-ray was normal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree