inconsistency between studies may be partially attributed to small sample sizes, different time points of blood collection, different types of coagulation tests used, and different patient populations.
Table 84.1 Risk factors for UEDVT | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 84.2 Prevalence (%) of acquired and inherited thrombophilia in patients with UEDVT | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
usual symptoms of UEDVT are extremity edema, discomfort, and erythema.13 Patients with coexisting PE may also have dyspnea, chest pain, or cough.33
Table 84.3 Advantages and disadvantages of imaging modalities used to diagnose UEDVT | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Low-molecular-weight heparin (LMWH) is a safe and effective alternative and may reduce the duration of hospitalization.91 Typically, heparin is used as a “bridge” to warfarin therapy, which is continued for a minimum of 3 months with an international normalized ratio of 2.0 to 3.0.9,59,92 A longer duration of anticoagulation may be appropriate if there is an underlying hypercoagulable state.63,93,94
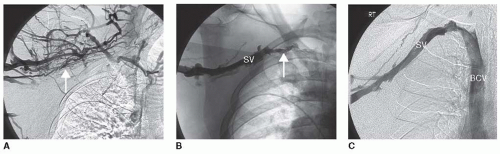
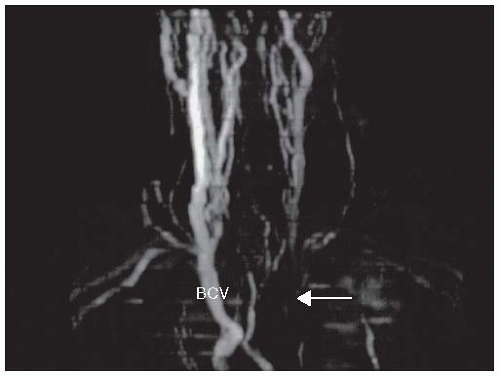 FIGURE 84.2 MRA demonstrating left BCV (arrow). (Adapted from Joffe HV, Goldhaber SZ. Upper-extremity deep vein thrombosis. Circulation 2002;106(14):1874-1880.) |
followed by prompt surgical correction, such as resection of bone or lysis of dense, perivascular adhesions.12,17,59,104,114,115,116,117,118 Persistent strictures after surgery could be treated with venoplasty and possibly vein stenting.119,120 This multimodal approach can successfully achieve long-term vessel patency.7,16,17,99,120,121,122,123 Although surgical thrombectomy restores venous patency, this approach is considered as a last resort because it is invasive, requires general anesthesia, and may be complicated by pneumothorax and brachial plexus damage.59 Conservative therapy rather than prompt surgical intervention may be preferable for selected patients with the thoracic outlet syndrome because physical therapy, weight loss, and nonsteroidal anti-inflammatory medications may avert the need for surgery.15
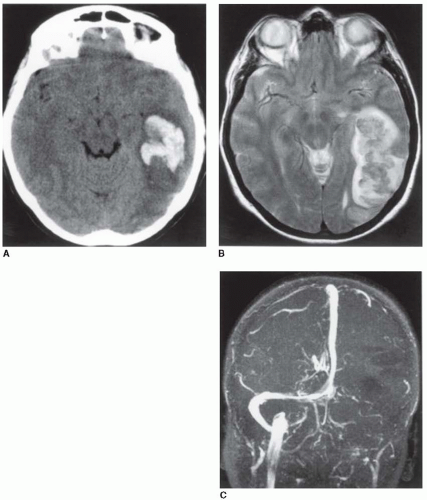
have no identifiable cause or are associated with head trauma, oral contraceptive (OC) usage, pregnancy or the puerperium, cachexia, dehydration, local malignancy, arteriovenous malformations, or other causes of generalized hypercoagulability. CVST is a well-recognized manifestation of the inherited and acquired thrombophilias, complicating virtually all of the known causes.142,143,144,145,146 Of note is the danger of cerebral vein thrombosis in patients with a hereditary predisposition who have been prescribed OC agents8 and in patients with paroxysmal nocturnal hemoglobinuria (PNH), antiphospholipid syndrome, and myeloproliferative disorders.147,148,149,150 Following thrombus formation in a venous sinus, increased venous pressure leads to cerebral edema and even hemorrhage (FIGURE 84.5), a process that may progress to the development of large and/or multiple venous infarctions, which cross the normal boundaries of arterial supply.151
seizure as an early manifestation, associated with supratentorial thrombotic lesions (OR = 3.0). Headache in combination with papilledema and absent focal neurologic signs can simulate brain tumor (“pseudotumor cerebri”).155 Nausea, vomiting, and mental confusion develop over hours to days, followed in the most severe cases by stupor and coma, but focal sensory or motor losses are not dominant features, and the cerebrospinal fluid and the electroencephalogram may show only nonspecific findings. Fever will usually accompany sinusitis or other infection that leads to direct extension of the process into a contiguous (e.g., cavernous) sinus. Diagnosis is established by magnetic resonance (MR) or computerized tomography (CT) venography,141,156,157,158,159 which documents the important contribution of “cytotoxic edema” in the pathogenesis of cerebral venous infarction.160 D-Dimer levels have been noted to be elevated, in correlation with the degree of thrombosis, and it is unlikely that an acute thrombotic event exists in the face of a normal D-dimer value.161 Predictors of adverse outcomes (death, dependency) are age >37 years, coma, intracranial hemorrhage, central nervous system infection, or malignant disease.162
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree