Anemia is a decreased number of circulating red blood cells and is a common medical condition faced in clinical practice. Anemia is caused by loss of red blood cells, destruction of red blood cells, decreased production of red blood cells, or a combination of these processes. Through a clinical history, physical examination, and laboratory evaluation the provider must identify the process by which the patient is anemic. Often the cause of anemia is straightforward; however, the cause can be challenging, requiring a thorough knowledge of both hematology and general medicine.
- •
Anemia is a common clinical question in consultative hematology.
- •
The causes and consequences of anemia have important implications for the care of patients.
- •
Anemia results from 1. red cell loss of sequestration, 2. red cell destruction, or 3. decreased red cell production.
- •
A systematic approach to the evaluation of anemia is needed to diagnose the cause of anemia.
Anemia is one of the most common clinical questions in consultative hematology. The variety of causes and consequences of anemia reflects the key role of blood as a transport and messaging system for the entire body. Traditionally, anemia has been viewed as an innocent bystander, a marker of disease rather than a cause of disease, but emerging evidence suggests that anemia may affect quality of life, cardiovascular health, and mortality.
Despite the association of anemia with a variety of diseases and with adverse clinical outcomes, the hemoglobin concentration that defines anemia is not established and variations within the normal range are associated with disease. The World Health Organization (WHO) in 1958 defined sex-specific hemoglobin targets of 12 g/dL in women and 13 g/dL in men, but acknowledged that “[t]hese figures were chosen arbitrarily and it is still not possible to define normal precisely.” Most clinical laboratories define anemia as the bottom 2.5% of the distribution of hemoglobin values from a healthy population.
The lack of a standard definition complicates the role of the clinician, because small changes in the definition of abnormal can change dramatically the number of people who are anemic. In certain situations, the patient serves as their own reference range and changes in hemoglobin over time may provide an indicator of health or illness. In this review, the epidemiology and risk factors for anemia are discussed and a clinical guide to the evaluation of anemia is presented.
What is anemia?
The Merriam-Webster dictionary defines anemia as “a condition in which the blood is deficient in red blood cells (RBC), in hemoglobin, or in total volume.” In clinical practice, anemia has multiple clinical definitions, usually based on RBC volume or hemoglobin concentration. Table 1 presents multiple standards that are reported for healthy populations; however, many more are available. Most clinical laboratories define abnormal as the bottom 2.5% of the gender-specific population distribution, occasionally including age-specific ranges for adults, and thus reference ranges differ based on the local population.
| Men (g/dL) | Women (g/dL) | |||
|---|---|---|---|---|
| WHO | 13 | 12 | ||
| Williams hematology | 14.0 | 12.3 | ||
| Beutler & Waalen | Age 20–59 y | Age 60 y+ | All ages | |
| White | 13.7 | 13.2 | 12.2 | |
| Black | 12.9 | 12.7 | 11.5 | |
| Boston, MA | 13.5 | 12.0 | ||
| Togo | 11.9 | 10.2 | ||
| Tanzania | 13.7 | 11.1 | ||
| Ethiopia | 13.9 | 12.2 | ||
What are the determinants of hemoglobin concentration?
Hemoglobin concentration is a complex phenotype, controlled by both genetic and environmental factors. Although the environmental risk factors for anemia have been studied for years, we are only just beginning to understand the genetics of hemoglobin concentration.
Genetics
Previous analyses of the genetics of hemoglobin concentration have focused on disease states involving hemoglobin variants (ie, thalassemias, hemoglobin C, S, or E disease), red cell structural and metabolism protein defects (ie, hereditary spherocytosis), and iron metabolism (ie, hemochromatosis). In a recent genome-wide association study of healthy individuals, variations in multiple genes, some known to affect hematopoiesis and others novel, were found that affect hemoglobin concentration ( Table 2 ). These variants explain only some of the observed variation in hemoglobin concentration in individuals with European ancestry, and further work is under way in non-European ancestry populations.
| Protein Name | Chromosome | Function |
|---|---|---|
| Protein C kinase ϵ | 2p21 | Phosphorylates a wide variety of protein targets in cellular signaling |
| Transmembrane protein 163 | 2q21 | Unknown |
| Aminomethyltransferase | 3p21 | Glycene cleavage system |
| v-kit Hardy-Zuckerman 4 feline sarcoma viral oncogene homolog | 4q11 | Transmembrane protein, target for stem cell factor; mutations are associated with various tumors |
| Hereditary hemochromatosis protein | 6p21 | Controls iron absorption by regulating interaction between transferrin and the transferrin receptor |
| HBS1L-like v-myb myeloblastosis viral oncogene homolog | 6q23 | Guanosine triphosphate elongation factor; regulates hematopoiesis; intragenic region associated with modification of severity of sickle cell anemia and thalassemia/hemoglobin E disease |
| Erythropoietin | 7q22 | Regulates red cell production by promoting erythroid differentiation and initiating hemoglobin synthesis |
| Protein kinase, adenosine monophosphate-activated, γ2 noncatalytic subunit | 7q36 | Monitors cellular energy status and inactivates key enzymes involved in regulating synthesis of fatty acids and cholesterol |
| Hexokinase 1 | 10q22 | Phosphorylates glucose to glucose-6-phosphate–energy metabolism |
| SH2B adaptor protein 3 | 12q24 | Signaling protein believed to play a role in hematopoiesis |
| TSHZ3 teashirt zinc finger homeobox 3 | 19q12 | Unknown |
| Transmembrane protease, serine 6 | 22q12 | Hepatic protein, may be involved in regulating iron metabolism |
Age
Age is a known risk factor for anemia, although the physiology is often not completely understood. As we age, a greater proportion of our bone marrow is replaced with fat, leaving fewer hematopoietic elements. In an apparently healthy elderly cohort (age >64 years), the Cardiovascular Health Study, the prevalence of anemia (WHO criteria) at baseline was 8.5%. In another study, for every 10-year increase in age, participants had a 30% increased odds of anemia using the WHO criteria. Whether lower hemoglobin concentrations and increased anemia prevalence represents physiologic aging versus a condition of disease is poorly studied. Several studies in elderly individuals suggest hemoglobin decline is associated with increased mortality.
Race
African Americans have lower hemoglobin levels and a nearly 3-fold increased odds of anemia than whites. Some of the difference is associated with an increased prevalence of hemoglobin variants such as α-thalassemia. When examining the distribution of hemoglobin between African Americans and whites ( Fig. 1 ), the curves are almost identical except for a shift to lower hemoglobin values in African Americans. Whether African Americans tolerate lower hemoglobin concentrations better is not known. In one analysis of elderly individuals, anemia by the WHO criteria was just as poorly tolerated in blacks as in whites.
Gender
Women have lower hemoglobin concentrations than men. Most anemia criteria use sex-specific ranges and thereby the prevalence of anemia differs only slightly between men and women. In younger women, this difference may be partially explained by menstrual blood losses; however, this differences persists into older ages. Again, apart from a shift to lower hemoglobin values, there is no evidence of a skewed distribution in women versus men (see Fig. 1 ). Although there are no outcomes data to support using different hemoglobin criteria for men and women to define anemia, different ranges have been used for many years in clinical practice.
Geography
Environmental factors such as altitude have a profound effect on hemoglobin concentrations. At higher altitudes, decreased oxygen concentrations in the blood provoke a reactive polycythemia, potentially increasing hemoglobin concentrations by more than 2 g/dL in individuals acclimatized to sea level. Polycythemia is seen in some populations native to high altitudes such as the Aymara in South America but not in others such as Tibetans in Asia, suggesting different genetic adaptations to altitude in different populations. Recent studies indicate that there may be geographic differences in hemoglobin concentration independent of altitude, but the impact on health and anemia definitions have not been studied. Apart from incorporating population-specific reference ranges in clinical laboratories serving discrete populations, no effort has been made to account for altitude and geography when establishing normal hemoglobin ranges.
Diseases and Medications
A variety of acute disease conditions affect hemoglobin concentration, but the role of chronic disease conditions is less recognized. Common medical conditions are independently associated with anemia, such as a history of stroke or myocardial infarction, diabetes mellitus, hypertension, and chronic kidney disease. Some common medications such as angiotensin-converting enzyme inhibitors and antiandrogen medications are also associated with anemia.
What are the determinants of hemoglobin concentration?
Hemoglobin concentration is a complex phenotype, controlled by both genetic and environmental factors. Although the environmental risk factors for anemia have been studied for years, we are only just beginning to understand the genetics of hemoglobin concentration.
Genetics
Previous analyses of the genetics of hemoglobin concentration have focused on disease states involving hemoglobin variants (ie, thalassemias, hemoglobin C, S, or E disease), red cell structural and metabolism protein defects (ie, hereditary spherocytosis), and iron metabolism (ie, hemochromatosis). In a recent genome-wide association study of healthy individuals, variations in multiple genes, some known to affect hematopoiesis and others novel, were found that affect hemoglobin concentration ( Table 2 ). These variants explain only some of the observed variation in hemoglobin concentration in individuals with European ancestry, and further work is under way in non-European ancestry populations.
| Protein Name | Chromosome | Function |
|---|---|---|
| Protein C kinase ϵ | 2p21 | Phosphorylates a wide variety of protein targets in cellular signaling |
| Transmembrane protein 163 | 2q21 | Unknown |
| Aminomethyltransferase | 3p21 | Glycene cleavage system |
| v-kit Hardy-Zuckerman 4 feline sarcoma viral oncogene homolog | 4q11 | Transmembrane protein, target for stem cell factor; mutations are associated with various tumors |
| Hereditary hemochromatosis protein | 6p21 | Controls iron absorption by regulating interaction between transferrin and the transferrin receptor |
| HBS1L-like v-myb myeloblastosis viral oncogene homolog | 6q23 | Guanosine triphosphate elongation factor; regulates hematopoiesis; intragenic region associated with modification of severity of sickle cell anemia and thalassemia/hemoglobin E disease |
| Erythropoietin | 7q22 | Regulates red cell production by promoting erythroid differentiation and initiating hemoglobin synthesis |
| Protein kinase, adenosine monophosphate-activated, γ2 noncatalytic subunit | 7q36 | Monitors cellular energy status and inactivates key enzymes involved in regulating synthesis of fatty acids and cholesterol |
| Hexokinase 1 | 10q22 | Phosphorylates glucose to glucose-6-phosphate–energy metabolism |
| SH2B adaptor protein 3 | 12q24 | Signaling protein believed to play a role in hematopoiesis |
| TSHZ3 teashirt zinc finger homeobox 3 | 19q12 | Unknown |
| Transmembrane protease, serine 6 | 22q12 | Hepatic protein, may be involved in regulating iron metabolism |
Age
Age is a known risk factor for anemia, although the physiology is often not completely understood. As we age, a greater proportion of our bone marrow is replaced with fat, leaving fewer hematopoietic elements. In an apparently healthy elderly cohort (age >64 years), the Cardiovascular Health Study, the prevalence of anemia (WHO criteria) at baseline was 8.5%. In another study, for every 10-year increase in age, participants had a 30% increased odds of anemia using the WHO criteria. Whether lower hemoglobin concentrations and increased anemia prevalence represents physiologic aging versus a condition of disease is poorly studied. Several studies in elderly individuals suggest hemoglobin decline is associated with increased mortality.
Race
African Americans have lower hemoglobin levels and a nearly 3-fold increased odds of anemia than whites. Some of the difference is associated with an increased prevalence of hemoglobin variants such as α-thalassemia. When examining the distribution of hemoglobin between African Americans and whites ( Fig. 1 ), the curves are almost identical except for a shift to lower hemoglobin values in African Americans. Whether African Americans tolerate lower hemoglobin concentrations better is not known. In one analysis of elderly individuals, anemia by the WHO criteria was just as poorly tolerated in blacks as in whites.
Gender
Women have lower hemoglobin concentrations than men. Most anemia criteria use sex-specific ranges and thereby the prevalence of anemia differs only slightly between men and women. In younger women, this difference may be partially explained by menstrual blood losses; however, this differences persists into older ages. Again, apart from a shift to lower hemoglobin values, there is no evidence of a skewed distribution in women versus men (see Fig. 1 ). Although there are no outcomes data to support using different hemoglobin criteria for men and women to define anemia, different ranges have been used for many years in clinical practice.
Geography
Environmental factors such as altitude have a profound effect on hemoglobin concentrations. At higher altitudes, decreased oxygen concentrations in the blood provoke a reactive polycythemia, potentially increasing hemoglobin concentrations by more than 2 g/dL in individuals acclimatized to sea level. Polycythemia is seen in some populations native to high altitudes such as the Aymara in South America but not in others such as Tibetans in Asia, suggesting different genetic adaptations to altitude in different populations. Recent studies indicate that there may be geographic differences in hemoglobin concentration independent of altitude, but the impact on health and anemia definitions have not been studied. Apart from incorporating population-specific reference ranges in clinical laboratories serving discrete populations, no effort has been made to account for altitude and geography when establishing normal hemoglobin ranges.
Diseases and Medications
A variety of acute disease conditions affect hemoglobin concentration, but the role of chronic disease conditions is less recognized. Common medical conditions are independently associated with anemia, such as a history of stroke or myocardial infarction, diabetes mellitus, hypertension, and chronic kidney disease. Some common medications such as angiotensin-converting enzyme inhibitors and antiandrogen medications are also associated with anemia.
What are the consequences of anemia?
The effect of severe anemia on cardiovascular function is well recognized in clinical practice. In contrast, less severe anemia has been considered a consequence of disease rather than a cause of disease. A growing body of evidence suggests that anemia and even hemoglobin concentrations within the lower normal range are associated with increased morbidity and mortality in a variety of populations. An alternate approach to defining anemia is to use the individual as their own reference range; a decreasing hemoglobin concentration, even within the normal range, has been shown to relate to future mortality in an elderly population.
Summary
A variety of factors both genetic and environmental can affect hemoglobin concentration and the prevalence of arbitrarily defined anemia. In most cases, a hemoglobin concentration less than 11 g/dL is abnormal. Hemoglobin concentrations between 11 g/dL and 14 g/dL may or may not be normal, depending on the clinical context. The role of the consulting hematologist is to help identify the cause of anemia and when appropriate recommend treatment options. Patients should be given transfusion support when experiencing severe anemia-related symptoms. However, there are no data to show that providing transfusion support for asymptomatic patients with the purpose of bringing hemoglobin concentrations into a specific normal range improves outcomes.
Why is my patient anemic?
The reasons for anemia can be complex and multifactorial. To diagnose and manage anemia, the workup needs a systematic approach. Although there are innumerable immediate causes of anemia, there are only a few overarching reasons why someone is anemic:
- 1.
Blood loss or sequestration
- 2.
Increased destruction of RBC
- 3.
Decreased production of RBC.
Determining which of these processes is occurring in the patient helps determine the cause of the anemia. An initial clinical and laboratory assessment must focus on determining which of these processes are active. An initial workup consisting of a complete blood count, reticulocyte count, a clinical history, and a physical examination can help guide the anemia workup.
Clinical History
A careful history to establish whether or not the patient has an unstable volume is warranted in all anemias. A history of gastrointestinal (GI), urinary, or respiratory blood loss is essential, with confirmatory testing for the presence of blood. A dietary and medication/drug history determines whether the patient is at risk for nutritional deficiencies. The physical examination may help direct the workup for anemia:
- •
Head and neck: the presence of scleral icterus and mucosal jaundice can indicate increased RBC destruction and increase of indirect bilirubin in the serum. Thyromegaly can suggest anemia caused by thyroid disease.
- •
Lymph nodes: lymphadenopathy can denote an underlying infection or malignancy leading to anemia.
- •
Cardiac: the detection of murmurs associated with valvular heart disease can lead to suspicion for increased RBC destruction. In the appropriate clinical scenario, assess for signs of endocarditis, which can lead to both diminished RBC production and increased RBC destruction.
- •
Respiratory: blood loss can present as a hemothorax yielding diminished breath sounds and dullness to percussion. Basilar crackles can suggest congestive heart failure, which is commonly associated with anemia.
- •
Abdominal: detection of an enlarged spleen or liver can signify a malignancy, increased RBC destruction, or RBC sequestration. The presence of a palpable mass is suggestive of malignancy. A fluid wave or shifting dullness in the abdomen also can suggest a malignancy associated with ascites or portal hypertension and cirrhosis. Abdominal distention with tenderness and abdominal wall ecchymosis can denote a retroperitoneal hematoma associated with RBC loss.
- •
Extremities: thigh swelling or ecchymosis can point to a site of bleeding. Joint swelling or deformity can hint at an infectious or rheumatologic process leading to anemia.
- •
Skin: jaundice can be a sign of increased RBC destruction. Rashes can be associated with diseases such as systemic lupus erythematosus or vasculitis, which can lead to anemia.
Laboratory Studies
Several initial laboratory studies guide the workup, as can review of the peripheral smear:
- •
Peripheral smear blood
- ○
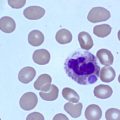
RBC size: the RBC is a biconcave disc that appears as round to slightly ovoid on review of the peripheral smear. Approximately one-third of the center appears paler than the surrounding periphery. A normal RBC is typically the size of the nucleus of a nonreactive lymphocyte, approximately 7 mm ( Fig. 2 A). A change in the cell size or amount of central pallor constitutes an abnormal RBC. RBC greater than 8.5 μm are called macrocytes (see Fig. 2 E). Macrocytic RBC occur with nutritional deficiencies (eg, vitamin B 12 or folic acid), primary bone marrow disorders (eg, myelodysplastic syndromes, multiple myeloma), hypothyroidism, medications (eg, hydroxyurea), excess alcohol consumption and reticulocytosis in response to bleeding or hemolysis. Small RBC, microcytes, are seen with iron deficiency, lead poisoning, thalassemias, abnormal hemoglobins (eg, sickle disease), and sideroblastic anemia (see Fig. 2 C). Spherocytes are small RBC less than 6.5 μm with absent central pallor (see Fig. 2 D) seen in hereditary spherocytosis and autoimmune hemolytic anemias.
Fig. 2
Peripheral smears. ( A ) Normal RBC morphology. Note central pallor occupying approximately one-third of cell. ( B ) Schistocytes and burr cells consistent with microangiopathic hemolytic anemia. ( C ) Hypochromic microcytic RBC consistent with IDA. ( D ) Spherocytes as seen in hereditary spherocytosis or autoimmune hemolytic anemia. ( E ) Megaloblastic RBC with a hypersegmented neutrophil as seen in vitamin B 12 deficiency. ( F ) Nucleated RBC and tear-drop cells consistent with leukoerythroblastic syndrome as seen in bone marrow infiltration.
( Courtesy of John H. Lunde, Medical Director of the Hematology Lab.)
- ○
RBC shape: when viewing the peripheral blood smear it is important to consider the shape of the RBC. Several distinct shapes can suggest a diagnosis. Schistocytes are small fragmented pieces of RBC caused by hemolysis (see Fig. 2 B). Target cells, codocytes, are small RBC with a central area of pigmentation. Target cells are present in the hemoglobinopathies and may also appear in iron-deficiency anemia (IDA). Dacrocytes, tear-drop cells, appear in the presence of myelophthisis or leukoerythroblastosis when the bone marrow is infiltrated by another process (see Fig. 2 F). Sickle cells are present in the sickle hemoglobinopathies. Rouleaux formation or the appearance of RBC as a coin stack can be present in Waldenstrom macroglobulinemia, multiple myeloma, and inflammatory states. Clumping of RBC suggest cold antibodies.
- ○
Abnormal circulating cells: the peripheral smear can reveal crucial information beyond direct visualization of the RBC. Review of the circulating white blood cells (WBC) and platelets is essential. Hypersegmented neutrophils, neutrophils with greater than 6 nuclear lobes, may be present in vitamin B 12 deficiency (see Fig. 2 C). Immature lymphocytes or numerous lymphocytes can reveal the diagnosis of acute or chronic leukemias, respectively. Abnormal platelets can raise suspicion for the myelodysplastic or myeloproliferative disorders.
- ○
- •
Red cell distribution width (RDW): the RDW is a measure in the variation of the size of RBC, with an abnormally high RDW indicating increased RBC variation. An increased RDW is the first sign of an iron-depleted state and when noted in the setting of microcytosis is consistent with IDA. An increased RDW with macrocytosis can indicate a mixed nutritional deficiency (eg, combined iron and vitamin B 12 or folic acid deficiency), or reticulocytosis in response to either RBC loss, RBC destruction, or correction of a nutritional deficiency.
- •
Reticulocyte count: a reticulocyte count helps differentiate anemias of increased RBC loss/destruction from anemias of decreased RBC production. Reticulocytes are young RBC forced into the circulation in response to increased RBC loss or destruction. A low reticulocyte count with anemia suggests decreased RBC production or inadequate time for RBC production to increase. Reticulocytes can be reported as either a percentage of RBC or as an absolute count. If the reticulocytes are presented as a percentage of RBC, a correction factor ( corrected reticuocyte count = % reticulocytes × ( Patient Hct Normal Hct ) ) should be applied to adjust for the severity of anemia.
- •
Other initial laboratory tests: increases in lactate dehydrogenase (LDH) and indirect bilirubin levels with a decrease in haptoglobin level are signs of increased RBC destruction. A positive direct antibody test (DAT) is suggestive of immune-mediated RBC destruction.
Red blood cell (RBC) loss or dilution anemia
There are many potential sources of RBC loss. These sources include occult GI bleeding, urologic bleeding, menstruation, pulmonary bleeding, and phlebotomies (eg, blood donation, laboratory testing). Blood loss must be addressed as a potential cause for all anemias because identification of an early-stage malignancy such as colon cancer can be potentially life saving. Indolent blood loss over a period of time often results in iron deficiency and loss of the ability of the bone marrow to properly increase RBC production. Anemia secondary to blood loss and IDA should prompt a complete workup in men, regardless of age, and in postmenopausal women for a source of bleeding. In menstruating women, an initial trial of iron is warranted, but with further evaluation if there is no response to therapy. Occasionally, anemia is secondary to an increased plasma volume rather than a decrease in RBC mass. The only common clinical situations in which this situation occurs are pregnancy and iatrogenic fluid overload from intravenous fluids. Hemoglobin concentration in pregnancy is typically reduced to 11 to 12 g/dL.
Clinical History
Careful questioning about blood loss is important. Unless there is evidence of an overdose, blood loss on anticoagulant and antithrombotic medications is not physiologic and the source must be identified rather than attributed to anticoagulation.
GI blood losses are one of the most common sources of blood loss. Past history of medications that can cause GI ulceration or inflammation such as nonsteroidal antiinflammatory agents, aspirin, and bisphosphonates may help the practitioner narrow down potential sources. A history of gastric reflux symptoms or use of gastric reflux medications may indicate the potential for GI blood loss secondary to chronic gastritis. Patients may report hematemesis with either bright red blood or emesis described as like coffee grounds in appearance. Questioning about bright red blood with bowel movements, dark tarry stools or melena, known diverticular disease, or previous diverticular bleeding are important to identify possible GI losses. Occasionally, swallowed blood from the upper respiratory tract can present as apparent GI blood loss. Confirmation of colorectal cancer screening is crucial.
In women, a careful menstrual history is mandatory, including the amount of blood loss, the frequency of periods, and the duration of menstruation. The prevalence of IDA in menstruating women is reported to be between 25% and 47.5%. Women with decreases in iron intake or even small increases in blood loss as seen in menorrhagia or metrorrhagia can further deplete iron stores, contributing to worsened anemia.
Urinary blood loss is often underappreciated. Changes in urine color, with variations of a pink tint to deep red, can point to a urinary source. Microscopic hematuria may represent underlying urinary disease, including benign prostatic hypertrophy, renal calculi, polycystic kidney disease, or more concerning causes such as bladder, prostate, or kidney cancer. Intrinsic renal disease represents another potential for microscopic hematuria that can result in IDA.
Pulmonary and upper airway bleeding often present as varying degrees of hemoptysis. Patients may ascribe to a chronic cough with hemoptysis described as either obvious blood-colored or rust-colored sputum, raising suspicion of a pulmonary lesion. Patients may not recognize hemoptysis because most sputum is swallowed and never visualized.
There are several potential spaces within the body that can sequester large amounts of blood and be relatively asymptomatic: the pleural space, the retroperitoneal space, and the thigh. Trauma, even minor, especially in the setting of antithrombotic or anticoagulant medications can result in significant blood loss. Intracranial, retinal, or joint space hemorrhages are small in volume and are unlikely to present as anemia. Hip or flank pain, vague abdominal complaints, and lower extremity paresis can be symptoms associated with retroperitoneal hemorrage.
A careful history of blood donation, frequency of phlebotomy for laboratory examinations, and potential surreptitious phlebotomy should be obtained. Iron deficiency from blood donation is a reported cause of anemia. Repetitive phlebotomy during hospitalization can result in a meaningful decline in hemoglobin. Rarely, Munchausen syndrome has been associated with anemia in patients seeking unneeded therapy by bloodletting or intentional diet modifications.
Physical Examination
The focus of the physical examination depends largely on the acuity of the blood loss. Orthostatic vital signs are important in acute blood loss because a patient at rest can seem hemodynamically stable and become profoundly hypotensive with standing. GI blood loss may be evident on nasogastric lavage or digital rectal examination. Inspection of the urine color may reveal hematuria. Suspicion of gynecologic bleeding requires a complete pelvic examination. Trauma, lacerations, or venous puncture sites may be visible. A complete musculoskeletal examination may reveal focal pain or swelling, suggesting a hematoma or internal blood loss.
Laboratory Findings
The severity of anemia varies depending on the amount and chronicity of blood loss. Typically, anemia of acute blood loss remains normocytic and as iron stores are depleted the RDW increases and the mean corpuscular volume (MCV) decreases. Initial screening tests include stool for occult blood, urinalysis, or sputum analysis, as directed by the clinical history. Localized complaints of pain or swelling may represent collections of blood and can direct imaging studies. If a patient history and workup are consistent with blood loss, a negative screen for bleeding does not eliminate the need for direct imaging of likely sites by procedures such as colonoscopy, esophagogastroduodenoscopy, or visualization of the upper aerodigestive tract by endoscopy.
Red Blood Cell (RBC) Destruction
RBC destruction is a challenging cause of anemia because of the large number of conditions in the differential diagnosis. The normal erythrocyte has a life span of approximately 100 to 140 days. The processes through which the body identifies older or damaged RBC for clearance are not fully understood; hypotheses include decreased deformability or alterations in the RBC membrane. There are two main sites for the body to destroy RBC: within the blood vessels (intravascular hemolysis) and ingestion of RBC by macrophages in the spleen and liver (extravascular hemolysis).
Intravascular
Under normal circumstances, only some RBC are destroyed in the vascular space. Circulating haptoglobin binds to free hemoglobin, and haptoglobin-hemoglobin complexes are cleared by the liver, with the hemoglobin converted to iron and biliverdin (further converted to bilirubin).
Extravascular
Macrophages in the spleen and liver engulf RBC and heme is cleaved into iron and biliverdin, which is later converted into bilirubin. This is the main route for normal RBC catabolism. Haptoglobin is decreased in extravascular hemolysis as well from hemoglobin spilling from macrophages.
It is possible to divide hemolytic anemias into intravascular and extravascular processes; however, the cause often overlaps between these 2 processes. Further, chronic RBC destruction can lead to nutritional deficiencies such as iron deficiency from urinary losses and folate deficiency from increased nucleic acid turnover. A reasonable clinical approach is to divide hemolysis into mechanical, immune-mediated, and intrinsic RBC abnormalities and recognize that the destruction can occur at multiple sites.
Mechanical
Within blood vessels, RBC can be destroyed by physical trauma such as from prosthetic cardiac valves and by repetitive trauma of vascular beds, as is seen in march hemoglobinuria. Pathologic processes such as systemic infections, thrombotic thrombocytopenic purpura (TTP), and vasculitis sheer RBC passing through obstructed small vessels. Injury from toxins and heat as well as injury from parasites such as malaria and Babesia and bacteria such as Clostridium species are other possible means of RBC destruction.
Immune-mediated
Immune-mediated destruction or RBC can be from autoreactive antibodies or alloreactive antibodies. Autologous antibodies can result from neoplastic, infectious, drug-associated, and idiopathic processes, whereas alloreactive antibodies are not apparent unless there is sensitization and exposure to allergenic RBC. Depending on the antibody, immune-mediated hemolysis can occur in the intravascular space, extravascular space, or both.
Hereditary syndromes
Hereditary syndromes can present as chronic hemolysis throughout the lifetime of the individual or as paroxysms of hemolysis with an environmental trigger. A full discussion of hemoglobin variants (ie, sickle cell anemia, thalassemias) is beyond the scope of this review but should be considered in the appropriate clinical setting. Carriers of hemoglobin S, C, and E rarely have obvious hematologic abnormalities, but carriers of thalassemia minor (both α and β) may be microcytic and mildly anemic. An important group of patients are those with RBC enzyme deficiencies because these can present in adulthood as specific episodes of hemolysis caused by an environmental trigger.
Clinical History and Physical Examination
A clinical history suggestive of RBC destruction includes the normal signs and symptoms of anemia (eg, fatigue, pallor). Hemolysis should be strongly suspected with a history of jaundice and changes in urine color. A careful history of recent illnesses and medications is important in the diagnosis of immune-mediated hemolysis or drug-induced hemolysis. Review of travel history, sick contacts, and sexual history may be clues of underlying infections. Hemolysis can be associated with a hypercoagulable state and patients may present with venous thromboembolic disease.
The physical examination is useful in assessing the stability of the patient. Most patients with hemolysis have jaundice. If there is an underlying infectious or neoplastic disorder, lymphadenopathy or splenomegaly may be apparent. Patients with vasculitis may present with neurologic complaints and skin lesions. Patients with TTP or hemolytic uremic syndrome (HUS) may have accompanying symptoms, including fevers and neurologic complaints. Occasionally, patients present with cholelithisis or cholecystitis from pigmented gallstones.
Laboratory Findings
The degree of anemia is variable in hemolytic anemias and can range from mild to severe. Markers of hemolysis such as LDH, indirect bilirubin, and urinary urobilinogen are increased, and haptoglobin is suppressed. A reticulocyte count is usually increased except in acute hemolysis in which the bone marrow has not had a chance to increase RBC production or in chronic hemolysis if individuals have developed concurrent nutritional deficiencies.
Review of the peripheral blood smear is important. In nonimmune-mediated hemolysis, the peripheral blood smear may reveal characteristic burr cells, schistocytes, helmet cells, and microspherocytes from physical destruction of the RBC (see Fig. 2 B). In immune-mediated hemolysis, the peripheral smear may reveal spherocytes, fragmented red cells, acanthocytes, bite or blister cells, or RBC clumping (see Fig. 2 D).
Mechanical hemolysis
Mechanical breakdown of RBC is the result of physical trauma, microangiopathic hemolysis, infections associated with destruction, and several other miscellaneous processes.
- •
Physical trauma: repetitive trauma to vascular beds can cause destruction of erythrocytes, as seen in runners or in soldiers forced to march long distances, resulting in march hemoglobinuria. Individuals present with discrete episodes of hemolysis, which may include dark urine or muscle aches/pains. Laboratory and physical examination findings are usually negative but occasionally jaundice and hepatosplenomegaly are present. Malfunctioning prosthetic cardiac valves or abnormalities of native valves can cause shearing of RBC and hemolysis. Hemolysis is seen in many prosthetic valves, with a higher risk in mitral versus aortic valve replacement and mechanical versus bioprosthetic valves. Review of the peripheral smear shows red cell fragments (see Fig. 2 B).
- •
Microangiopathic hemolytic anemia: the underlying process is destruction or shearing of the RBC in the microcirculation and leads to the classic finding of schistocytes or helmet cells on review of the peripheral blood smear (see Fig. 2 B). Schistocytes are seen in most individuals; however, in pathologic conditions, the percentage of schistocytes usually exceeds 1%. Signs and symptoms of anemia are often secondary to signs and symptoms of the underlying disorder. The clinical setting varies, but markers of hemolysis (increased LDH, decreased haptoglobin) are almost universally present. Disorders that can cause a microangiopathic hemolytic anemia include TTP, HUS, systemic infections (with or without diffuse intravascular coagulation), systemic malignancy, malignant hypertension, and preeclampsia/HELLP syndrome in pregnant women. In general, coagulation studies are normal and the diagnosis is made with clinical criteria in the setting of a microangiopathic hemolytic anemia on peripheral blood smear. The diagnosis and treatment of microangiopathic hemolytic anemias is complex and an accurate diagnosis is important. Classic TTP can be diagnosed with low levels of the ADAMTS13 protease and an excess of high-molecular-weight Von Willebrand multimers. The diagnosis of other microangiopathic hemolytic anemias has recently been reviewed.
- •
Infections: malaria and Babesia are parasites that reside within the RBC. Intravascular hemolysis occurs as a result of reproduction of the parasites within the RBC. Severe malarial infections can mimic the signs and symptoms of TTP; however, review of the peripheral smear reveals parasites within RBC. Toxins produced by infections such as E coli O157:H7 and Clostridium species result in direct RBC destruction; diagnosis is made by the clinical history and isolation of bacterial toxins from stool or bacteria from the blood ( Table 3 ).