Lymph node or spleen enlargement may be innocent or the first sign of a serious disorder. Lymphadenopathy and splenomegaly can be found in symptomatic or asymptomatic patients. Lymph node enlargement in a single region or multiple sites can be seen in various diseases, including infections, noninfectious inflammatory conditions, or malignancies; a similar differential diagnosis applies to splenomegaly, but splenomegaly can also be caused by vascular abnormalities and hemolysis. Frequently, lymphadenopathy is detected incidentally during screening examinations or imaging procedures. This review focuses on causes of lymphadenopathy and splenomegaly and an appropriate diagnostic approach to patients with lymphadenopathy or splenomegaly.
Enlarged lymph nodes or a palpable spleen tip are exceptionally common physical findings and are not always signs of disease. For instance, in one US pediatric practice, 45% of children aged 5 years or less had palpable lymph nodes in the head and neck region. However, lymphadenopathy or splenomegaly may also be the first sign, or even the only sign, of a serious or life-threatening condition, so physicians must be able to judge accurately when lymphadenopathy or splenomegaly are potentially pathologic, and clinicians should be comfortable with contemporary diagnostic approaches to evaluate these findings.
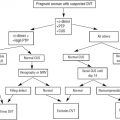
Lymphadenopathy and splenomegaly can be detected in symptomatic or asymptomatic patients. The possible causes of each finding are diverse, with a broad differential diagnosis ranging from nonmalignant conditions, such as inflammatory disorders or acute or chronic infections, to malignant processes, including hematologic malignancies or metastatic carcinomas. The sites and characteristics of lymphadenopathy, as well as age of the patient and presence or absence of associated symptoms such as constitutional symptoms, fevers, weight loss, or other physical findings, can help direct evaluation and can point to a specific cause of the lymphadenopathy. In most cases of persistent lymphadenopathy or splenomegaly, pathologic (tissue) diagnosis is necessary to rule out malignant conditions.
Mechanisms of lymphadenopathy
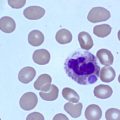
Physical enlargement of a lymph node can occur via several processes. Polyclonal lymphocyte proliferation due to a reaction to a specific group of antigens or monoclonal proliferation from malignant transformation of a lymphoid cell can increase the size and number of lymph node follicles, thereby expanding the node. Enlargement of a lymph node can also occur due to infiltration of the node by nonlymphoid cells, such as inflammatory reaction by neutrophils in lymphadenitis, or metastatic spread of cancer cells from a primary site of neoplasia. In addition, systemic processes can cause a release of cytokines resulting in edema of lymph nodes; such cytokine-mediated adenopathy is usually diffuse and not localized to a single node or nodal group. In metabolic storage disorders, engorged macrophages can accumulate in a lymph node, causing enlargement.
Mechanisms of splenomegaly
Because the splenic white pulp serves as an active immune organ with efferent lymphatic vessels, the mechanisms by which splenomegaly can occur overlap with the mechanisms that cause lymphadenopathy. Because the spleen is also a phagocytic organ with mechanical filtration capability (eg, for senescent erythrocytes) as well as a potential site of hematopoiesis, there are additional mechanisms for splenomegaly, including brisk hemolysis and extramedullary hematopoiesis. Furthermore, splenomegaly can also occur due to disruption of venous blood flow from the organ, such as splenic or portal vein thrombosis, or portal hypertension due to intrinsic hepatic disease.
Mechanisms of splenomegaly
Because the splenic white pulp serves as an active immune organ with efferent lymphatic vessels, the mechanisms by which splenomegaly can occur overlap with the mechanisms that cause lymphadenopathy. Because the spleen is also a phagocytic organ with mechanical filtration capability (eg, for senescent erythrocytes) as well as a potential site of hematopoiesis, there are additional mechanisms for splenomegaly, including brisk hemolysis and extramedullary hematopoiesis. Furthermore, splenomegaly can also occur due to disruption of venous blood flow from the organ, such as splenic or portal vein thrombosis, or portal hypertension due to intrinsic hepatic disease.
Location of lymphadenopathy
The normal peripheral lymph node chains in the body are responsible for drainage of lymphatic fluid from specific anatomic locations ( Table 1 ). Drainage patterns of deep/central lymph nodes (eg, mesenteric, retroperitoneal) are less predictable, although unilateral hilar lung node enlargement usually reflects a pathologic process in the ipsilateral lung. Enlargement of peripheral lymph nodes in a specific area may point to a regional source of the abnormality, but this is not always reliable. A differential diagnosis of lymphadenopathy according to the sites of pathologic enlargement is shown in Box 1 . Although a search for enlarged lymph nodes is one of the most important components of a physical examination, discussion of specific physical examination techniques is beyond the scope of this review.
| Lymph Node Group | Sites |
|---|---|
| Preauricular | Conjunctiva, anterior and temporal scalp, anterior ear canal |
| Posterior auricular | Parietal and temporal scalp |
| Parotid | Forehead, midface, temporal scalp, external ear canal, middle ear, parotid glands, gums |
| Cervical-superficial | Parotid gland, lower larynx, lower ear canal |
| Cervical | Larynx, thyroid, palate, esophagus, paranasal sinuses, tonsils, adenoids, posterior scalp and neck, nose |
| Occipital | Posterior scalp |
| Submandibular | Nose, lips, tongue, cheek, submandibular gland, buccal mucosa |
| Submental | Floor of mouth, lower lip |
| Supraclavicular | Chest and abdomen (left supraclavicular, abdomen; right supraclavicular, mediastinum and lungs) |
| Axillary | Lower neck, upper extremity, lateral breast, chest wall |
| Deltopectoral | Upper extremity |
| Epitrochlear | Upper extremity below the elbow |
| Inguinal | Lower extremity, genital region, buttock, abdominal wall below the umbilicus |
| Popliteal | Lower extremity below the knee |
Generalized lymphadenopathy
Infections :
Viral: common upper respiratory tract infections; infections caused by Epstein-Barr virus, cytomegalovirus, human immunodeficiency virus, varicella-zoster virus, human T cell lymphotropic virus, and adenovirus; measles; rubella typhoid fever; syphilis; plague
Bacterial: a broad range of bacterial infectious, including those caused by Bartonella , tuberculosis, nontubercular mycobacterial infections, syphilis
Protozoal: toxoplasmosis
Fungal: coccidioidomycosis
Malignancy: non-Hodgkin lymphoma, Hodgkin lymphoma, chronic lymphocytic leukemia, acute lymphoblastic leukemia
Autoimmune disorders: rheumatoid arthritis, systemic lupus erythematosus
Noninfectious granulomatous disease: sarcoidosis
Atypical lymphoproliferative disorders
Angioimmunoblastic lymphadenopathy
Atypical cellular disorders
Cervical lymphadenopathy
Infections: dental abscess; otitis media and externa; pharyngitis; toxoplasmosis; and infections caused by Epstein-Barr virus, cytomegalovirus, and adenovirus; hepatitis; rubella
Malignancies: non-Hodgkin lymphoma, Hodgkin disease, head and neck cancer
Kikuchi disease
Supraclavicular lymphadenopathy
Malignancy: thoracic, abdominal
Diseases of the thyroid and larynx
Infections: tuberculosis, fungal infection
Axillary lymphadenopathy
Infection: infections caused by Staphylococcus and Streptococcus , sporotrichosis, cat-scratch disease, tularemia
Malignancies: breast cancer, non-Hodgkin lymphoma
Hilar and mediastinal lymphadenopathy
Hilar unilateral
Infection: bacterial, mycobacterial, and fungal infections; pertussis; tularemia; psittacosis
Malignancy: lung, breast, or gastrointestinal cancer; Hodgkin disease; non-Hodgkin lymphoma
Granulomatous disease
Hilar bilateral, mediastinal
Infection
Malignancy: metastatic cancer, Hodgkin disease, non-Hodgkin lymphoma
Granulomatous disease
Abdominal lymphadenopathy
Malignancy: metastatic gastrointestinal cancer, non-Hodgkin lymphoma, Hodgkin disease, chronic lymphocytic leukemia, urinary transitional cell carcinoma
Infection: tuberculosis
Epitrochlear lymphadenopathy
Connective tissue disorders
Granulomatous disease: sarcoidosis
Dermatologic disease
Syphilis, leishmaniasis, leprosy, rubella
Inguinal lymphadenopathy
Reactive
Malignancy: non-Hodgkin lymphoma, Hodgkin disease, melanoma, squamous cell cancer of the vulva, penis cancer, anal cancer
Infection: cellulitis, sexually transmitted diseases
Generalized Lymphadenopathy
Malignant, inflammatory, and infectious causes can all cause generalized lymphadenopathy. Hematologic malignancies (most commonly lymphoid neoplasms: acute lymphoblastic leukemia [ALL], chronic lymphocytic leukemia [CLL], and Hodgkin and non-Hodgkin lymphomas) and infectious processes (infectious mononucleosis and a diverse roster of other viral, bacterial, and fungal processes) can cause a diffuse nodal reaction, as can advanced carcinomas. Rarely, mesenchymal tumors such as rhabdomyosarcoma or neuroblastoma can present with adenopathy. Hypersensitivity reactions to drugs should be considered, especially if rash, fever, or eosinophilia is present.
Cervical and Occipital Lymphadenopathy
Enlargement of cervical lymph nodes is most commonly caused by an infection in the head and neck region; malignancy is the second most common cause. Infectious causes include pharyngitis, otitis (media and external), dental abscesses, and scalp infections; cervical adenopathy may also be the only sign of systemic infections including infectious mononucleosis or infection caused by cytomegalovirus (CMV). Among malignancies, lymphoma (Hodgkin and non-Hodgkin lymphomas) and head and neck cancers are the most common causes of cervical adenopathy. Small preauricular nodes may be palpable in conjunctivitis or ocular lymphoproliferative disorders. Localized lymphadenopathy in the posterior cervical chains can be seen in histiocytic necrotizing lymphadenopathy (Kikuchi disease), toxoplasmosis, or rubella. Computed tomographic (CT) and ultrasonographic studies have been reported to help differentiate malignant versus reactive lymph nodes, but their test characteristics in this region remain uncertain and biopsy is often necessary for adenopathy that persists beyond 2 to 3 weeks without known cause.
In a study of 155 patients who presented with lymphadenopathy in the cervical region without prior history of malignancy, histologic diagnosis could be made by core needle biopsy in 146 (94%) patients. The pathologic examination results showed 44 cases of reactive hyperplasia, 37 cases of tuberculosis, 25 cases of Kikuchi disease, 16 cases of metastatic malignancies, 16 cases of lymphoma, 1 diagnosis of toxoplasmosis, and normal findings in 7 patients. The study reported sensitivity, specificity, and accuracy of sonographically guided core biopsy of 97.9%, 99.1%, and 97.9%, respectively.
Enlargement of salivary glands can mimic adenopathy. Rheumatologic causes in one series underlied 4% of all cases of cervical lymphadenopathy.
Supraclavicular Lymphadenopathy
Abdominal and thoracic malignancies may metastasize to supraclavicular lymph nodes. Supraclavicular adenopathy, especially unilateral left-sided (ie, Troisier or Virchow sentinel node, named after French pathologist Charles Emile Troisier [1844–1919] or German pathologist Rudolf Virchow [1821–1902]), can be the first sign of a visceral malignancy, including cancer of the gastroesophageal junction or stomach or of other intrathoracic or intra-abdominal organs. Infectious causes, as already mentioned, may cause enlargement in several lymph node chains, including supraclavicular nodes, which may be the only palpable peripheral nodal group. Less commonly reported causes of supraclavicular lymphadenopathy include silicone breast implants or amyloidosis.
The term Delphian node, evoking the classical oracle at Delphi, Greece, refers to a midline prelaryngeal node that could be a sign of laryngeal or thyroid cancer or inflammatory thyroid disease (eg, Hashimoto thyroiditis).
Axillary Lymphadenopathy
Similar to most other lymph node chain enlargements, infections and malignancies are the 2 most common causes of axillary lymphadenopathy. Common malignancies presenting as axillary adenopathy include lymphoproliferative neoplasms and breast carcinoma. Occasionally, a left axillary lymph node may be a metastasis from gastric carcinoma, also called Irish node. Infectious causes of axillary adenopathy include Staphylococcus and Streptococcus skin infections and other infections of the hand or arm (eg, sporotrichosis, cat-scratch disease due to Bartonella organisms). Patients, especially small children, may not recall a recent hand injury because the incubation period between inoculation and axillary adenopathy may be as long as 2 months.
Mediastinal and Hilar Lymphadenopathy
The causes of intrathoracic lymphadenopathy are particularly diverse and include a broad range of infectious, inflammatory, and malignant processes.
Unilateral hilar lymphadenopathy can be seen in inflammatory pneumonitis; infections such as bacterial pneumonia, tuberculosis, and atypical mycobacterial infection; pertussis; or granulomatous diseases such as fungal infections (eg, histoplasmosis or coccidioidomycosis) and sarcoidosis; less common infections such as tularemia or psittacosis should be considered in the appropriate clinical setting. Malignant causes of hilar adenopathy include lung cancer, breast cancer, metastases from the gastrointestinal tract, or involvement by Hodgkin or non-Hodgkin lymphoma.
Bilateral hilar lymphadenopathy can be caused by Hodgkin and non-Hodgkin lymphoma, chronic granulomatous disease (sarcoidosis, berylliosis), or metastatic cancer from a wide variety of primary sites. Calcified hilar lymphadenopathy is seen in tuberculosis, silicosis, sarcoidosis, and histoplasmosis.
Mediastinal lymphadenopathy also occurs in a variety of conditions ranging from infectious to malignant, and the differential diagnosis overlaps with that of hilar adenopathy.
Abdominal or Retroperitoneal Lymphadenopathy
Enlargement lymph nodes in the abdomen or retroperitoneum, including periportal, celiac, mesenteric, iliac, and periaortic node clusters, is a recurrent finding during abdominal imaging and is often worrisome for underlying malignancy. Limits on upper limits of normal size for abdominal lymph nodes have been proposed. An abnormal lymph node in the umbilical region (“pants button umbilicus,” also called the Sister Mary Joseph node, named after surgeon William Mayo’s surgical scrub nurse in the 1920s and 1930s at Mayo Clinic in Minnesota) can be associated with intra-abdominal or pelvic malignancy.
Epitrochlear Lymphadenopathy
Epitrochlear adenopathy is less well studied than adenopathy in other nodal groups. In one series of 184 consecutive patients with diseases in which lymphadenopathy occurs, 27% of patients had palpable epitrochlear lymph nodes, compared with 140 healthy controls, all of who did not have palpable epitrochlear lymphadenopathy. In that series, patients with epitrochlear lymphadenopathy in the setting of lymph node enlargement in other regions were most commonly found to have non-Hodgkin lymphoma, CLL, or infections, including human immunodeficiency virus (HIV) infection. Other causes included connective tissue disorders and sarcoidosis.
Popliteal Lymphadenopathy
Popliteal lymph nodes drain the lower extremities and may be a sign of an infection of the heel or foot. Only scarce data are available specifically about popliteal lymphadenopathy. Popliteal swelling due to a Baker cyst or an aneurysm or other vascular disorder is sometimes confused with adenopathy.
Inguinal Lymphadenopathy
Because of the chronic colonization of the anogenital region by bacteria, a small amount of reactive lymphadenopathy in the inguinal/femoral region is not necessarily pathologic and appears commonly in healthy populations. However, inguinal lymphadenopathy can be caused by sexually transmitted diseases, as well as cellulitis, including pedal dermatophytosis. Among metastatic lesions, inguinal metastases can be seen in cancers of skin of the lower extremities, cervix, vulva, skin of the trunk, mucosal surfaces of the rectum and anus, or the ovary or penis. Terminology of inguinal region nodes in the medical literature is inconsistent, with some investigators referring to femoral nodes as those below the inguinal ligament (eg, the node of Cloquet) and inguinal nodes as those above the inguinal ligament, whereas others using less precise terms such as vertical or horizontal nodes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree